Safe Management of the COVID-19 Health Emergency: The Experience of the OORR Area Nolana of ASL NA3 Sud
by Giovanna Sepe1*, Giovanni Cirillo2
1Direzione Sanitaria OO.RR. Area Nolana, ASL NA3 Sud
2Department of Mental and Physical Health and Preventive Medicine, University of Campania “Luigi Vanvitelli, Naples, Italy
*Corresponding author: Dr. Giovanna Sepe, Direzione Sanitaria OO.RR. Area Nolana, ASL NA3 Sud, Via Seminario, 80035 Nola (NA), Italy
Received Date: 28 November 2025
Accepted Date: 03 December 2025
Published Date: 05 December 2025
Citation: Sepe G, Cirillo G (2025) Safe Management of the COVID-19 Health Emergency: The Experience of the OORR Area Nolana of ASL NA3 Sud. Advs Prev Med Health Care 8: 1085. https://doi.org/10.29011/2688-996X.001085
Abstract
The SARS Cov-2 pandemic has induced necessary measures to contain infection and the reorganization of health services to safeguard the health of users and the safety of health professionals. We here present the hospital and territorial guidelines developed and adopted by the Strategic Management of the ASL NA3Sud during the pandemic. In the ASL NA3Sud area, specific infection prevention procedures have been implemented, ensuring the safety of users and health personnel, and guaranteeing essential health services. In the hospital setting, the creation of a specific emergency network has transformed the P.O. of Boscotrecase in the HUB, leaving ordinary activities and suspected COVID-19 cases in triage and isolation courses to the other hospitals of the ASL NA3Sud (SPOKE). These measures have allowed to face health emergency by protecting the health and safety of health professionals and patients and ensuring, through the integration of hospital and territory, the essential health services.
Keywords: COVID-19; hospital/territorial guidelines; health and safety; HUB/SPOKE; ASL NA3 Sud Strategic Management; ergonomics.
Introduction
The rapid and widespread diffusion of the COVID-19 pandemic caused by the SARS-CoV-2 virus presented an unprecedented challenge to national healthcare systems, necessitating the urgent implementation of drastic infection containment strategies and extensive reorganization of healthcare services [1]. These actions were essential to ensure continuity of care for the population during the health emergency while simultaneously preserving the health, safety, and well-being of healthcare professionals, who were directly and continuously exposed to biological risks.
In Italy, as in other affected countries, the pandemic significantly disrupted the delivery of ordinary medical services [2,3]. Public and accredited private healthcare providers were required to rapidly shift their operational models, reconfigure their infrastructures, and adopt novel organizational solutions to cope with the increased demand for care and to prevent healthcare system collapse. This included the reallocation of clinical personnel, suspension of nonurgent procedures, conversion of hospital units into COVID-19 wards, and the implementation of triage systems capable of distinguishing between suspected COVID-19 cases and other urgent conditions.
The present paper aims to describe the strategic response implemented by ASL Napoli 3 Sud (Local Health Authority) during the COVID-19 emergency, with a specific focus on the integrated hospital and territorial healthcare network in the Nolan Area (Ospedali Riuniti Area Nolana- OORR, including the hospital facilities of Nola and Pollena Trocchia, province of Naples, Italy).
This experience represents a valuable model of organizational resilience, rapid adaptability, and coordinated action under extreme operational stress.
Concerning the hospital network, the Strategic Management of ASL Napoli 3 Sud undertook a comprehensive reorganization of all clinical and logistical activities. One of the most significant interventions was the delineation of differentiated pathways for emergency, urgent, and elective care, structured according to the HUB and SPOKE model. This system ensured that patients could receive the most appropriate care in the most suitable facility based on clinical complexity, resource availability, and regional epidemiological dynamics. Specifically, the Boscotrecase Hospital was designated as the central COVID-19 HUB and underwent a complete functional conversion. A total of 96 dedicated beds were made available, distributed across sub-intensive care (32), general surgery (14), internal medicine (30), cardiology (14), and intensive care (6). This concentration of COVID-19 resources allowed the remaining hospital sites in the ASL (the SPOKE centers) to continue delivering routine care and to manage suspected COVID-19 cases via separate triage and isolation routes. Confirmed cases were stabilized and subsequently transferred to the HUB facility, ensuring efficient allocation of resources and minimizing the risk of nosocomial transmission.
In parallel, substantial efforts were made at the territorial level. The Strategic Management of ASL Napoli 3 Sud promptly issued and implemented specific protocols aimed at containing community transmission and preserving essential services. A central element of this strategy was the establishment and operational deployment of special units for continuing assistance (USCA), responsible for home monitoring and follow-up of asymptomatic or mildly symptomatic COVID-positive patients, thereby reducing unnecessary hospital admissions and preventing overloading of emergency departments.
Additional measures included the adoption of structured procedures for healthcare worker protection, such as standardized donning and doffing protocols, mandatory use of personal protective equipment (PPE), systematic sanitization of clinical and administrative environments, and flexible work arrangements such as remote working, wherever applicable. Diagnostic testing protocols were also enhanced through widespread use of nasopharyngeal swabs and serological screening.
To maintain continuity of care for chronic and vulnerable patients, telemedicine solutions were activated, with particular emphasis on endocrinology and diabetology services. These digital pathways enabled remote consultations, monitoring of clinical parameters, and medication management, ensuring that patients with long-term conditions remained in contact with healthcare providers during lockdown periods. The integration of hospital and territorial care systems proved to be a critical factor in the resilience of the healthcare network. The coordinated approach adopted by ASL NA3 Sud was characterized by rapid decisionmaking, multidisciplinary collaboration, and a shared governance model that involved clinicians, administrative staff, public health officials, and support services.
The aim of this paper is to present and critically analyse the emergency response model implemented in the OORR Area Nolana under the coordination of ASL Napoli 3 Sud, as a concrete example of how an integrated healthcare system can adapt to an epidemiological crisis. By illustrating the strategies adopted, such as the effective reallocation of hospital resources, the activation of territorial care units, the strategic implementation of telemedicine services, and the rigorous enforcement of infection prevention protocols, this work seeks to highlight the organizational measures that allowed the health authority to mitigate the impact of the pandemic. Ultimately, the model ensured continuity of care and safeguarded both patients and healthcare professionals, offering a replicable approach for future public health emergencies.
Specific Procedures
In response to the official directives issued by ASL Napoli 3 Sud, the OORR Area Nolana implemented a comprehensive series of general and specific interventions, with the primary objective of containing the spread of the SARS-CoV-2 virus and reducing the incidence of new infections. These actions were developed in accordance with national and regional guidelines and were adapted to the specific organizational and logistical context of the hospital facilities involved.
Among the key containment measures, differentiated procedures and dedicated pathways were introduced for the reception, triage, and isolation of suspected or confirmed COVID-19 cases. This reorganization included the installation of external tent structures adjacent to the hospital buildings, which served as initial screening areas to separate potentially infected patients from the general hospital population, thus limiting the risk of in-hospital transmission.
To ensure the highest possible safety standards for both patients and healthcare professionals, a series of strict protocols were enacted. These included standardized procedures for the donning and doffing of personal protective equipment (PPE), thorough cleaning and environmental sanitization protocols, and staff training programs aimed at reinforcing correct behaviours and minimizing errors during high-risk operations. Emphasis was placed on the adoption of an ergonomic approach to emergency management, addressing the physical, cognitive, and organizational dimensions of healthcare work under pandemic conditions.
From a physical ergonomics perspective, attention was given to the interaction between healthcare personnel and their working environment, which had been profoundly altered by the pandemic context. Nurses and support staff working in COVIDdedicated areas were frequently engaged in physically demanding and repetitive activities, including the manual handling and repositioning of non-collaborative or immobilized patients. To prevent musculoskeletal disorders and reduce operator fatigue, training sessions were organized on proper handling techniques, and healthcare workers were instructed on the correct use of mechanical aids already available in the wards (e.g., patient lifters, transfer boards).
Additional ergonomic adaptations were made to prevent prolonged or incorrect postures. Height-adjustable chairs with high and adjustable backrests, ergonomic stools, and cushions were distributed to staff involved in static tasks, such as office personnel working for extended periods in a seated position, laboratory technicians processing nasopharyngeal swabs (typically performed in standing and semi-bent positions), and ambulance drivers responsible for patient transfers between SPOKE centers and HUB hospitals.
The physical spaces dedicated to donning and doffing procedures were identified among pre-existing areas and, when necessary, were adapted through urgent renovation works to meet the safety requirements defined by occupational health regulations. To further mitigate the risk of cross-contamination, external containers with climate control and hygienic amenities were employed for the execution of nasopharyngeal testing.
Another critical aspect addressed was the issue of microclimate and thermal comfort, particularly for staff wearing high-level PPE (including FFP2 respirators, full-face shields, goggles, impermeable gowns, and gloves) during physically intensive tasks. The exposure time, intensity, and number of personnel involved were minimized by introducing rotating shifts, with a strict limit of three consecutive hours of exposure in highrisk zones. Cognitive and organizational ergonomics were also integrated into the emergency response strategy. Workflows and decision-making processes were redesigned to enhance cognitive interaction between healthcare workers and information systems. Attention was paid to perception, attention, memory, and emotional load during task execution. Specific protocols were established to reduce human error, and some departments were equipped with intuitive, next-generation electro medical equipment designed to support rapid decision-making and reduce cognitive fatigue.
Lastly, a structured occupational health surveillance protocol was activated, allowing continuous monitoring of all hospital staff through periodic nasopharyngeal swab tests and monthly or weekly serological screening for SARS-CoV-2, enabling early identification of infected individuals and helping to control intrahospital outbreaks.
Results
One of the main strengths of the organizational model implemented by ASL Napoli 3 Sud in response to the COVID-19 health emergency was the prompt establishment of a dedicated Corporate Crisis Unit. This unit was composed of the Strategic Management Team and several key organizational figures, including the heads of the Clinical Risk Unit and the Hospital Functions Management Unit. Also involved were the Directors of the various Hospital Facilities, the Directors of Healthcare Departments and Districts, the Heads of Primary Care and Continuity of Care, the Director of Emergency Medical Services (118), and the Heads of the Pharmaceutical Service, Procurement Office, and Clinical Engineering Department.
This coordinated and multidisciplinary structure enabled a unified and rapid response to the unfolding crisis. Each stakeholder contributed their specific expertise and organizational knowledge, facilitating the development and operationalization of a flexible, scalable, and responsive model of emergency healthcare management within ASL Napoli 3 Sud.
The distribution of roles and clear definition of responsibilities allowed for an effective division of labour and ensured active participation across all levels of the healthcare system. This collaborative approach strengthened the resilience of both hospital and territorial services, enabling them to support the National Health Service even under extreme stress. Despite the temporary suspension of elective procedures, essential and urgent care was preserved for patients with chronic conditions-particularly those with diabetes, cancer, or cardiovascular disease-through the creation of prioritized and safe care pathways. The activation of a dedicated COVID-19 molecular diagnostics laboratory within the ASL NA3 Sud territory proved to be a critical factor in accelerating diagnostic workflows. The presence of this facility significantly reduced turnaround times for test results, enabling faster identification of positive cases, timely initiation of isolation protocols, and prompt clinical decision-making. This greatly improved the efficiency of both hospital admissions and territorial surveillance programs.
From March 2020 to October 2021, the Nola Hospital alone managed approximately 790 confirmed COVID-positive cases, all of which were stabilized and transferred to the designated HUB hospitals. During the same observation period, emergency room access remained high despite the pandemic context. Approximately 50,300 non-COVID emergency visits were recorded, including paediatric, obstetric, and orthopaedic cases, all managed through segregated care pathways Figure 1.
Figure 1: Hospital activity during the COVID-19 emergency. Overview of hospital activity at the OORR Area Nolana (ASL NA3 Sud) during the COVID-19 emergency. Between March 2020 and October 2021, the hospital managed 790 confirmed COVID-19 cases (stabilized and transferred to HUB centers) and maintained substantial non-COVID operations, including 50,300 emergency visits, 7,830 urgent non-COVID admissions, 744 cardiovascular emergencies, 830 childbirths, 2,079 emergency surgical procedures, and 383 orthopaedic/trauma surgeries.
In addition, the hospital reported 7,830 non-COVID urgent hospitalizations, including 744 admissions for acute cardiovascular events, 830 childbirths, 2,079 emergency surgical procedures, and 383 orthopaedic and trauma surgeries. A key element in preventing the collapse of the hospital emergency system was the deployment of USCA (Special Continuity Assistance Units) across the ASL Napoli 3 Sud territory. These mobile units provided home-based care and clinical monitoring for COVID-positive but asymptomatic or mildly symptomatic patients, reducing unnecessary hospital visits and preventing the saturation of emergency departments. The USCA teams played a vital role in maintaining continuity of care while safeguarding hospital capacity for more severe cases.
To ensure the safety and well-being of healthcare workerswho represented the most exposed population segment during the pandemic-occupational health surveillance protocols were significantly strengthened. In total, 5,512 nasopharyngeal swabs were performed for healthcare staff, alongside 600 occupational medical evaluations Figure 2.
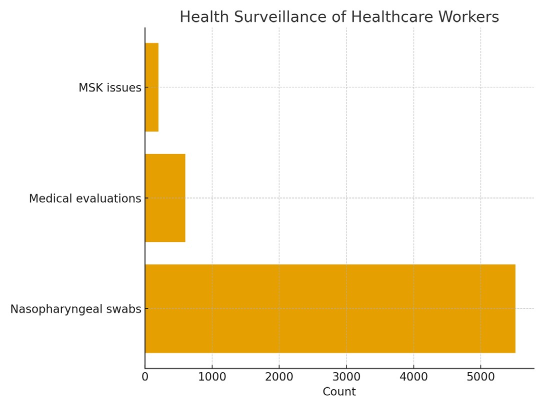
Figure 2: Health surveillance of healthcare workers. Occupational health surveillance activities performed for healthcare workers during the pandemic. A total of 5,512 nasopharyngeal swabs and 600 medical evaluations were conducted. Approximately 200 workers reported musculoskeletal disorders related to physical overload, prolonged PPE use, and altered ergonomics in COVIDdedicated areas.
Workers identified as clinically fragile were temporarily excluded from COVID-19 care pathways. When suitable alternative tasks could not be assigned, remote working arrangements were authorized to preserve workforce participation while mitigating individual risk. Attention was given to healthcare personnel with high exposure to biological hazards (e.g., staff in COVID wards, ambulance crews, swab collection teams) and to those frequently engaged in physically demanding tasks such as the manual handling of non-cooperative patients. These workers were subjected to more frequent clinical monitoring and targeted preventive measures. Approximately 200 healthcare workers reported musculoskeletal issues such as lower back pain and generalized muscle fatigue, symptoms often associated with improper postures, prolonged workloads, and the use of PPE in high-temperature settings.
In addition to physical health, the psychological impact of the pandemic on healthcare personnel was closely monitored Figure 3.
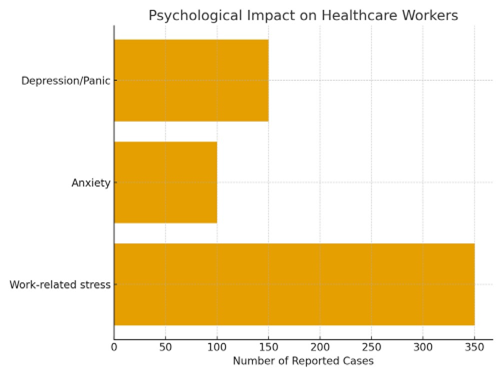
Figure 3: Psychological impact on healthcare workers. Mental health outcomes reported among healthcare personnel during the pandemic. The occupational health monitoring program recorded 350 cases of work-related stress, 100 cases of clinically significant anxiety, and 150 cases of depressive symptoms or panic attacks, highlighting the considerable psychological burden associated with high-risk clinical environments.
The constant exposure to critical and high-pressure scenarios, combined with social isolation and emotional exhaustion, led to a rise in stress-related conditions. Specifically, 350 cases of workrelated stress, 100 cases of clinically significant anxiety, and 150 cases of depressive symptoms or panic attacks were documented. In response, psychological counselling and mental health support services were made available through a dedicated program activated by the Health Management Unit.
Overall, these data demonstrate that the model adopted by ASL Napoli 3 Sud not only sustained core healthcare operations during the acute phase of the pandemic but also succeeded in proactively addressing the needs of both patients and healthcare workers. The systematic integration of hospital-based and territorial interventions, combined with constant clinical monitoring and psychological support, contributed to the overall effectiveness and sustainability of the emergency response system.
Discussion
The COVID-19 pandemic presented an unprecedented challenge to healthcare systems worldwide, requiring not only a massive mobilization of resources but also the rapid restructuring of care delivery processes [4]. In this context, the organizational strategy developed and implemented by ASL Napoli 3 Sud proved to be both effective and adaptable, allowing for a comprehensive response to the health emergency. The approach adopted ensured the safety of both patients and healthcare workers through a multidimensional strategy that integrated clinical, logistical, organizational, and ergonomic considerations.
A central element of this model was the emphasis on ergonomics at every operational level (physical, cognitive, and organizational) which contributed significantly to risk mitigation and performance optimization during the most critical phases of the pandemic [5]. For patients and healthcare users, the model entailed a necessary and substantial redefinition of healthcare services, both at the hospital and territorial level. This redefinition led to the establishment of interoperable care pathways and facilitated a more dynamic and functional integration between hospital-based and communitybased services. Such integration proved crucial for maintaining continuity of care during lockdowns and for managing both COVID-19 and non-COVID-19 patients in parallel.
The strategic coordination between hospital and territorial services was not simply an operational necessity but a structural innovation. The establishment of a clearly defined hospital-territory network allowed ASL Napoli 3 Sud to control the risk of intra- and intercommunity viral transmission more effectively. This structure enabled the reduction of COVID-19-related morbidity and mortality and helped contain the impact of the epidemic on healthcare and social services by protecting the most vulnerable segments of the population while maintaining access to essential medical services. Without such systemic integration, the healthcare infrastructure would likely have experienced operational overload, with potentially severe consequences for both acute and chronic care delivery.
Throughout the emergency period, all care processes were supported by robust interconnections between various institutional and clinical stakeholders. The synergistic collaboration among healthcare management, clinical staff, territorial units, administrative bodies, and technical services, under the leadership of the Strategic Management Team, enabled a shared governance framework. This participatory coordination model promoted flexibility, responsiveness, and the continuous reevaluation of care protocols in light of evolving epidemiological data and operational feedback. For healthcare professionals, the implemented measures had a dual protective function: on the one hand, they aimed to mitigate biological risk, particularly the risk associated with exposure to SARS-CoV-2 through patient contact and contaminated environments; on the other, they addressed occupational hazards related to workload, ergonomics, and psychosocial stress. The health surveillance protocols enacted played a pivotal role in identifying workers at higher risk and allowed for preventive and corrective interventions, including reassignment of tasks, activation of remote working modalities, and periodic medical evaluations for personnel engaged in highexposure or high-strain duties [6].
The ergonomic approach was especially valuable. By evaluating and improving the interaction between healthcare workers and their work environments, including the use of personal protective equipment (PPE), the handling of patients and materials, and the organization of clinical workflows, ASL Napoli 3 Sud was able to significantly reduce the risk of work-related injuries and fatigue [7]. This included musculoskeletal problems and physical overload, as well as cognitive fatigue and decision-making errors, which are particularly dangerous during high-pressure medical interventions. Cognitive ergonomics also contributed to the development of intuitive protocols and the adoption of userfriendly technologies, minimizing training time and reducing error margins during complex tasks.
However, despite these successes, several structural limitations emerged during the response phase. Chief among these was the need to manage the pandemic within pre-existing hospital infrastructures. Most of the healthcare facilities involved were not originally designed to accommodate the type of functional and spatial flexibility required during an infectious disease outbreak of this magnitude. As a result, significant efforts had to be invested in adapting physical spaces, redistributing resources, and re-engineering workflows. This included the reorganization of hospital beds to dedicate entire wards to COVID-positive patients, often at the expense of other specialties, as well as the creation of physically separate emergency departments for COVID and non-COVID patients. These adjustments, while effective, imposed considerable strain on personnel and required constant logistical support and reallocation of clinical competencies.
Over time, as the epidemiological picture evolved, the clinical presentation of COVID-19 also changed. In the more recent phases of the pandemic, particularly after the introduction of vaccination campaigns and the emergence of less severe viral variants, SARS-CoV-2 infections have increasingly been detected incidentally, especially in patients accessing healthcare services for unrelated reasons [9,10]. Despite this apparent attenuation in disease severity, the gradual yet steady increase in healthcare demand has created new organizational challenges. The return to “normal” service volumes has necessitated careful planning to avoid new clusters of infection within hospital settings, especially in departments treating immunocompromised or fragile patients. As a result, hospital management teams are now faced with the complex task of maintaining pandemic preparedness measures while restoring full-service provision across all departments. This dual objective requires the continued adoption of infection control protocols, real-time surveillance systems, contingency planning, and ergonomic principles that enhance resilience without compromising efficiency or quality of care.
In conclusion, the case of ASL Napoli 3 Sud demonstrates that an integrated, multidisciplinary, and ergonomically-informed emergency management model can provide an effective and sustainable response to public health crises. By leveraging the synergies between hospital and territorial systems, investing in staff safety and training, and maintaining a high level of organizational adaptability, it was possible to manage the COVID-19 emergency without sacrificing the delivery of essential healthcare services. The lessons learned through this experience should inform future policy development and serve as a framework for institutional readiness in the face of future pandemics or large-scale emergencies. Moreover, the application of ergonomic methodologies in the context of healthcare emergencies emerges not only as a protective factor for workers but also as a strategic lever for ensuring the quality, safety, and continuity of care in the most complex and unpredictable scenarios.
However, this study is not without limitations. First and foremost, the findings presented are based on a single territorial and hospital network experience (OORR Area Nolana–ASL Napoli 3 Sud), which may limit the generalizability of the model to other healthcare contexts with different structural, demographic, or epidemiological characteristics. Secondly, the analysis primarily relied on retrospective organizational and clinical data, whichalthough valuable-may lack granularity in capturing the subjective experiences of frontline staff and patients. The absence of a formal quantitative evaluation of ergonomic interventions (e.g., pre- and post-intervention risk assessments or biomechanical workload indices) also represents a constraint, as the benefits described are based largely on observed outcomes and operational feedback rather than systematic measurement. Furthermore, while psychological support services were activated and accessed by a significant number of healthcare workers, no formal psychometric assessments were administered to evaluate the long-term mental health impacts of the pandemic on staff well-being.
Future studies should aim to complement these findings with multicenter comparative analyses, incorporate prospective evaluation methods, and integrate patient-reported outcomes and healthcare worker satisfaction metrics. Despite these limitations, the present study offers a robust descriptive framework and a practical reference for healthcare system reorganization in times of epidemiological crisis.
References
- Kraus M, Stegner C, Reiss M, Riedel M, Børsch AS, et al. (2025) Management of Hospital Care during the COVID-19 Pandemic: Lessons Learnt from Five European Countries. SSM-Health Systems. 4: 100050.
- Sabaa-Ayoun Z (2021) Restructuring of Healthcare System in Italy during COVID-19. Univ West Ont Med J
- Parotto E, Lamberti-Castronuovo A, Censi V, Valente M, Atzori A, et al. (2023) Exploring Italian Healthcare Facilities Response to COVID-19 Pandemic: Lessons Learned from the Italian Response to COVID-19 Initiative. Front Public Health 9:1016649.
- Filip R, Gheorghita Puscaselu R, Anchidin-Norocel L, Dimian M, Savage WK (2022) Global Challenges to Public Health Care Systems during the COVID-19 Pandemic: A Review of Pandemic Measures and Problems. J Pers Med 12: 1295.
- Boatca ME, Draghici A, Robescu D (2022) Conception of Ergonomic Interventions and Challenges during Covid-19 Pandemic. Saf Health Work 13: S195-S196.
- Sakowski P, Marcinkiewicz A (2018) Health Promotion and Prevention in Occupational Health Systems in Europe. Int J Occup Med Environ Health 32: 353-361.
- Rodríguez Y, Hignett S (2021) Integration of Human Factors/ Ergonomics in Healthcare Systems: A Giant Leap in Safety as a Key Strategy during Covid‐19. Human Factors and Ergonomics in Manufacturing & Service Industries. 31: 570-576.
- Della Torre V, Nacul FE, Rosseel P, Baid H, Bhowmick K, et al. (2021) Human Factors and Ergonomics to Improve Performance in Intensive Care Units during the COVID-19 Pandemic. Anaesthesiol Intensive Ther 53: 265-270.
- Gabutti G, d’Anchera E, De Motoli F, Savio M, Stefanati A (2021) The Epidemiological Characteristics of the COVID-19 Pandemic in Europe: Focus on Italy. Int J Environ Res Public Health 18: 2942.
- Are EB, Song Y, Stockdale JE, Tupper P, Colijn C (2023) COVID-19 Endgame: From Pandemic to Endemic? Vaccination, Reopening and Evolution in Low- and High-Vaccinated Populations. J Theor Biol 21: 111368.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.