Research Status and Influencing Factors of Postoperative Sore Throat in Patients Undergoing General Anesthesia Surgery
by Ying Long, Nan Chen, Zemin Zhan*, Miaoe Lu, Yi Wu
Nursing Department, Nansha Division, The First Affiliated Hospital, Sun Yat-sen University, Guangdong 511400, China
*Corresponding author: Zemin Zhan, Nursing Department, Nansha Division, The First Affiliated Hospital, Sun Yat-sen University, Guangdong 511400, China
Received Date: 15 August 2025
Accepted Date: 23 August, 2025
Published Date: 27 August, 2025
Citation: Long Y, Chen N, Zhan Z, Lu M, Wu Y (2025) Research Status and Influencing Factors of Postoperative Sore Throat in Patients Undergoing General Anesthesia Surgery. Int J Nurs Health Care Res 8:1663. DOI: https://doi.org/10.29011/2688-9501.101663
Abstract
Objective: To analyze the influencing factors of postoperative sore throat in patients undergoing general anesthesia surgery, and provide reference for nursing intervention. Design: A cross-sectional, prospective, and descriptive study. Method: This study involved 271 patients who met the study’s eligibility criteria between January 2024 and June 2024. A self-made questionnaire, Hamilton Anxiety Scale, and visual analog scoring method were used to investigate 271 patients undergoing general anesthesia surgery in a tertiary hospital in Guangzhou, and the influencing factors of postoperative sore throat were analyzed. Result: The incidence of postoperative sore throat was 41.32% (112/271). Multivariate logistic regression analysis showed that 18-44 years old, Preoperative anxiety, and perioperative hypothermia are influencing factors for postoperative sore throat in patients undergoing general anesthesia surgery. Conclusion: The incidence of postoperative sore throat in patients undergoing general anesthesia surgery is relatively high. The influencing factors of postoperative sore throat are 18-44 years old, preoperative anxiety, and perioperative hypothermia.
Keywords: General Anesthesia Surgery; Postoperative Sore Throat; Influencing Factors
Introduction
Postoperative sore throat (POST) is one of the most common complications following the removal of the endotracheal tube after general anesthesia. Research indicates that the incidence of POST in patients under general anesthesia ranges from 21% to 70% [1]. The prolonged intubation during surgery can cause abrasion to the patient’s larynx, leading to laryngeal edema and pain. Patients often experience unbearable sore throat after the endotracheal tube is removed. Currently, there is no effective solution during the anesthesia recovery process, thus making the prevention of POST particularly important. Therefore, this study aims to assess the influencing factors of POST in order to prevent it, reduce the incidence of POST, and shorten the recovery time, thereby achieving comfortable nursing care, enhancing the patient’s medical experience, and improving medical satisfaction [2].
Materials and Methods
Design
This study was conducted as a cross-sectional, prospective descriptive study.
Study Setting and Sampling
This study was conducted in the Postoperative Recovery Room of the Nansha Division of The First Affiliated Hospital, Sun Yatsen University. The study population consisted of 355 patients. However, the study sample included only 271 patients because 34 patients were unable to respond coherently postoperatively, 16 patients could not cooperate due to postoperative delirium, 6 patients were transferred to the ICU after arriving in the recovery room, 9 patients experienced severe allergies in the recovery room, and 19 patients had incomplete data (Figure 1).
Inclusion and Exclusion Criteria
A convenience sampling method was employed to select postoperative patients who underwent general anesthesia in the anesthesia recovery room of a tertiary hospital in Guangzhou from January to June 2024 as the subjects of this study.
Inclusion Criteria
- All patients were over 18 years old and had good reading comprehension, language communication, and cognitive abilities;
- All patients voluntarily or according to medical advice accepted endotracheal intubation general anesthesia, rather than local or regional anesthesia;
- Patients with health conditions that might affect the results were typically excluded, such as those with severe complications or other diseases that affect the efficacy of anesthesia;
- Patients who were informed of their condition and consented to participated in this study.
- Patients with other preoperative laryngeal diseases and discomfort, such as vocal cord polyps, gastroesophageal reflux, etc.;
- Patients with severe mental or neurological diseases who could not cooperate to complete the survey;
- Allergies to specific drugs or adverse reactions in the history of anesthesia;
- Patients who needed to enter the ICU after surgery;
- Patients who were too weak to communicate;
- Patients who required reintubation;
- Patients who used double-lumen endotracheal tubes for intubation.
Exclusion Criteria
Instruments
The assessment tool was developed by the researchers through literature review and expert consultation. It is divided into two parts: general disease conditions and specialty-specific conditions. The general disease section includes factors such as type of surgery, age, gender, BMI, smoking history, surgical history, financial concerns, preoperative anxiety, cardiac function rating, airway rating, ASA classification, and whether hypothermia occurred during the perioperative period. The specialty-specific section includes factors such as whether the patient has a difficult airway, surgical position, intubation duration, number of suctioning episodes, number of coughing episodes, number of agitation episodes, whether there was delayed awakening, whether the endotracheal tube size was appropriate, use of steroid medications, and type of endotracheal tube [3-8].
Body Mass Index (BMI)
This is an indicator that measures the ratio of weight to height, used to assess whether the weight is within a normal range. The calculation formula is weight (in kilograms) divided by the square of height (in meters). Typically, a BMI value between 18.5 and 24 is considered within the normal range.
Cardiac Function Classification
It is divided into four grades. Grade I indicates no limitation of physical activity. Grade II indicates slight limitation of physical activity. Grade III indicates marked limitation of physical activity.
Grade IV indicates that any physical activity causes discomfort.
Airway Classification (Mallampati Grading)
It is divided into four grades, with higher grades generally indicating greater difficulty in intubation. Grade I: The soft palate, uvula, fauces, and hard palate are visible. Grade II: The soft palate, uvula, and hard palate are visible. Grade III: The soft palate and hard palate are visible. Grade IV: Only the hard palate is visible.
ASA Classification
It is divided into five grades. Grade I indicates a healthy individual. Grade II indicates mild or moderate systemic disease. Grade III indicates severe systemic disease with limitation of daily activities but without loss of working capacity. Grade IV indicates severe systemic disease with loss of working capacity. Grade V indicates critical illness.
Hamilton Anxiety Rating Scale (HAM-A)
The Hamilton Anxiety Rating Scale (HAM-A) is a clinical scale used to assess the severity of anxiety in individuals. It consists of 14 items that evaluate various anxiety symptoms, such as tension, fear, and muscle tension. Each item is scored on a scale of 0 to 4, with a total score ranging from 0 to 56. Higher scores indicate more severe anxiety symptoms. A total score above 29 indicates severe anxiety; above 21 indicates definite anxiety; above 14 indicates probable anxiety; and above 7 suggests possible anxiety. If the score is less than 6, the patient is considered to have no anxiety symptoms. In this study, HAMA scores of ≥7 were defined as anxiety. This scale is widely used in clinical assessments and research to determine the severity of anxiety [9].
Facial Visual Analogue Scale (F-VAS)
The Facial Visual Analogue Scale (F-VAS) was used to assess patients’ postoperative sore throat. The VAS is one of the most commonly used single-dimensional measurement tools for pain intensity. The scale primarily consists of a 100mm line, with one end representing ‘no pain at all’ and the other end representing ‘the most severe pain imaginable’ or ‘the worst pain possible’. Patients are asked to mark their pain level on this line, and any score above 0 indicates sore throat [10]. This method is sensitive, intuitive, simple to understand, and less influenced by other factors, making it widely used in clinical research.
Data Collection
One day before surgery, the researchers explained the purpose, methods, and significance of the study to the subjects and their families, obtaining their consent and support, and having them sign an informed consent form. The study involved asking patients about their basic medical history, the presence of preoperative sore throat, and the level of preoperative anxiety using a verbal questionnaire on the day before surgery. Patients with preoperative sore throat were excluded. The specialty-specific conditions were assessed on the day of surgery, and the patients’ sore throat was evaluated using the Facial Visual Analogue Scale (F-VAS) before they left the anesthesia recovery room after extubation. The study was conducted from January 2024 to June 2024.
Ethical Considerations
To conduct this study, approval was obtained from the Ethics Committee for Clinical Research and Animal Trials of the First Affiliated Hospital of Sun Yat-Sen University (approval number: [2023]844). Written and verbal informed consent was obtained from the participants. All data were collected anonymously and stored securely. The study was conducted in accordance with the ethical standards of the Declaration of Helsinki 2008.
Data Analysis
Descriptive, graphical, and statistical methods were employed to assess whether the scores obtained from each continuous variable followed a normal distribution. The Kolmogorov-Smirnov test was utilized to evaluate the normality of the scores derived from continuous variables using statistical methods. Categorical variables were presented as frequencies (n, %), while continuous variables were expressed as means and standard deviations. Independent samples t-tests were conducted to compare quantitative differences between independent groups. Multivariate logistic regression analysis was performed to identify independent variables associated with the dependent variable. The HosmerLemeshow test and Nagelkerke R² were used to assess the strength of the relationship between the dependent and independent variables and the goodness of fit of the regression model. Results were evaluated at a 95% confidence interval, with P-values less than 0.05 considered statistically significant. All statistical analyses were carried out using SPSS (Statistical Package for the Social Sciences) software version 26 (IBM Corp.).
Result
Description of the Sample
A total of 271 patients who underwent general anesthesia were divided into two groups based on the occurrence of postoperative sore throat: the postoperative sore throat group, with 112 cases (41.33%), and the non-postoperative sore throat group, with 159 cases (58.67%).
Univariate Analysis Findings
Univariate analysis of the impact of general and specialty conditions on the occurrence of postoperative sore throat is presented in Table 1. Age, preoperative anxiety, use of steroids, and perioperative hypothermia were found to have significant effects on the occurrence of postoperative sore throat in general anesthesia patients (P < 0.05) (Table 1).
|
Item |
Postoperative Sore Throat Group |
Non-postoperative Sore Throat Group(N=159) |
t |
P Value |
|
(N=112) |
||||
|
Gender |
0.959 |
0.327 |
||
|
Male |
45(40.2) |
74(46.5) |
||
|
Female |
67(59.8) |
85(53.5) |
||
|
Age |
12.66 |
0.005** |
||
|
18-44 |
56(50.0) |
57(35.8) |
||
|
45-59 |
30(26.8) |
43(27.0) |
||
|
60-74 |
24(21.4) |
53(33.3) |
||
|
75-90 |
2(1.8) |
6(3.8) |
||
|
BMI |
0.786 |
0.853 |
||
|
<18.5 |
6(5.4) |
13(8.2) |
||
|
≥18.5 |
52(46.4) |
83(52.2) |
||
|
≥24 |
37(33.0) |
40(25.2) |
||
|
≥27 |
17(15.2) |
23(14.5) |
||
|
Smoking and Alcohol History |
0.66 |
0.797 |
||
|
Yes |
15(13.4) |
19(11.9) |
||
|
No |
97(86.6) |
140(88.1) |
||
|
Operating history |
2.199 |
0.138 |
||
|
Yes |
67(59.8) |
100(62.9) |
||
|
No |
45(40.2) |
59(37.1) |
||
|
Financial Concerns |
1.518 |
0.218 |
||
|
Yes |
3(2.7) |
7(4.4) |
||
|
No |
109(97.3) |
152(95.6) |
||
|
Surgical Category |
1.626 |
0.471 |
||
|
Urology |
36(32.1) |
46(28.9) |
||
|
Gynecology |
19(17.0) |
28(17.6) |
||
|
Gastrointestinal |
12(10.7) |
30(18.9) |
||
|
Thyroid |
11(9.8) |
16(10.1) |
||
|
Breast |
6(5.4) |
8(5.0) |
||
|
Orthopedics |
15(13.4) |
22(13.8) |
|
Otorhinolaryngology |
13(11.6) |
5(3.1) |
||
|
Thoracic |
0(0.00) |
2(1.3) |
||
|
Burn |
0(0.00) |
2(1.3) |
||
|
Cardiac Function Classification |
0.059 |
0.808 |
||
|
Grade I |
88(78.6) |
120(75.5) |
||
|
Grade II |
24(21.4) |
39(24.5) |
||
|
Airway Classification |
2.739 |
0.434 |
||
|
Grade I |
62(55.4) |
91(57.2) |
||
|
Item |
Postoperative Sore Throat Group |
Non-postoperative Sore Throat Group(N=159) |
t |
P Value |
|
(N=112) |
||||
|
Grade II |
46(41.1) |
63(39.6) |
||
|
Grade III |
3(2.7) |
4(2.5) |
||
|
Grade IV |
1(0.9) |
1(0.6) |
||
|
ASA Classification |
1.508 |
0.68 |
||
|
Grade I |
8(7.1) |
8(5.0) |
||
|
Grade II |
80(71.4) |
103(64.8) |
||
|
Grade III |
23(20.5) |
48(30.2) |
||
|
Grade IV |
1(0.9) |
0(0.00) |
||
|
Difficult Airway |
0.127 |
0.721 |
||
|
Yes |
2(1.8) |
4(2.5) |
||
|
No |
110(98.2) |
155(97.5) |
||
|
Surgical Position |
3.226 |
0.199 |
||
|
Supine position |
98(87.5) |
138(86.8) |
||
|
Lateral Position |
8(7.1) |
6(3.8) |
||
|
Lithotomy Position |
6(5.4) |
15(9.4) |
||
|
Intubation Duration |
5.467 |
0.362 |
||
|
≤1h |
0(0.00) |
2(1.3) |
||
|
1h-1h30 |
25(22.3) |
34(21.4) |
||
|
1h30-2h |
39(34.8) |
47(29.6) |
|
2h-2h30 |
20(17.9) |
35(22.0) |
||
|
2h30-3h |
12(10.7) |
12(7.5) |
||
|
≥3h |
16(14.3) |
29(18.2) |
||
|
Cuff pressure difference |
-0.808 |
0.8 |
||
|
Normal |
15(13.4) |
28(17.6) |
||
|
-5~+5 |
42(37.5) |
56(35.2) |
||
|
-(5~10)~(5-10) |
16(14.3) |
24(15.1) |
||
|
≥10 |
39(34.8) |
51(32.1) |
||
|
Awakening peak ΔP |
-0.684 |
<0.001*** |
||
|
<5 |
25(22.3) |
15(9.4) |
||
|
5~10 |
8(7.1) |
17(10.7) |
||
|
10~15 |
12(10.7) |
52(32.7) |
||
|
15~20 |
17(15.2) |
39 (24.5) |
||
|
>20 |
50(44.6) |
36(22.6) |
||
|
Suctioning Frequency |
0.324 |
0.851 |
||
|
0 |
96(85.7) |
142(89.3) |
||
|
1 |
12(10.7) |
15(9.4) |
||
|
≥2 |
4(3.6) |
2(1.3) |
||
|
Item |
Postoperative Sore Throat Group |
Non-postoperative Sore Throat Group(N=159) |
t |
P Value |
|
(N=112) |
||||
|
Coughing Episodes |
3.64 |
0.457 |
||
|
0 |
64(57.1) |
107(67.3) |
||
|
1 |
25(22.3) |
29(18.2) |
||
|
2 |
10(8.9) |
11(6.9) |
||
|
3 |
9(8.0) |
8(5.0) |
||
|
≥4 |
4(3.6) |
4(2.5) |
||
|
Agitation Episodes |
0.141 |
0.998 |
||
|
0 |
98(87.5) |
143(89.9) |
||
|
1 |
6(5.4) |
8(5.0) |
||
|
2 |
3(2.7) |
7(4.4) |
||
|
3 |
3(2.7) |
1(0.6) |
||
|
≥4 |
2(1.8) |
0(0.00) |
||
|
Delayed emergence |
2.547 |
0.111 |
||
|
Yes |
3(2.7) |
1(0.6) |
||
|
No |
109(97.3) |
158(99.4) |
||
|
Use of Steroids |
5.009 |
0.025* |
||
|
Yes |
37(33.0) |
68(42.8) |
||
|
No |
75(67.0) |
91(57.2) |
||
|
Preoperative Anxiety |
7.073 |
0.008** |
||
|
Yes |
30(26.8) |
22(13.8) |
||
|
No |
82(73.2) |
137(86.2) |
||
|
Tracheal tube non - conformance |
-1.828 |
<0.001*** |
||
|
Yes |
8(7.1) |
4(2.5) |
||
|
No |
104(92.9) |
155(97.5) |
||
|
Catheter Type |
0.134 |
0.715 |
||
|
Standard Cuffed Tracheal Tube |
106(94.6) |
151(95.0) |
||
|
Reinforced Cuffed Tracheal Tube |
6(5.4) |
8(5.0) |
||
|
Perioperative Hypothermia |
6.246 |
<0.001*** |
||
|
Yes |
52(46.4) |
20(12.6) |
||
|
No |
60(53.6) |
139(87.4) |
ASA,American Society of Anesthesiologists;t,T-test *P<0.05, **P<0.01, ***P<0.001
Table 1: Univariate Analysis of Postoperative Sore Throat Occurrence in Patients under General Anesthesia. (N=271) [n(%)].
Multivariate Analysis Findings
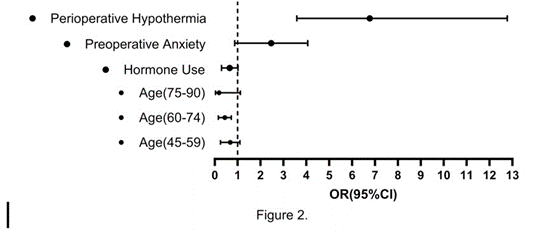
Multiple logistic regression model analysis with the enter method was applied to determine the independent variables associated with the occurrence of postoperative sore throat (POST) by using the variables found to be statistically significant in univariate analysis results. The Hosmer and Lemes how test (χ² = 6.411, P = .601) indicated that the model was appropriate for determining the variables associated with the formation of postoperative sore throat. According to the results of the logistic regression analysis, age between 18-44 years, preoperative anxiety, and Perioperative hypothermia were identified as influencing factors for postoperative sore throat. The presence of preoperative anxiety increased the probability of developing postoperative sore throat by 2.12 times (95% CI, 1.069 to 4.205), and the occurrence of perioperative hypothermia increased the probability of postoperative sore throat by 6.769 times (95% CI, 3.585 to 12.779) (Table 2) (Figure 2).
|
Item |
B |
SE |
Wald X2 |
OR (95%CI) |
P Value |
||
|
Age (with 74-90years as the control group) |
|||||||
|
18-44 |
-1.654 |
0.937 |
3.118 |
0.191(0.030-1.200) |
0.077 |
||
|
45-59 |
-1.078 |
0.944 |
1.305 |
0.340(0.054-2.163) |
0.253 |
||
|
60-74 |
-0.607 |
0.944 |
0.413 |
0.545(0.086-3.468) |
0.52 |
||
|
Coughing Episodes (with 4 as the control group) |
|||||||
|
0 |
0.448 |
0.758 |
0.35 |
1.566(0.354-6.919) |
0.554 |
||
|
1 |
-0.153 |
0.797 |
0.037 |
0.847(0.180-4.089) |
0.847 |
||
|
2 |
0.286 |
0.927 |
0.095 |
0.758 (0.216-8.185) |
0.758 |
||
|
3 |
-0.394 |
0.911 |
0.187 |
0.665 (0.113-4.022) |
0.665 |
||
|
Hormone Use (yes vs no) |
-0.562 |
0.296 |
3.604 |
0.570(0.319-1.018) |
0.058 |
||
|
Preoperative Anxiety (yes vs no) |
0.685 |
0.351 |
3.806 |
1.983(0.997-3.974) |
0.051 |
||
|
Perioperative Hypothermia (yes vs no) |
1.912 |
0.333 |
35.027 |
7.186(3.740-13.807) |
0.000*** |
B, regression coefficient; SE, standard error; OR, odds ratio; CI, confidence interval;
*P<0.05, **P<0.01, ***P<0.001
Table 2: Multivariate Analysis of Postoperative Sore Throat Occurrence in Patients under General Anesthesia(N=271).
Discussion
Postoperative sore throat (POST) is a common complication following the removal of an endotracheal tube after general anesthesia, characterized by congestion or edema of the throat. The incidence of POST varies internationally, ranging from 12.1% to 70% [1]. POST has been shown to impair the recovery after anesthesia and affect patient satisfaction during hospitalization [2]. Additionally, POST may lead to aspiration pneumonia. The mechanisms of POST include damage to epithelial and mucosal cells caused by airway secretions, as well as injury and congestive swelling of the vocal cords. Currently, there are no effective treatments, and POST typically resolves spontaneously within 3 to 4 days.
Analysis of Factors Influencing Postoperative Sore Throat After General Anesthesia
In this study, it was found that age between 18 and 44 years, preoperative anxiety, and perioperative hypothermia are significant risk factors for postoperative sore throat after general anesthesia. Yuta Mitobe’s [5] research indicates that personal factors contributing to postoperative sore throat include smoking history, female gender, and age. However, in this study, smoking history and gender were not identified as risk factors for postoperative sore throat. Experimental pain pressure threshold tests have shown that the intensity and unpleasantness of pain stimuli are significantly lower in older individuals compared to younger patients[11]. After studying changes in pain perception, Lauten bacher et al. [12] found that aging reduces pain sensitivity and intensity. These findings suggest that age is a factor in postoperative sore throat (POST). Yuta Mitobe’s [5] study also points out that pain is influenced by mental states such as anxiety, which varies from person to person. Patients often experience anxiety before surgery, which can increase the incidence of postoperative sore throat.
Anxiety can act as a stressor, triggering a series of psychological, endocrine, and immune changes. Individuals with anxiety are more sensitive to stimuli, making them more prone to postoperative redness and pain in the throat. In this study, preoperative anxiety was identified as a risk factor for postoperative sore throat in patients undergoing general anesthesia with endotracheal intubation, with the risk being 2.120 times higher for anxious patients compared to non-anxious patients (P < 0.05). Perioperative hypothermia is another significant risk factor for postoperative sore throat in this study. This phenomenon may be related to coagulation dysfunction, reduced local immune response, slowed metabolism of anesthetic drugs, extended postoperative recovery time, and shivering. Coagulation dysfunction: Hypothermia can reduce the activity of thrombin, decrease platelet release and aggregation, thereby affecting the hemostasis process [13].
This increases the risk of postoperative bleeding, which can lead to sore throat. Reduced local immune response: Hypothermia can lower local immune function, making the throat more susceptible to infection. Extended postoperative recovery time: Hypothermia slows the metabolism and elimination of anesthetic drugs, prolonging the patient’s recovery time [12]. This increases the duration of stimulation and compression from the endotracheal tube, thereby increasing the likelihood of sore throat. Shivering: Rapid rhythmic contractions of the skeletal muscles in the throat can pull on the wound, exacerbating sore throat [10]. These factors interact and collectively influence the occurrence and severity of postoperative sore throat. Christiansen P’s [14] research on tracheal tube size showed that the incidence of POST was significantly lower in women with a tube size of 6.0 compared to those with a size of 7.0, and in men with a size of 7.0 compared to those with a size of 8.0. This study suggests that smaller tube sizes can reduce postoperative throat pain and hoarseness after general anesthesia, but their safety still needs further investigation. In this study, tracheal tube size did not affect postoperative sore throat.
Prevention Measures for Postoperative Sore Throat After General Anesthesia
In the prevention of postoperative sore throat after general anesthesia, the first factor to consider is the patient’s age. For older patients, the action of endotracheal intubation should be more gentle to avoid frequent coughing after surgery, thereby reducing the friction between the pharyngeal mucosa and the tracheal cuff. Additionally, maintaining body temperature during the perioperative period is crucial. The room temperature for adult surgeries should not be lower than 21°C, and for pediatric surgeries, it should not be lower than 23°C. One hour before surgery, equipment such as warm air blowers and air-filled warming blankets can be used to preheat the operating table. Research has shown that using an intravenous fluid warmer to heat blood transfusions and infusions in a controlled clinical environment is safe and reliable [15], which helps to prevent body temperature drop caused by the infusion of refrigerated blood products. During surgical pauses, incisions should be covered with gauze moistened with 37°C saline to prevent heat loss from the skin. Postoperatively, patients should be warmed as soon as possible with a warm air blower to prevent the occurrence of postoperative sore throat. Laparoscopic surgery is more likely to cause postoperative hypothermia, so preoperative assessment of the type of surgery and appropriate warming measures should be taken [16].
Preoperative anxiety has been proven to increase the risk of postoperative sore throat in this study. Therefore, it is particularly important to assess the patient’s level of preoperative anxiety and intervene accordingly [17]. Specific measures include pharmacological and non-pharmacological interventions. For patients with moderate to severe anxiety, appropriate pharmacological intervention should be provided, while for those with mild anxiety, psychological therapy or cognitive-behavioural interventions can be used for prevention. Studies have shown that factors such as being female, younger age, not being retired, undergoing surgery for the first time in one’s life, higher surgical risk, and poor preoperative sleep are associated with a higher prevalence of preoperative anxiety. By addressing these factors in preoperative anxiety prevention, the incidence of postoperative sore throat can be effectively reduced.
Strengths and Limitations of the Work
We identified factors related to anesthesia techniques and patientrelated psychological factors, including preoperative anxiety of patients. However, these factors are not independent of each other and act together to cause POST. Yet, it is unclear how many of these factors act together to cause POST and whether the combination of these factors affects the severity and duration of POST. We also strictly controlled for bias in the aspect of postoperative extubation, but there may still be some other factors that cannot be controlled, such as the habits or seniority of the extubation personnel. Therefore, in this study, the factors related to postoperative extubation had little effect on postoperative sore throat.
Conclusion
The occurrence of postoperative sore throat (POST) is a multifactorial event. Patients undergoing surgery have unique risk factors at every stage of the perioperative period. In this study, the incidence of POST in surgical patients was 41.33%, which is highly concerning. Perioperative risk factors included age, preoperative anxiety, the use of steroid medications during surgery, and perioperative hypothermia. In multivariate analysis, variables significantly associated with the risk of POST were age, preoperative anxiety, and perioperative hypothermia. The majority of POST cases can be prevented through appropriate identification and reduction of risk factors. Healthcare organizations and perioperative nurses must understand the risk factors related to the occurrence of POST and develop strategies to prevent them. These findings may aid in the development of strategies to prevent the development of POST.
References
- Tsukamoto M, Taura S, Kadowaki S, Hitosugi T, Miki Y, et al. (2022) Risk Factors for Postoperative Sore Throat After Nasotracheal Intubation. Anesth Prog 69: 3-8.
- Mazzotta E, Soghomonyan S, Hu LQ (2023) Postoperative sore throat: prophylaxis and treatment. Front Pharmacol 14:1284071.
- Niu JY, Yang N, Yu JM (2022) Postoperative sore throat after laparoscopic surgery. Anaesthesia.77: 934.
- Cho HY, Yang SM, Jung CW, Cheun H, Park HP, et al. (2022) A randomised controlled trial of 7.5-mm and 7.0-mm tracheal tubes vs. 6.5-mm and 6.0-mm tracheal tubes for men and women during laparoscopic surgery. Anaesthesia. 77: 54-58.
- Mitobe Y, Yamaguchi Y, Baba Y, Yoshioka T, Nakagawa K, et al. (2022) A Literature Review of Factors Related to Postoperative Sore Throat. J Clin Med Res 14: 88-94.
- Christiansen P, Pedersen CH, Selter H, Odder L, Riisager JP, et al. (2021) How Does Tube Size Affect Patients’ Experiences of Postoperative Sore Throat and Hoarseness? A Randomised Controlled Blinded Study. J Clin Med 10: 5846.
- Higgins PP, Chung F, Mezei G (2002) Postoperative sore throat after ambulatory surgery. Br J Anaesth 88: 582-584.
- Clayton-Smith A, Bennett K, Alston RP, Adams G, Brown G, et al. (2015) A comparison of the efficacy and adverse effects of doublelumen endobronchial tubes and bronchial blockers in thoracic surgery: a systematic review and meta-analysis of randomized controlled trials. Journal of Cardiothoracic and Vascular Anesthesia. 29: 955-966.
- HAMILTON M (1959) The assessment of anxiety states by rating. Br J Med Psychol 32: 50-55.
- Lee JH, Kim SB, Lee W, Ki S, Kim MH, et al. (2017) Effects of topical dexamethasone in postoperative sore throat. Korean J Anesthesiol 70: 58-63.
- Petrini L, Matthiesen ST, Arendt-Nielsen L (2015) The effect of age and gender on pressure pain thresholds and suprathreshold stimuli. Perception. 44: 587-596.
- Lautenbacher S, Peters JH, Heesen M, Jennifer S, Kunz M (2017) Age changes in pain perception: A systematic-review and meta-analysis of age effects on pain and tolerance thresholds. Neurosci Biobehav Rev 75:104-113.
- Duong H, Patel G (2024) Hypothermia.
- Roxby D, Sobieraj-Teague M, Wielligh JV, Sinha R, Kuss B, et al. (2020) Warming blood prior to transfusion using latent heat. Emerg Med Australas 32: 604-610
- Shen C, He Y (2024) Intraoperative hypothermia in patients with laparoscopic surgery: Influencing factors and prevention strategies. Heliyon. 10: e31479.
- Wang R, Huang X, Wang Y, Akbari M (2022) Non-pharmacologic Approaches in Preoperative Anxiety, a Comprehensive Review. Front Public Health 10: 854673.
- Yu J, Zhang Y, Yu T, Mi W,Yao S, et al. (2022) Preoperative Anxiety in Chinese Adult Patients Undergoing Elective Surgeries: A Multicenter Cross-Sectional Study. World J Surg 46: 2927-2938.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.