Missed Appointments in Mental Health Services in Primary Health Care at Al Wazarat
by Nouf Aljunaidel, Renad Alsuwaylimi, Marwan Alhudaithi, Mostafa Kofi*
Family and Community Medicine Dept, Prince Sultan Military Medical City; Ministry of Defense Health Services, Riyadh, Saudi Arabia
*Corresponding author: Mostafa Kofi, Family and Community Medicine Dept, Prince Sultan Military Medical City, Ministry of Defense Health Services, Riyadh, Saudi Arabia
Received Date: 20 May 2025
Accepted Date: 28 May, 2025
Published Date: 30 May, 2025
Citation: Aljunaidel N, Alsuwelmy R, Alhedethy M, Kofi M (2025) Missed Appointments in Mental Health Services in Primary Health Care at Al Wazarat. Int J Nurs Health Care Res 8:1644. https://doi.org/10.29011/2688-9501.101644
Abstract
Background: Missed appointments in mental health clinics, particularly at Al Wazarat PHC, Riyadh, Saudi Arabia, significantly put the healthcare system at risk due to a lack of patient care and the waste of valuable time and resources. Similar non-attendance behavior all over the world demands an in-depth analysis of why people skip appointments to ensure the development of effective interventions. Methodology: This was done through a retrospective analysis of clinic performance reports and patient appointment data. The study included the time factor, which employed a retrospective analysis of clinic performance reports and patient appointment data from 2023 and 2024. The analysis of centered on the prevalence of appointments being missed for reasons such as demographic patterns and barriers to all possibilities in access. Results: The results show the need for focused activities to understand patient-specific difficulties, improve referral procedures, and make mental health services more accessible and acceptable to the public generally. Conclusion: The clinic can achieve reduced appointment non-adherence, improved patient outcomes, and the best use of mental health resources by overcoming these challenges.
Keywords: Missed appointments; Mental health; Primary Health Care (PHC); Riyadh, Saudi Arabia; No-shows; Patient attendance
Introduction
Missed appointments are an important matter in the healthcare industry, primarily in mental health clinics, where it could affect patients’ health and the overall efficiency of healthcare delivery. In our case, it is essential to assess the problem of missed meetings and the reasons behind them, more so following alarming statistics of mental health. Statistics show that the rate of missed appointments stands at between 24.8% - 58.1% in Riyadh [1], similar to the United States where a study indicated that up to 64% of psychiatric patients failed to attend their first appointment once discharged [2]. Further, comparative research from England shows that missed psychiatric appointments accounted for 19%, which was higher than the 11% of other appointments [2]. Missed appointments do not only affect the health of individual patients; they also create considerable pressure on the financial aspect of healthcare systems. It is estimated that the cost of no-shows for mental health appointments in the UK is about 100 billion pounds, while in the U.S the costs amount to about $340 billion [3]. This is further complicated by the fact that patients with specific chronic mental illnesses having a high likelihood of not keeping appointments, are at a high risk of dying, with some scholars indicating that the rate of dying is eight times greater for those who miss two or more appointments per year [2].
Moreover, the absence of follow-up appointments can cause the likelihood of prehospitalization and relapse among psychiatric patients to double [2]. Understanding the real reasons why patients miss their scheduled appointments is of utmost importance as it serves as the basis for developing evidence-based and effective interventions for addressing appointment non-attendance. Recent research strongly suggests that forgetfulness is one of the most common causes of people failing to attend their appointments, and there is a high success rate of sending appointment reminders via SMS leading to a sharp reduction in the number of patients that miss appointments, an assertion that is supported by [4] and his colleagues in the year 2022. The study goes ahead to identify some of the contributing factors that lead to missed appointments as previous non-attendance, long wait times for appointments as well as logistical problems, such as issues of transportation, as indicated by the works of [5], and [6]. Certain studies have shown, however, that patients dealing with mental health comorbidities have a higher chance of missing appointments because the ailments impair cognitive functions that cause lapses in memory and low motivation to attend appointments, according to the researchers [7].
Considering the high and disturbing rates of missed appointments in mental health clinics, especially in the clinic, an examination into specific, targeted research that seeks to discover modifiable factors that may be positively changed to influence non-attendance is urgently required. This has caused a significant gap in the literature which needs to be filled through research that focuses specifically on the case of Saudi Arabia, as the current available data is scarce and incomplete. By ascertaining the specific percentage of missed appointments as well as the main causes, healthcare providers can be able to come up with strategies that improve patient attendance rates in a bid to positively alter the health outcomes of the patients and at the same time lessen the financial burden that the health on the health care system overall. Furthermore, it is important to mention that missed appointments continue to be a challenge that affects health facilities and patients, as they produce negative consequences including increased wait times, reduced access to services, and delays in treatment hence missed opportunities for the care of patients.
Research Objectives
- To explore the extent and the causes of missed mental health appointments at the mental health clinic in Riyadh, Saudi Arabia, with the goal of evidence-based models that aim directly at the patients’ access to improve attendance.
- To determine the real rate of no-shows at the mental health clinic.
Literature Review
This section provides an in-depth examination of the pressing issue of patients’ mental health appointments, targeting specifically Primary Health Care (PHC) in Riyadh, Saudi Arabia. In the health care, missed appointments are one of the major challenges, especially in the area of mental health some who would really benefit require constant attention so that their well-being can be achieved [3]. The latter statistics notwithstanding, the realities of missed appointments reflect those other regions and countries are also facing, and which require serious attention by health caregivers worldwide in order to get rid of such issues that affect treatment. Increasing these rates would somehow adversely affect the kind of lives that these counselled people tend to lead as well as put a lot of burden on the practitioners of health given the limited number of practitioners in a saturated area of practice.
Prevalence of Missed Appointments
Missed appointments within healthcare settings, specifically in mental health clinics, present a serious concern that has a negative impact on the overall health outcomes of people and the overall functionality of the healthcare system. In the clinic, Riyadh, Saudi Arabia, the missing appointment rates are alarmingly high and recent studies have revealed that as much as 23% to 30% of the scheduled appointments in the primary healthcare facilities were missed [8,9]. Similar findings have been reported in different research done internationally where missed appointment rates lie within the range of 5% to 55% and these rates mainly depend on the nature of the clinical field and the respective healthcare system [10,11]. Similarly, the research conducted in Nigeria brought forward high levels of missed appointments, further solidifying the fact that this problem cuts across various countries in the world [10].
The effects of missed appointments transcend individual health risks and escalate into larger systemic drawbacks. Findings from research indicate that patients suffering from chronic mental health conditions who fail to attend their scheduled meetings have a considerable chance of premature death, with some academic findings indicating that patients who miss more than 6 of their annual appointments are eight times more likely to die than patients who met with their doctors regularly [12,13]. Additionally, the likelihood of hospitalization and relapse is significantly increased when patients miss follow-up appointments and this worsens the issue of overworking the healthcare sector as a whole [12,13]. Just like the individual patients who fail to attend their appointments incur costs for the health care system, the magnitude of the financial consequences is also staggering where estimates indicate that the missed mental health appointments in the UK and US cost their health care systems over £100 billion and $340 billion a year respectively [3]. It has been noted that although these figures are only estimates, they do in some way accentuate the enormous potential for the primary care sector in the UK and the US to generate health care savings through improving mental health and adherence to appointments.
This phenomenon of missed health appointments continues to dominate the agenda because of its importance in the future of the healthcare system. All evidence suggests that missed appointments are associated with poor health outcomes and exploitation of health resources, which in turn requires urgent action. Hence, the problem calls for a concerted effort from the healthcare authorities, practitioners, and the community.
This includes the need for clear policies and procedures, developing and implementing effective strategies and interventions, and improving access to and acceptability of mental health services. Such measures must become central in addressing the phenomenon of missed appointments, with the ultimate aim of improving patient care and the efficiency of healthcare delivery in the future and globally. It is really significant that in-depth research on why people failed to attend appointments has been done so that ways to help them are developed as a result. In one of the investigations carried out, it was shown that many patients did not go for medical appointments due to barriers related to means of transport, forgetfulness, as well as life’s demands, which were competing for time - [14-16]. For instance, patient appointments cannot be missed only because there are people who require the services but have no way of getting there. More than one-quarter of the caregivers surveyed claimed they were unable to visit doctors or clinics due to transport issues.
This shows that access to health care facilities is particularly vital [14]. Also, through systematic research done in the review, forgetfulness and misunderstandings on the part of patients concerning their scheduled appointments have been identified as one of the most telling issues, which lead to the dismissal of these meetings as being insignificant [15]. Helping people remember their appointments could greatly reduce the number of no-shows - studies reveal that, when introduced, such systems as SMS notifications are able to reduce patients’ absentism by about 10% [4, 8]. Additionally, there are some specific groupings of people who are more likely than others to miss appointments in mental health care. These include adolescents, patients from low-income families, or those suffering from mental illness in addition to t heir other health problems - this has been concluded in the papers published by [9,13,17] The study conducted in Saudi Arabia found that patient satisfaction in dealing with service providers was a crucial element in ensuring people stick to their medical calendars and missing outpatient visits; thus, improving the quality of services could contribute to the growth of attendance at the clinics [8,25]. In this paper, the result is that the increase in attendance rates at medical appointments requires the impact of multiple actors since the responsibility cannot lie only with patients; it lies on healthcare providers, healthcare systems, and other stakeholders as there is a need for unity to reduce absenteeism at the clinics.
In the clinic, there is a growing worry regarding the overly high levels of missed appointments that are often reported in the region’s mental health clinics. It is therefore important that targeted research is carried out if we are to identify the possible reasons behind these alarming trends, as this is the only way effective solutions that would help mitigate the present issue can be developed. One of the most important issues that require attention and consideration during the course of this investigative study is the local environment and distinct patient characteristics. Therefore, unless the interventions designed are anchored on a proper understanding of the underlying factors affecting the uptake of such services, the improvements in appointment adherence will only be minimal, and the desired goal of enhanced patient outcomes will remain a pipe dream.
Barriers to Mental Health Care Access
Obtaining the psychological care that is required to be healthy is something that is often poorly served by a lot of the barriers that exist. One of the most essential points that should be considered in regard to the cultural beliefs is the great influence they have on the people’s attitude towards mental health care. To illustrate, it can be inferred that Patients face numerous obstacles when seeking mental health care. Fear of family reactions due to lack of awareness. Concerns about confidentiality impacting employment, and worries about future job prospects create significant barriers. Some individuals lack conviction in treatment, attending only due to recommendations, while others prematurely halt therapy upon initial improvement or mistakenly believe medications alone are effective. Logistical issues like transportation, conflicting work schedules, and missed appointment reminders further hinder access. Additionally, some patients struggle with clinic application technology, harbor skepticism towards primary healthcare referrals, or find clinic hours inconvenient due to holidays and seasonal events.
The power to make decisions be it through prescribing medication or offering other possible solutions to individuals who have mental health conditions, have the potential of being resisted by customs from other countries, especially older people [19]. This will definitely lead to the marginalization of persons with mental health problems [15,18]. Also know probably that the economic situation of people influences the access to mental health care. People from working classes usually encounter financial issues, which often reduce their abilities to seek help. As an illustration, an investigation discovered the influence of poverty as one of the most responsible for mental illnesses [16]. Besides, the availability of appropriate transportation options and the time it takes for these invalids to attend the appointments are factors that lead to the aggravation of such challenges as they entail additional hurdles which make it even more challenging for them to go to the carrion centres [20].
The problem is that stigmas about mental health is still one of the main barriers to care access. Most people are afraid of being processed as well as undressed, which can be one of the things that dissuade them from getting help. Medics have found that stigma exists in the majority, who probably claim that they are shame-faced of their mental health problems and are more into self-help than seeking professional medicine help [21]. This tends to keep people even further away from stressful circumstances, which means that many individuals today may need better mental health education due to a lack of awareness regarding mental health conditions and quality services, as well as there being an enormous treatment gap [22]. The major problems faced within the health care system also play a role in the barriers of obtaining mental health care. To illustrate, poor integration of mental health services within the primary care facility may cause the breakdown of a solid unit, which makes it hard for the patients to go through [23]. Besides, mental health professionals’ availability is usually limited, especially in rural and remote areas, and thus many patients have to wait for a long time until the appointment as well as they do not follow the treatment plan [24].
The study that has presented that the limited access to psychiatric care and professionals was the main obstacle to these people’s health care opportunities [24]. To put it one way, there are many sides to the fact that mental health care is not being delivered, and this happens besides the cultural beliefs, the economic situation, stigma and the ongoing at the healthcare systems. These problems of the access to mental health care are of various natures and the main ones are cultural beliefs, socioeconomic factors, stigma, and systemic healthcare issues. The key to overcoming these barriers entails a plan that would be made up of various elements like promoting people’s awareness and knowledge about the ongoing health conditions, achieving the service integration, and bettering the availabilities of culturally competent care. Taking care of these issues through healthcare systems can lead to their better functioning, thus allowing the access to mental health services be broadened - for all people, but especially those from the marginalized communities.
Methodology
The case study applied retrospective analysis of clinic data and program performance report review to evaluate the impact of integrating psychotherapy into the primary care setting. The following data was analyzed:
- Clinic performance report: This report presented an overview of the clinic’s achievements over the 2023 year including some details such as number of patients and number of no-show patients.
- Patient appointment data: I reviewed records showing how many appointments were scheduled for new and follow-up patients; virtual as well as physical visits; and the rate at which patient discharges were made.
- Reasons of Missed Mental Health Appointments 2024: Performance reports of random missed mental health appointments that already existed at the clinic Primary Health Care, Riyadh
Situation Analysis
This clinic performance report and patient appointment data are significant in understanding the effectiveness of integrating psychotherapy into primary care.
|
2023 |
Number of patients |
No show |
|
Jan |
1 |
34 |
|
Feb |
7 |
27 |
|
Mar |
12 |
37 |
|
Apr |
1 |
6 |
|
May |
19 |
24 |
|
Jun |
14 |
26 |
|
jul |
19 |
29 |
|
Aug |
43 |
29 |
|
Sep |
38 |
27 |
|
Oct |
39 |
28 |
|
Nov |
26 |
29 |
|
Dec |
39 |
44 |
|
total |
258 |
340 |
Table 1: Clinic performance report 2023.
The point where we have to examine patient appointment data from 2023 is shown in Table 1 because it provides insight into services offered by the clinic regarding its patients. The records indicate that there were a total of 598 appointments placed, there was 258 patients who missed appointments, and 340 total. The month with the most no-shows was December (39 missed appointments), and the month with the least no-shows was April corresponding to Ramadan (1 missed appointment).
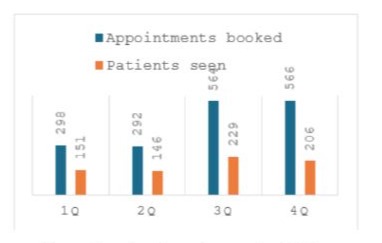
Figure 1: patients’ appointment data 2024.
The information is available in figure 1 when considering patients’ appointment data for the year 2024 shows a worrying trend of missed appointments in 2024. In the first quarter (1Q), while 298 appointments were booked, only 151 patients were seen, showing a huge 147 missed appointments. Similarly, the second quarter (2Q) had 292 appointments booked but only 146 patients have been seen, resulting in 146 missed appointments. The situation gets even worse in the third quarter (3Q), with 564 appointments booked and only 229 patients seen, leading to a significant 335 missed appointments. And the last quarter (4Q), with 566 appointments booked and only 206 patients seen, leading to a significant 360 missed appointments. This consistent and increasing difference between those who are seen and those who are booked suggests a potential patient adherence or scheduling effectiveness issue that needs further investigation.
The issue of missed appointments represents a significant challenge within the mental health services at the Primary Health Care (PHC) in Riyadh, Saudi Arabia. This situation analysis examines the available data, spanning from 1Q, 2024 to 3Q.
|
Ratio |
Standards |
|
0.28 |
Wrong referral |
|
0.02 |
Busy with work |
|
0.18 |
He does not want |
|
0.52 |
Other |
Table 2: Reasons of Missed Mental Health Appointments 2024.
“Over a ten-month period in 2024, a study was conducted involving monthly phone outreach to a random sample of 100 individuals (10 per month). The initial contact revealed a diverse range of factors hindering treatment engagement. A significant portion, 28%, reported receiving inappropriate referrals. Further investigation highlighted several common challenges: 2% cited work commitments as a barrier, while 18% expressed a complete disinterest in treatment. A substantial 52% of respondents detailed a complex web of concerns centered around privacy and social stigma. This included apprehension about family reactions, fear of breaches in confidentiality affecting employment, and logistical difficulties stemming from frequent travel.
Furthermore, a lack of conviction in treatment efficacy was evident, with some participants discontinuing care after initial symptom relief, believing it was no longer necessary. Others expressed a preference for medication over therapy, or faced obstacles related to transportation and scheduling. Concerns about maintaining confidentiality within their workplace, missed communication, and technological challenges among elderly participants were also noted. Additionally, some preferred specialist care to primary care. Finally, a significant number indicated that holidays and significant life events consistently interfered with their ability to attend appointments.
Findings
The situation analysis of mental health service integration at the Primary Health Care (PHC) in Riyadh presents a multi-faceted picture. In 2023, even though 598 appointments were scheduled, a substantial 43% (258) of them did not show up, with December having the highest rate (39) and April, which coincided with Ramadan, having the lowest (1). This movement signifies that potential obstacles in managing those who are actually coming are arising especially with regard to overlapping with existing plans of people, and individual characteristics of patients, among others. The program’s integration is a good thing as there have been positive results, such as increased service accessibility, reduced wait times, and a surge in late 2023 appointments, which could have been influenced by higher mental health awareness. Moreover, the data of patients’ appointment for the year 2024 shows a worrying trend of missed appointments in 2024. This consistent and increasing difference between those who are seen and those who are booked suggests a potential patient adherence or scheduling effectiveness issue that needs further investigation.
Health determinants in the field of referrals to social services draw attention to the necessity of an all-around approach, whilst high no-show rates of 21 per month, on average, during the year 2023, evidence the existence of system flaws. The study on appointments in 2024 even elaborated on the causes of missed appointments, uncovering that 28% of them were due to wrong referrals, 18% were a consequence of disinterest, and last but the largest number - 52% - were due to privacy concerns and social stigma. Besides, labor issues, unreal treatment efficacy, transportation difficulties, and technical problems also seemed to be the causes of nonattendance. These results show the need for focused activities to understand patient-specific difficulties, improve referral procedures, and make mental health services more accessible and acceptable to the public generally.
Discussion
This research aimed to check the depth and source of missing out mental health appointments at Primary Health Care (PHC) in Riyadh, Saudi Arabia and to know the actual no-show rate. The outcome discloses a very difficult situation in the prefix-patients attendance, which is in line with the literature that deals with the non-attendance of appointments in mental health settings that is common worldwide. The high no-show rate of 43% in 2023, especially in December, brings into focus the telling fact that the matter is quite pressing. This rate supports and sometimes goes beyond the 23-30% that are declared in other primary healthcare centers in Saudi Arabia and is a part of 5-55% of the global range, which can be understood as a very widespread challenge.
The seen fall and rise in no-show rates, where there is a visible decrease during Ramadan indicate that some non-medical conditions such as culture and religion play a role in appointment attendance. This is following the relevance to put cultural and religious factors into context while designing and running mental health services. The explosion of appointments in the late 2023 and the success story of Q1 2024 (equal new and follow-up patients, discharges), tells that the psychotherapy integration into the primary care system has made the access and awareness better. However, the always-had high no-show rates despite the improvements, the main causes are suspected to be systemic and patient-specific barriers.
The discovery in a study, that consent issues and fear of social stigma accounted for 52% of the missed appointments, is congruent with the prevalent talented people who pointed out the stigma that surrounds mental health care as the biggest barrier. This makes it clear that culturally sensitive measures are of supreme importance and that one focus of these would be on the topics of concern itself and the promotion of mental health literacy. The 28% of missed appointments, because the referrals were wrong, make us realize that there might be one problem in the whole referral process and thus a necessity to do something like the improvement of the screening and assessment procedures. The 18% indicative heads infer that, besides their concerns about the treatment’s effectiveness, patients should be educated and persuaded to disbelieve the myths and establish their convictions in mental health services.
One of the identified barriers in logistics refers to transportation and scheduling conflicts, which are in line with earlier research that explains the influence of socioeconomic factors on healthcare access. The problems like the elderly patient’s difficulty in coping with technological challenges, on the other hand, point to the importance of having user-friendly technologies. The findings also underscore the importance of the physician-patient relationship, as dissatisfaction with service providers and perceived lack of care can contribute to no-shows.
The study utilized a retrospective data analysis methodology that shed light on the clinic’s performance and patient appointment patterns. Nonetheless, there are also drawbacks. A 2024 study that contained some interesting pieces of information did not reach utopia as it was based on a small sample size and self-reported reasons for missed appointments which may be subject to bias. Future research should employ larger, more diverse samples and utilize mixed-methods approaches to gain a deeper understanding of the complex factors influencing appointment adherence.
Conclusion
To conclude, this study has presented shortage and causes of missed mental health appointments at PHC in an evidence-based way. Resolving this issue requires a comprehensive approach which includes such measures as cultural sensitivity training to staff, referral processes improvement, patient education and engagement, as well as service delivery models that are convenient for patients. The clinic can achieve reduced appointment nonadherence, improved patient outcomes, and the best use of mental health resources by overcoming these challenges.
Acknowledgment
Many thanks to Ms. Munira Abdulaziz Alajmi, Language and Translation Specialist for the English language improvement of this manuscript.
References
- Shabbir A, Alzahrani M, Khalid A (2018) Why do patients miss dental appointments in eastern province military hospitals, kingdom of saudi arabia?. Cureus. 10: e2355
- McQueenie R, Ellis DA, McConnachie A, Wilson P, Williamson AE, et al. (2019) Morbidity, mortality and missed appointments in healthcare: a national retrospective data linkage study. BMC Medicine. 17: 2.
- Triemstra JD, Lowery L (2018) Prevalence, predictors, and the financial impact of missed appointments in an academic adolescent clinic. Cureus. 10: e3613
- Khairuddeen NFI, Nazari NHNA, Al-Kadhim AHA, Samsudin AD, Amran N, et al. (2022) Prevalence and reasons for missed dental appointments among patients treated by undergraduate dental students of universiti sains islam malaysia. Iium Journal of Orofacial and Health Sciences. 3: 95-101.
- Miranne JM, Courtepatte A, Schatzman-Bone S, Minassian VA (2023) Risk factors for missed appointments at a multisite academic urban urogynecology practice. Urogynecology. 30: 406-412.
- Adepoju OE, Chae M, Liaw W, Angelocci T, Millard P, et al. (2021) Transition to telemedicine and its impact on missed appointments in community-based clinics. Annals of Medicine. 54: 98-107.
- Santos J, Camplain C, Pollitt AM, Baldwin JA (2023) A formative assessment of client characteristics associated with missed appointments in integrated primary care services in rural arizona. Journal of Evaluation in Clinical Practice. 30: 243-250.
- Alhamad Z (2013) Reasons for missing appointments in general clinics of primary health care center in riyadh military hospital, saudi arabia. International Journal of Medical Science and Public Health. 2: 258-267.
- Almalki, A (2014) Missed appointments at maternal healthcare clinics in primary healthcare centres in riyadh city: reasons and associated factors. Journal of Hospital Administration. 3: 92.
- Omokanye SA, Adeleke IT, Adekanye AO, Adewale FB, Nwachukwu CND, et al. (2021) Missed appointment at specialist outpatient clinics: the federal medical centre bida, northern nigeria experience. Int. J. Biol. Pharm. Sci. Arch 1: 133-144.
- Alawadhi A, Palin V, Staa TV (2021) Prevalence and factors associated with missed hospital appointments: a retrospective review of multiple clinics at royal hospital, sultanate of oman. BMJ Open. 11: e046596.
- Lesaca T (2017) The impact of queue-controlled modified open access scheduling on no-show rate in a community mental health child psychiatry med check clinic: a pilot study. Patient Experience Journal. 4: 141-144.
- Williamson AE, McQueenie R, Ellis DA, McConnachie A, Wilson P (2021) ‘missingness’ in health care: associations between hospital utilization and missed appointments in general practice. a retrospective cohort study. Plos One. 16: e0253163.
- Syed ST, Gerber BS, Sharp LK (2013) Traveling towards disease: transportation barriers to health care access. Journal of Community Health. 38: 976-993.
- Parsons J, Bryce C, Atherton H (2021) which patients miss appointments with general practice and the reasons why: a systematic review. British Journal of General Practice. 71: e406-e412.
- Nguyen DL, Dejesus RS, Wieland ML (2011) Missed appointments in resident continuity clinic: patient characteristics and health care outcomes. Journal of Graduate Medical Education. 3: 350-355.
- Perron NJ, Dao MD, Kossovsky MP, Miserez V, Chuard C, et al. (2010) Reduction of missed appointments at an urban primary care clinic: a randomised controlled study. BMC Family Practice. 11:79.
- Wilson R, Winnard Y (2022) Causes, impacts and possible mitigation of non-attendance of appointments within the national health service: a literature review. Journal of Health Organization and Management. 36: 892-911.
- Derr AS (2016) Mental health service use among immigrants in the united states: a systematic review. Psychiatric Services. 67: 265-274.
- Kilic C, Kaya E, Karadag O, Sarp Uner (2021) Barriers to accessing mental health services among syrian refugees in ankara.
- Radez J, Reardon T, Creswell C, Lawrence PJ, Evdoka-Burton G et al. (2020) Why do children and adolescents (not) seek and access professional help for their mental health problems? a systematic review of quantitative and qualitative studies. European Child & Adolescent Psychiatry. 30: 183-211.
- Errázuriz A, Schmidt K, Valenzuela P, Pino R, Jones PB (2023) Common mental disorders in peruvian immigrant in chile: a comparison with the host population. BMC Public Health. 23:1274.
- Hajebi A, Sharifi V, Abbasinejad M, Asadi A, Jafari N, et al. (2021) Integrating mental health services into the primary health care system: the need for reform in iran. Iranian Journal of Psychiatry. 16: 320-328
- Sijbrandij M, Acarturk C, Bird M, Bryant RA, Burchert S, et al. (2017) Strengthening mental health care systems for syrian refugees in europe and the middle east: integrating scalable psychological interventions in eight countries. European Journal of Psychotraumatology. 8:1388102.
- Alokeil N, AlGhaleb S, Alshehri M, Alromaih F, Almalky A, et al. (2023) Appointments delay and no-show among patients in primary health care centers, Riyadh, Saudi Arabia. Acta Scientific Medical Sciences. 10–18.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.