Comparison of the Clinical Effects of Two Chest Drainage Devices for Thoracoscopic Lung Surgeries
by Han-Yun Wu1, Yi Liu2*, Ming-Ho Wu1
1Department of Surgery, Tainan Municipal Hospital (managed by Show Chwan Medical Care Corporation), Taiwan
2Kaohsiung Medical University School of Nursing, No. 100, Shih-Chuan 1st Road, Sanmin Dist., Kaohsiung City, 807378, Taiwan
*Corresponding author: Yi Liu, Kaohsiung Medical University School of Nursing, No. 100, Shih-Chuan 1st Road, Sanmin Dist., Kaohsiung City, 807378, Taiwan
Received Date: 02 August, 2024
Accepted Date: 09 August, 2024
Published Date: 12 August, 2024
Citation: Wu HY, Liu Y, Wu MH (2024) Comparison of the Clinical Effects of Two Chest Drainage Devices for Thoracoscopic Lung Surgeries. Int J Nurs Health Care Res 7:1562. https://doi.org/10.29011/2688-9501.101562
Abstract
Objective: To compare the clinical efficacy of a digital drainage device versus a new drainage bag for pleural drainage after thoracoscopic lung surgery. Methods: This quasiexperimental two-group study involved one hundred patients assigned to the digital drainage device or the new drainage bag. After thoracoscopic lung resection, air leakage and drainage were evaluated until the chest tube was removed. The outcome criteria included chest tube indwelling and hospitalization days, as well as patient and nurse satisfaction. The data were statistically analyzed using chi-square and Mann-Whitney U tests. Results: There were no significant differences in the duration of chest tube indwelling (2.36 ± 1.53 days vs 1.96 ± 1.22 days, p=.153) or postoperative hospital stay (3.72 ±1.65 days vs 3.18 ± 1.54 days, p=.095) between the two groups. However, the scores of the patients (4.86 ± 0.34 vs. 3.82 ±0.98, p<.001) and their levels of nurse satisfaction (4.38± 0.717 vs. 3.07 ± 0.979 p<.001) were significantly greater in the new drainage bag group than in the digital device group. Conclusion: The effect of the new drainage bag system is equivalent to that of the digital drain system in terms of days of chest tube dwelling and hospital stay, and the new drainage bag system is more cost effective. Patient and nurse satisfaction with the new draining bag system is superior to that with the digital system in terms of convenience, ease of care, and promotion of early mobilization, proficiency, and efficiency.
Keywords: Thoracoscopic surgery; Digital drain system; New drain bag; satisfaction
Background
Thoracoscopic surgery is a common thoracic surgical technique [1], and patients typically require pleural air and fluid drainage for lung re-expansion following thoracic lung surgery [2]. Underwater seal bottles are commonly used for collecting fluid and pleural air drainage [2], but their use might interfere with mobilization and is associated with pneumonia, constipation, and urinary retention. Improper management of chest bottles induces fluid backflow and is likely to cause secondary infection [3]. The drainage volume of underwater seal bottles can be reduced when fluid accumulates, and incorrect placement of underwater seal bottles, such as tube misconnections, can result in life-threatening events [4]. Recently, many chest drainage devices have been developed [1,2,4] to accelerate lung expansion and reduce the length of chest tube indwelling and hospitalization. A new digital chest drainage system with real-time pressure monitoring and a continuous suction device [5,6] provides constant suction and digital recording of the speed of air leakage and fluid amount. However, an intermittent electric charge is needed to maintain the suction power. Many clinicians favor digital chest drainage devices over traditional chest drainage following pulmonary resection [6-8], with digital devices considered superior to underwater seal bottles. Researchers have also attempted to simplify pleural drainage [9-15] and develop a new drainage bag to improve the quality of care [16]. Its thin and flexible anterior wall prevents the air reflex, and its light weight could promote early ambulation [8]. It has been reported that there are no significant differences in the total drainage amount or duration of drainage between new bags and conventional chest bottles, and no device-related complications are observed [3,15,17]. Moreover, drainage bags are superior to chest bottles for postoperative drainage in inpatient care [7]. Therefore, this study was designed to compare the clinical effects of digital drainage devices and new drainage bags in thoracoscopic lung surgery and to investigate patient and nurse satisfaction with the use of different drainage devices after lung resection.
Materials and methods
Study design
This study had a quasiexperimental design.
Materials
Two devices were compared: a digital drainage device and a new drainage bag (Figure 1). The digital drainage device used was a Thopaz manufactured by Medela, which monitors air leaks and applies suction only to maintain negative pressure close to the chest. The digital display provides real-time objective data and a 24-hour historical graph of air leaks, but the drainage data may be inaccurate if the drainage bottle is unsteady. Once the collection bottle was full, it was replaced with an extra charge. The new chest drainage bag, designed in May 2016 [18], uses a Heimlich one-way valve and exhaust tube to discharge fluid and gas in the chest cavity; this bag has been tested for its antireflux effect and breathability. The pleural fluid can easily flow through by gravity or by coughing, and the amount of drainage is accurately recorded.
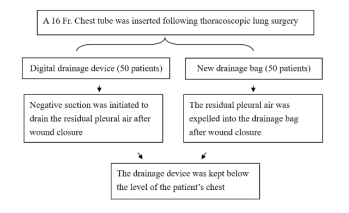
Figure 1: Flow chart of postthoracoscopic pleural drainage.
Study sample
This study was approved by the Institutional Review Board of Show Chwan Memorial Hospital, and the need to obtain informed consent was waived. The same thoracic surgeon operated on all patients aged 18 to 80 years who underwent thoracoscopic lung surgeries for benign or malignant disease. Patients who underwent thoracoscopic pneumonectomy, open lung surgery, robotic-assisted lung surgery, postoperative respiratory failure, ventilator use, or postoperative complications requiring reoperation were excluded. A total of 100 patients were enrolled from April 2022 to September 2023. The data from the digital drainage device group (Group 1) were collected first, followed by the new drainage bag group (Group 2).
Intervention procedures
The patients who met the inclusion criteria were evaluated based on chest Computed Tomography (CT) findings, health status, biochemical test results, and cardiopulmonary function. Before surgery, routine care, including deep breathing and effective coughing, was provided. And early ambulation, was applied.
Thoracoscopic lung resection was performed using a 4~6 cm incision at the anterior axillary line of the 4th intercostal space and a thoracoscopic port at the posterior axillary line of the 7th intercostal space. The bronchial stumps were closed using a stapler, incomplete interlobar fissures were divided using a stapler, and tissue glue was not used to control air leakage or bleeding. Before inserting the chest tube and performing wound closure, the airtightness of the bronchial stump and lung parenchyma was confirmed by the anesthetist’s manual bagging using 30 cm of water pressure.
Thoracoscopic surgery was performed according to the nature and location of the lesions. A chest tube (16 French) was inserted through the thoracoscopic port for pleural drainage. Scissors were used to add additional side holes to the chest tube, and the tip of the chest tube was placed at the top of the pleural space. Most of the pleural air was expelled when patients were switched to the supine position to remove the endotracheal tube. Typically, patients will be kept in the anesthesia recovery room for approximately 40 minutes, and chest radiography will be performed on admission to the general wards.
In group 1, digital drainage devices continuously detected pleural air leakage. In group 2, the drainage bag was kept below the patient’s chest wall or 20 cm below the bed. Air leaks were classified into three levels: the first level was the visible expansion of the bag during cough and forceful exertion, the second level was the visible expansion of the bag during talking, and the third level was the visible expansion of the bag during expiration. No air leakage was defined as no visible bag expansion during coughing or forceful exertion. For both groups, the chest tube was removed if there was no air leakage and if the 24-hour drainage volume was less than 100 mL.
Data collection
After the operation, the nurses installed the drainage equipment and transferred the patient to the recovery room. The patient was then assessed twice, once in the recovery room and once after admission to the ward, using the thoracic surgery information sheet. The patients were assessed twice daily, at 8:30 a.m. and 4:00 p.m., until the chest tube was removed to evaluate air leakage, drainage, and complications such as subcutaneous emphysema or pneumothorax. The duration of chest tube indwelling, hospitalization duration, and patient and nurse satisfaction were recorded after tube removal.
Statistical analysis
The data were tested for normality and are presented as the mean and standard error. Categorical data are presented as frequencies and percentages and were compared using the chi-square test. Student’s t test and the Mann-Whitney U test were used to compare the group differences. A P value less than 0.05 was considered to indicate statistical significance, and the statistical analysis was performed using the Statistical Package for Social Sciences (IBM SPSS Statistics 22).
Results
Sample characteristics
The participants’ characteristics in Table 1 show that most participants were male, with a mean age of 61.7 (34 to 80) years. There was no significant difference in the nature of the disease, site of lobectomy, drainage amount, or duration between the groups. Additionally, there were no significant differences between the groups in terms of the number of days of chest tube indwelling (2.36 ± 1.53 days vs 1.96 ± 1.22 days, p=.153) or postoperative hospital stay (3.72 ±1.65 days vs 3.18 ± 1.54 days, p=.095). However, the patients’ (4.86 ± 0.34 vs. 3.82 ±0.98, p<.001) and nurses’ satisfaction (4.38± 0.717 vs. 3.07 ± 0.979 p<.001) were significantly greater in the new drainage bag group than in the digital device group Figure 2. Patients were most satisfied with “no interference with sleep” and “ease of care”, whereas nurses were most satisfied with “no extra training time” and “confidence to use.” The detailed item scores are shown in Tables 2 and 3.
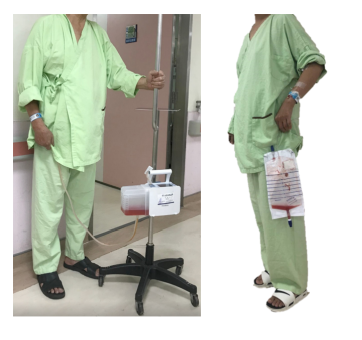
Figure 2: Patients using a digital device (left) or drainage bag (right).
|
Digital device |
Drainage bag |
p |
|
|
Age, years, mean ± SD |
61.4±11.3 |
61.9±9.7 |
0.799 |
|
Sex |
0.841 |
||
|
Male |
25 (50%) |
26 (52%) |
|
|
Female |
25 (50%) |
24 (48%) |
|
|
Disease |
0.683 |
||
|
Malignancy |
29 |
31 |
|
|
Benign |
21 |
19 |
|
|
Smoking |
0.685 |
||
|
yes |
22 |
20 |
|
|
no |
28 |
30 |
|
|
COPD |
0.595 |
||
|
yes |
7 |
10 |
|
|
no |
43 |
40 |
|
|
Previous lung surgery |
0.318 |
||
|
yes |
7 |
3 |
|
|
no |
43 |
47 |
|
|
BMI |
24.5±0.6 |
24.9±0.6 |
0.57 |
|
FEV1 |
1.11±0.03 |
1.11±0.04 |
0.916 |
|
Resection |
|||
|
Lobar resection |
18 |
21 |
0.407 |
|
RUL |
5 |
7 |
|
|
RML |
6 |
6 |
|
|
RLL |
6 |
3 |
|
|
LUL |
1 |
2 |
|
|
LLL |
0 |
3 |
|
|
Sublobar resection |
32 |
29 |
0.278 |
|
RUL |
12 |
10 |
|
|
RML |
3 |
0 |
|
|
RLL |
8 |
5 |
|
|
LUL |
6 |
12 |
|
|
LLL |
3 |
2 |
|
|
Duration of drainage, mean ± SD |
2.36±1.53 |
1.96±1.22 |
0.153 |
|
Postoperative stay, mean ± SD |
3.72±1.65 |
3.18±1.54 |
0.095 |
Table 1: Patient characteristics.
|
Items |
Digital device |
Drainage bag |
Z |
P |
||||
|
M |
SD |
M |
SD |
|||||
|
Light weighted |
3.72 |
0.85 |
4.88 |
0.32 |
-7.07 |
<.001 |
||
|
Easy to handle troubleshooting in tubing |
3.78 |
0.88 |
4.66 |
0.55 |
-5.206 |
<.001 |
||
|
Easy to use |
3.74 |
1.13 |
4.92 |
0.27 |
-6.402 |
<.001 |
||
|
Convenient to move out of the bed |
3.5 |
0.93 |
4.84 |
0.42 |
-7.347 |
<.001 |
||
|
Convenient to move around the bed |
3.98 |
0.93 |
4.84 |
0.42 |
-5.606 |
<.001 |
||
|
Easy to observe the drainage amount |
4.4 |
0.75 |
4.84 |
0.42 |
-5.117 |
<.001 |
||
|
Not interfere with my sleep |
4.22 |
0.97 |
4.98 |
0.14 |
-5.536 |
<.001 |
||
|
Not worry about others’ opinion |
3.66 |
1.18 |
4.82 |
0.48 |
-5.551 |
<.001 |
||
|
Ease of care |
3.46 |
1.21 |
4.96 |
0.19 |
-7.51 |
<.001 |
||
|
I am satisfied with the device |
3.82 |
0.98 |
4.92 |
0.27 |
-6.843 |
<.001 |
||
|
Item mean |
3.82 |
0.98 |
4.86 |
0.34 |
-6.218 |
<.001 |
||
Table 2: Patient satisfaction with the drainage system (n=50 per group).
|
Items |
Digital device |
Drainage bag |
Z |
p |
||
|
M |
SD |
M |
SD |
|||
|
Easy to setup |
3.34 |
0.883 |
4.5 |
0.631 |
-5.717 |
<.001 |
|
Correct drainage data |
3.67 |
0.928 |
4.34 |
0.74 |
-3.788 |
<.001 |
|
Easy to handle troubleshooting |
3.41 |
0.985 |
4.31 |
0.753 |
-5.051 |
<.001 |
|
Easy to replace |
3.03 |
0.978 |
4.46 |
0.695 |
-5.927 |
<.001 |
|
Convenience for patient ambulation |
3.09 |
0.959 |
4.43 |
0.714 |
-5.815 |
<.001 |
|
Easy to observe |
3.24 |
1.042 |
4.07 |
0.857 |
-4.202 |
<.001 |
|
Detect the device failure |
2.99 |
1 |
4.41 |
0.732 |
-5.868 |
<.001 |
|
Patient safety |
3.34 |
0.883 |
4.31 |
0.692 |
-4.896 |
<.001 |
|
No extra time for training |
2.8 |
1.044 |
4.64 |
0.638 |
-6.519 |
<.001 |
|
Confidence to use |
2.84 |
0.958 |
4.66 |
0.657 |
-6.716 |
<.001 |
|
Highly recommend |
3.01 |
0.97 |
4.54 |
0.698 |
-6.221 |
<.001 |
|
Proficiency in using |
2.48 |
1.093 |
4.5 |
0.757 |
-6.622 |
<.001 |
|
Familiar to use |
2.67 |
1.01 |
4.54 |
0.755 |
-6.643 |
<.001 |
|
Item mean |
3.07 |
0.979 |
4.38 |
0.717 |
-5.691 |
<.001 |
Table 3: Nurses’ satisfaction (n=70) with the drainage devices.
Discussion
There was no significant difference in the number of days of chest tube indwelling or hospitalization after lung resection using new drainage bags or digital drainage devices. These findings might be attributed to the same surgeon performing the surgeries, as there was no difference in surgical technique or procedure between the two groups. Furthermore, other risk factors affecting the healing of the lung surface after surgery and prolonging the air leakage time, such as sex, smoking status, BMI, COPD, severity of disease, and lung function, were not significantly different between the two groups [19-22].
Regarding patient satisfaction, previous studies have compared patients' positive perceptions of digital devices with those of traditional bottle systems [5-7]. This is the first study exploring patient satisfaction with digital and new drainage bag systems. The patients were most concerned about the draining device's weight, ease of use, and interference with mobilization, and they preferred the new bag system over the digital system. The new drainage bag weighs only 45 grams, so it is lightweight and easy to carry, thus promoting early mobilization. In contrast, digital devices are much heavier and more expensive than digital devices and require additional caution to avoid damage. In this study, two participants accidentally damaged the drainage bottle in the digital device, causing an extra charge. Furthermore, the electric motor in the digital device produces low-frequency noise and, occasionally, a high-frequency alarm, which might interfere with the patient’s sleep, even though this device provides the benefit of continuous suction for the prevention of pneumothorax.
The nurses were more satisfied with the new drainage bag device because it is much easier to use, replace, and assess, and they were proficient and confident in its use. For digital devices, nurses need extra time to learn about the arrangement and troubleshooting, as well as to set up the system and respond to alarms. According to previous studies, nursing staff's satisfaction with care methods is related to the complexity of care [23-25], as highly complex clinical work and cumbersome care processes increase their care burden and decrease their satisfaction.
Conclusion
The clinical effect of the new, less expensive drainage bag system is equivalent to that of the digital drain system in terms of the number of days of chest tube dwelling and hospital stay. Patient and nurse satisfaction with the new drainage bag system is superior to that with the digital system, so this new drainage bag system is recommended for thoracoscopy surgery, except for emphysema patients who have a greater risk of prolonged air leakage. Future research could extend the application of this new drainage system to patients undergoing open thoracotomy or robotic surgery.
Limitations
This study was quasiexperimental and did not include random selection or assignment. These results should be generalized with caution.
Funding/Support
This work was not supported by any organization.
References
- Bar I, Papiashvilli M, Kurtzer B, et al. (2009) Effect of Heimlich valve and under-water seal on lung expansion after pulmonary resection. Ind J Thorac Cardi-ovasc Surg 25: 183-187.
- Zisis C, Tsirgogianni K, Lazaridis G, et al. (2015) Chest drainage systems in use. Ann Transl Med 3: 43.
- Cerfolio RJ, Pickens A, Bass C, Katholi C (2001) Fast-tracking pulmonary resections. J Thorac Cardiovasc Surg 122: 318-324.
- George RS, Papagiannopoulos K (2016) Advances in chest drain management in thoracic disease. J Thorac Dis 8: S55-S64.
- Chen CH, Liu TP, Chang H, Huang TS, Liu HC, et al. (2015) A chest drainage system with a real-time pressure monitoring device. J Thorac Dis 7: 1119-1124.
- Zhou J, Lyu M, Chen N, et al. (2018) Digital chest drainage is better than tradi-tional chest drainage following pulmonary surgery. Eur J Cardiothorac Surg 54: 635-643.
- Wang H, Hu W, Ma L, Zhang Y (2019) Digital chest drainage system versus tradi-tional chest drainage system after pulmonary resection: a systematic review and meta-analysis. J Cardiothorac Surg. 14: 13.
- Braimbridge MV (1993) The history of thoracoscopic surgery. Ann Thorac Surg 56: 610-614.
- Adegboye VO, Adebo OA, Brimmo AI (1997) Postoperative closed chest drainage without an underwater seal: a preliminary report. Afr J Med Med Sci 26: 1-3.
- Secher O (1963) Disposable Bag for Thoracic Drainage Thorax. 18: 213-214.
- Vricella LA, Trachiotis GD (2001) Heimlich valve in the management of pneumothorax in patients with advanced AIDS. Chest. 120: 15-18.
- European Plastics News: Plastic T-Shirt Carrier Bag (1965).
- Vuorisalo S, Aarnio P, Hannukainen J (2005) Comparison between flutter valve drainage bag and underwater seal device for pleural drainage after lung sur-gery. Scand J Surg 94: 56-58.
- McKenna RJ, Fischel RJ, Gelb AF (1996) Use of the Heimlich valve to shorten hospital stay after lung reduction surgery for emphysema. Ann Thorac Surg 61: 1115-1117.
- Graham AN, Cosgrove AP, Gibbons JR, McGuigan JA (1992) Randomised clinical trial of chest drainage systems. Thorax. 47: 461-462.
- Wu MH, Wu HY (2018) Pleural drainage using a drainage bag for thoracoscopic lobectomy. Asian Cardiovascular & Thoracic Annals. 26: 212-217.
- Kadkhodaei HR (2007) Comparison of drainage bag and chest bottle for pleural drainage. Tanaffos 6: 36-39.
- Wu MH, Wu HY (2022) Development and application of chest drainage bags. Show–Chwan Med J 21: 23-29.
- Dugan KC, Laxmanan B, Murgu S, Hogarth DK (2017) Management of per-sistent air leaks. Chest. 152: 417-423.
- Pompili C, Falcoz PE, Salati M, Szanto Z, Brunelli A (2017) A risk score to predict the incidence of prolonged air leak after video-assisted thoracoscopic lobectomy: An analysis from the European Society of Thoracic Surgeons da-tabase. J Thorac Cardiovasc Surg 153: 957-965.
- Zheng Q, Ge L, Zhou J, et al. (2022) Risk factors for prolonged air leak after pulmonary surgery: A systematic review and meta-analysis. Asian J Surg 45: 2159-2167.
- Zhao K, Mei J, Xia C, et al. (2017) prolonged air leak after video-assisted tho-racic surgery lung cancer resection: Risk factors and its effect on postopera-tive clinical recovery. J Thorac Dis 9: 1219-1225.
- Pompili C, Dalmia S, McLennan Battleday F, Rogers Z, Absolom K, et al. (2022) Factors influencing patient satisfaction after treatments for early-stage non-small cell lung cancer. J Cancer Res Clin Oncol 148: 2447-2454.
- Gillet N, Fouquereau E, Coillot H, Cougot B, Moret L, et al. (2018) The effects of work factors on nurses' job satisfaction, quality of care and turnover intentions in oncology. J Adv Nurs74: 1208-1219.
- Ghazali D, Ilha-Schuelter P, Barbosa, Truchot J, Ceccaldi P, et al. (2021) Interdisciplinary teamwork for chest tube insertion and management: An integrative review. Anesthesiol In-tensive Ther 53: 456-465.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.