Breaking Metal and Bone - Multiple Consecutive TKA and DFR Failures in a Cyclist: A Case Report
by Wayne Goldstein, MD1, Asher Lichtig, MD1, Eric Chang MD1, Farid Amirouche, PhD1,2*
1Department of Orthopaedic Surgery, University of Illinois at Chicago, Chicago, Illinois, USA
2Department of Orthopaedic Surgery, Northshore University Health System, an Affiliate of the University of Chicago Pritzker School of Medicine. Skokie, Illinois, USA
*Corresponding Author: Farid Amirouche, Vice Chairman, Basic Science Research, Orthopaedic and Spine Institute, Department of Orthopaedic Surgery, Northshore University HealthSystem, 9669 Kenton Avenue, Skokie. IL 60076, USA
Received Date: 12 June 2025
Accepted Date: 19 June 2025
Published Date: 21 June 2025
Citation: Goldstein W, Lichtig A, Chang E, Amirouche F (2025) Breaking Metal and Bone - Multiple Consecutive TKA and DFR Failures in a Cyclist: A Case Report. J Surg 10: 11354 https://doi.org/10.29011/2575-9760.011354
Abstract
Background: This is the first reported case, to our knowledge, of progressive implant failure in a professional cyclist due to internal tibial rotation following varus correction osteotomy, aggravated by sport-specific mechanics. It emphasizes the necessity of rotational assessment and activity modification in high-performance patients, offering novel insights into longterm failure mechanisms.
Case presentation: A professional cyclist underwent an elective distraction osteotomy in 1997 to correct varus malalignment, resulting in severe internal rotation deformity of the distal tibia. The patient experienced five additional surgeries in 16 years follow-up due to progressive complications, including fractures of the femur and implant components. High-intensity cycling with clipless pedals exacerbated the rotational misalignment, subjecting implants to unanticipated forces.
Conclusion: This underscores the importance of preoperative assessment for rotational deformities and postoperative activity modifications in high-demand athletes. The interaction between biomechanical misalignment and repetitive cycling motion highlights a rare mechanism of implant failure, providing insight into optimizing outcomes.
Keywords: Cycling and knee arthroplasty; Distal femur replacement; Implant failures; Knee infection; Malunion; Osteotomy; Osteoarthritis; Periprosthetic fracture; TKA failure
Abbreviations: TKA: Total Knee Arthroplasty; rTKA: revision Total Knee Arthroplasty; DFR: Distal Femoral Replacement; DFF: Distal Femoral Fracture; OSH: Outside the Hospital
Introduction
Total knee arthroplasty (TKA) failures are not uncommon, with significant causes for revision being attributed to infection, mechanical loosening, and implant breakage. [1,2] In light of this, a periprosthetic fracture is another reason for TKA revision (rTKA). A study of 60,355 rTKA procedures between 2005 and 2006 found infections in 25.2% of revisions, with periprosthetic fractures occurring in 1.5%. [2] Another study of 18,065 rTKA patients between 2007 and 2012 reported infections at 25% and periprosthetic fractures at 3%. [1] Distal Femoral Replacement (DFR) was complicated by periprosthetic fractures in 8% of cases in another study. [3] Interest in these fractures arises from their rarity and surgical complexity. This report discusses a patient who underwent 6 procedures over 16 years for the same knee, starting with a proximal tibial distraction osteotomy for osteoarthritis and correcting left knee genu varum. A series of distal femoral and periprosthetic fractures led to the failure of revision DFR with femoral locking plates due to nonunion. The mechanical breakages seen in this case are unprecedented in the literature.
The patient’s long-distance cycling, likely driven by behavioral addiction, was a primary factor in the multiple arthroplasty failures.
Case Presentation
The surgical interventions performed on the patient are listed in Table 1.
Table 1.
|
Date of Procedure |
Procedure Type |
Eventual Cause of Failure |
|
1997 |
Distraction Osteotomy |
Malunion |
|
2006 |
TKA - Unstemmed |
Distal Femoral fracture just proximal to the bone-implant interface |
|
2010 |
TKA Revision #1 - Stemmed |
Fracture near the bone-implant interface and subsequent bolt failure |
|
2010 |
TKA Revision #2 - Stemmed |
Mid-shaft femur fracture |
|
2011 |
Distal Femoral Replacement |
Distal femoral Replacement stem fracture |
|
2013 |
Distal Femoral Replacement Revision + Locking Plate |
Nonunion |
Table 1: Timeline of the patient’s operative treatments from 1997-2013. Listed briefly are the procedure types; the adjacent column comments on the subsequent cause of failure for that same procedure.
Surgery/Phase 1: Initial Osteotomy and Malunion
In October 1997, the patient presented with varus malalignment of the left knee and underwent a distraction osteotomy in November to achieve 7º of valgus. Post-operatively, he achieved painless full weight-bearing with an external fixator. After its removal, he walked full weight-bearing. In August 1998, the patient experienced increased pain and was found to have a hypertrophic nonunion at the osteotomy site, leading to further plating and bone grafting (Figure 1). The patient was lost to follow-up and did not return until 2006. Imaging revealed a healed malunion, resulting in internal rotation of the distal tibia at the osteotomy site (Figure 2).

Figure 1: Radiographs of the patient’s initial clinical course, including A) Initial presentation, B) Initial distraction osteotomy, C) Nonunion, and D) Non-union plating with bone graft.
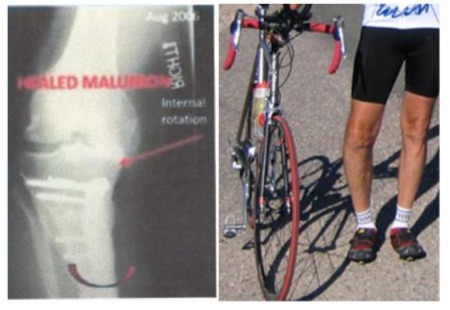
Figure 2: Plain radiograph depicting the site of healed malunion in the right tibia following plating and bone grafting, now with internal rotation present, as well as pictures of the knee with rotational deformity. The internal rotation depicted developed over a period of 9 years.
Surgery/Phase 2: Primary TKA and Failure
Evaluation in 2006 resulted in a decision that a repeat tibial osteotomy would not be feasible due to the encasement of the popliteal artery in scar tissue. He was referred to an arthroplasty specialist for a primary total knee arthroplasty (TKA) due to difficulty balancing the ligaments and correcting the coronal alignment. This procedure was performed using a Stemmed Rotating Platform (MBT) tibial component and a Sigma RP posterior-stabilized femoral component. After 12 weeks of physical therapy and a painless gait, the patient was allowed to ride his bicycle following evaluation by his surgeon at the three-month mark postoperatively. Notably, the patient is an avid long-distance cyclist, and he stated that he had already been riding his bike and was feeling great. In January 2010, he had been going to a rheumatologist on his own and was having repeated aspirations of hemarthrosis. After being consulted by this rheumatologist, the patient returned to the surgeon’s clinic in February 2010 with knee pain. Radiographs illustrated loosening and possible periprosthetic fracturing at the very distal femur with radiographic separation of cement from the bone without loosening at the bone-implant interface (Figure 3). The surgeon felt the hemarthrosis was a result of bleeding from the femur marrow, and there was a periprosthetic fracture.
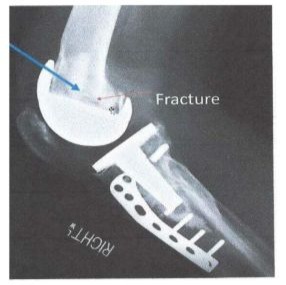
Figure 3: Plain radiograph depicting a distal femoral fracture proximal to the bone-implant interface following an unstemmed
TKA.
Surgery/Phase 3: TKA Revision #1 and Failure
After the failure of the primary total knee arthroplasty (TKA), a revision TKA (rTKA) in February 2010 was performed, utilizing a stemmed TC3 femoral component, and reinforced with rebar (Reinforced bars), given the Distal Femoral Fracture (DFF) that caused the initial failure (Figure 4). The rebar enforcement has been used numerous times by the attending physician. Rebar is commonly used to strengthen cement on roads. The attending used screws, impacted cancellous bone with bone cement to rebuild defects at interfaces in rTKA. The literature has validated it to improve the implant’s strength and stability [4,5]. Postoperatively, the patient felt well and returned to his daily activities, which included resuming competitive cycling shortly after the operation. The patient had no complaints of pain. However, almost 25 weeks later, the patient returned with reports of debilitating knee pain. Plain radiographs revealed that the patient had again undergone a DFF with additional breakage of the locking bolt in the femoral stem component (Figures 5 and 6). Between the first rTKA and failure, the patient reported daily cycling, equating to distances of over 100 miles per week.
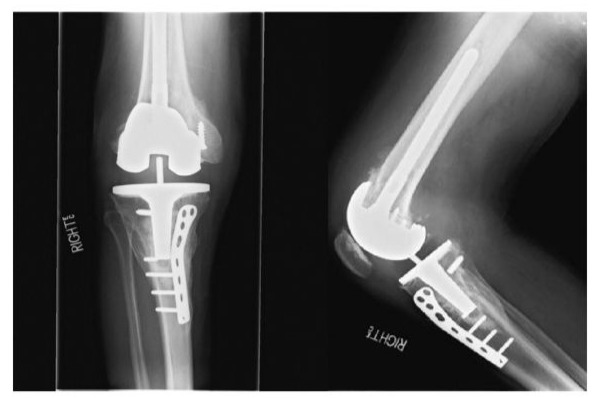
Figure 4: Initial post-operative films of first revision TKA.
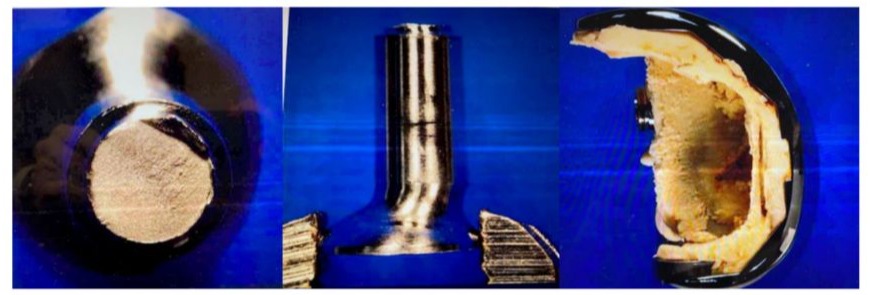
Figure 5: Boken cemented screw in the femoral component. Notice that the distal bone and cement firmly adhered to the femoral component, indicating there was no loosening but a distal fracture.
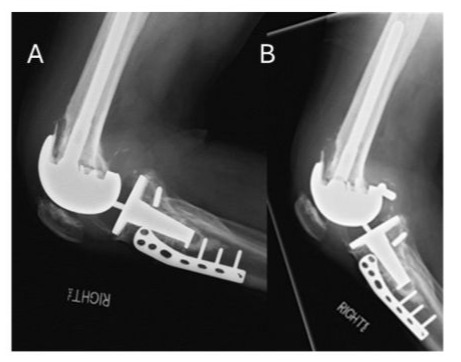
Figure 6: A) Plain radiograph depicting integrity of the TKA revision with stem 24 weeks post-op. B) Plain radiograph showing a distal femoral fracture near the bone-implant interface and subsequent cement bolt failure just 5 days after the 24-week post-op radiograph.
Surgery/Phase 4: rTKA #2 and Failure
The patient was then referred to another surgeon who used a different brand of revision implant and a component with a larger diameter and robust stem. The patient underwent a second rTKA at an outside hospital and received a Vanguard SSK Constrained Knee, which was constrained in a cast for 4 weeks to ensure varus-valgus alignment. 7 weeks post-op, the patient returned for manipulation under anesthesia for arthrofibrosis and 16 weeks later was found to have incurred a femoral fracture along the stem of the femoral TKA component (Figure 7). The patient was told to refrain from cycling. The patient reported again, however, having returned to competitive cycling following cast removal and, after 16 weeks, started to have severe pain.

Figure 7: Plain radiograph depicting post-operative pre and post-midshaft femoral fracture around the stem implant from TKA revision.
Mechanical Modeling of Surgery/Phase 4 Failure
The fracture leading to phase 4 surgery was unlikely and not due to periprosthetic malfunction or operative error. The patient’s cycling, despite physician advice, likely produced the forces needed to fracture the femur around the stem implant. Previous studies have shown that cyclists weighing 60 kg experience a compressive force of 700-800 N in the tibiofemoral joint during pedaling, with a maximum of 910 N during a hill-climbing stance. [6,7] However, these forces alone are insufficient to fracture the femur. In a biomechanical experiment on sawbone models at the University of Illinois at Chicago, 1236.68 N was required to fracture the femur, approximately 55% more than seated pedaling and 36% more than hill climbing (Figure 8). The patient’s prior malunion, causing internal rotation of the distal tibia, added rotational forces that contributed to the fracture.
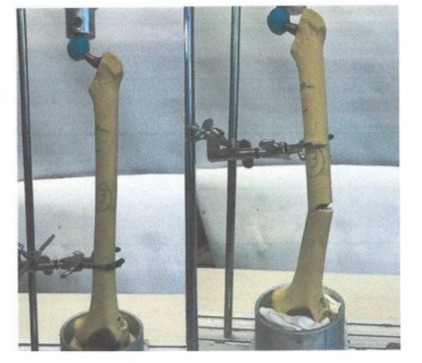
Figure 8: Saw-bone model with peri-prosthetics placed under axial load demonstrated mid-shaft fracturing at 1236.68 N of force.
Surgery/Phase 5: DFR and Failure
After the second rTKA failed, a DFR with a hinge was pursued at the outside hospital (OSH). The patient was advised not to exercise aggressively with this new implant, yet he continued to participate in competitive cycling. After six weeks, the patient returned for evaluation of leg pain, and it was discovered that the DFR had broken along the proximal metal stem (Figure 9).

Figure 9: Plain radiograph depicting AP of post-operative DFR and subsequent mid-stem fracturing at the site of the blue indicator. Surgery/Phase 6: Distal Femur Locking Plate and Failure
The femoral component of the DFR was replaced and reinforced with a femoral fracture plate with an allograft. After 12 weeks, the patient returned to the OSH and was found to have had nonunion of the proximal femoral osteotomy. Further imaging evaluation also revealed that the patient had unscrewed screws in the femoral plate construct, while also breaking the allograft, some other screws, and the plate itself (Figure 10).

Figure 10: The last available imaging from this patient shows a plain radiograph of a distal femoral replacement revision with a locking plate. The screws in the locking plate had been broken off. They unscrewed, as shown in this image, with an additional nonunion implant failure.
Surgery/Phase 7
A tertiary center performed a total femoral arthroplasty. At that time, the patient had stopped following up on the original arthroplasty and was subsequently lost to follow-up, and the outcomes were unknown.
Discussion/Summary
This case involves a rare pathology and an unusual patient. The fractures, including one of a non-modular femoral component, have never been reported before. These failures likely stem from two main factors: an unrecognized internal rotation of the distal tibia and excessive, intense cycling. Without both, the fractures wouldn’t have occurred. The initial osteotomy resulted in a 60-degree internal tibial rotation; however, the tibial component alignment remained unaffected, ensuring good intraoperative alignment. However, correcting the internal rotation was impossible due to ligament balancing. The rotation alone wouldn’t have caused such fractures without the combination of clipless pedals and high-intensity cycling. The patient used specialized gear for competitive cycling, which locked the left foot parallel to the bike frame, forcing external knee rotation and misaligning the mechanical axis. The patient performed 4800-6600 revolutions per hour, generating up to twice their body weight in force during standing. These forces, combined with the lack of foot rotation allowed by the clipless pedals, led to repeated implant failures, a scenario not previously reported. The pedals didn’t allow for the natural internal and external rotations needed for proper knee kinematics. When cyclists stand and pull down on the handles to increase pedal force, the force can be equivalent to or even double their body weight. The unexpected rotational forces led to repeated implant failures in this patient, which have not been reported before. The clipless pedal prevented foot rotation during knee flexion and extension, disrupting the natural internal and external rotations needed for proper knee kinematics (“screw home” mechanism). While modern clipless pedals allow 10-15 degrees of “float,” this patient’s Pedal allowed no float, as it was not designed for it.
Conclusion
This case highlights the potential risks of clipless pedals for TKA patients. While cycling is typically safe for most, individuals with uncorrected rotational deformities may experience unique implant failures due to repetitive, constrained foot movements, such as cycling or rowing. Surgeons should assess for malrotation in TKA patients with a history of prior fractures, and if present, advise against high-intensity, repetitive exercises that involve constrained foot movements.
References
- Pitta M, Esposito CI, Li Z, Lee Y-Y, Wright TM, et al. (2018) Failure After Modern Total Knee Arthroplasty: A Prospective Study of 18,065 Knees. J Arthroplasty 33: 407-414.
- Bozic KJ, Kurtz SM, Lau E, Ong K, Chiu V, et al. (2010) The epidemiology of revision total knee arthroplasty in the United States. Clin Orthop Relat Res 468: 45-51.
- Sobol KR, Fram BR, Strony JT, Brown SA (2022) Survivorship, complications, and outcomes following distal femoral arthroplasty for non-neoplastic indications. Bone Jt Open 3: 173-181.
- McPherson EJ, Sherif SM, Dipane MV, Arshi A (2021) Patellar Rebar Augmentation in Revision Total Knee Arthroplasty. J Arthroplasty 36: 670-675.
- Amirouche F, Choi KW, Goldstein WM, Gonzalez MH, Broviak S (2013) Finite element analysis of resurfacing depth and obliquity on patella stress and stability in TKA. J Arthroplasty 28: 978-984.
- Ericson MO, Nisell R (1986) Tibiofemoral joint forces during ergometer cycling. Am J Sports Med 14: 285-290.
- Soden PD, Adeyefa BA (1979) Forces applied to a bicycle during normal cycling. J Biomech 12: 527-541.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.