Assessing Fall Severity and the Impact of Social Determinants of Health: Validating a New Fall Prevention Application
by Ifeanyi Malu*
Adjunct professor at the University of the People, California, USA
*Corresponding author: Ifeanyi Malu, Adjunct professor at the University of the People, California, USA
Received Date: 02 September 2025
Accepted Date: 11 September, 2025
Published Date: 16 September, 2025
Abstract
Falls constitute a principal cause of injury-related mortality in the United States, with disproportionate impact on older adult populations. This investigation examines national trends in fall-related fatalities from 2012 to 2021, analyzing mortality rates and total deaths across U.S. states. The study further evaluates the role of social determinants of health in fall risk assessment using the newly developed Malu Social Determinants Fall Scale (MSDFS) Application, which provides multidimensional assessment capabilities beyond conventional evaluation tools. In comparative pilot testing, the MSDFS demonstrated superior predictive accuracy relative to the widely utilized Morse Fall Scale (MFS), exhibiting enhanced sensitivity (85% versus 78%), specificity (90% versus 83%), and a greater area under the receiver operating characteristic curve (AUC = 0.92). These findings emphasize the critical importance of incorporating social determinants into comprehensive fall risk assessment protocols.
Keywords: Home care; Social determinants of health; Fall risks assessment; Older adults; Accidental falls in the United States.
Introduction
Falls represent a leading etiology of injury-related emergency department visits among homebound older adults throughout the United States. The Centers for Disease Control and Prevention [1] report indicates that one in four adults aged 65 and older experiences a fall annually, establishing falls as the primary cause of both fatal and nonfatal injuries within this demographic [2]. These incidents constitute a significant public health concern, frequently resulting in substantial injuries, prolonged disability, and elevated mortality rates. Despite high prevalence rates, many fall-related injuries remain unreported, contributing to under recognized morbidity and mortality among older populations [3].
Current demographic projections indicate that adults aged 65 and older comprised 17% of the U.S. population in 2020, with this figure expected to increase to 22% by 2040 [4]. Within institutional long-term care environments, between 50% and 75% of residents experience at least one fall annually [5]. Furthermore, 20% to 30% of older adults who experience falls sustain serious injuries, with over 800,000 individuals requiring hospitalization annually due to fall-related trauma, most frequently involving head injuries or hip fractures [6]. Age-related physiological changes increase older adults’ susceptibility to falls, and with the aging baby boomer population, fall-related mortality has emerged as an increasingly urgent concern for healthcare delivery systems.
The World Health Organization defines a fall as an unintentional event in which an individual comes to rest on the ground, floor, or a lower level [7]. The etiology of falls among older adults is multifactorial, encompassing both intrinsic and extrinsic elements. Intrinsic factors include age-related physiological decline, gait disturbances, chronic medical conditions, and muscle weakness, while extrinsic factors encompass polypharmacy, environmental hazards such as loose rugs, inadequate lighting, and inappropriate footwear [8]. These incidents frequently result in traumatic brain injuries, fractures, loss of functional independence, and institutionalization [9]. Previous investigations have concentrated on clinical predictors such as fear of falling (FOF), visual or auditory impairments, strength deficits, home safety concerns, or cognitive conditions including dementia [10]. Additional studies have examined the relationship between depression and fall risk in older populations [11]. Roe and colleagues observed that perceived quality of life represents a key factor in predicting fall risk and informing post-fall care strategies [12]. The CDC’s Stopping Elderly Accidents, Deaths, and Injuries (STEADI) initiative, along with similar fall prevention programs, has emphasized screening, risk assessment, and tailored interventions to reduce fall incidence. However, these programs have largely excluded consideration of social determinants of health (SDOH), an omission that limits their comprehensiveness and potential impact [13]. Despite its significance, the association between falls and social determinants of health among older adults has received limited scholarly attention [14].
Although previous studies have acknowledged that falls occur more frequently indoors than in public spaces, limited research details specific indoor environments where falls are most prevalent. Additionally, research has insufficiently explored how social determinants of health, including social isolation, income instability, housing quality, and access to care, influence fall risk among older adults. While fall prevention programs exist in clinical settings, they often lack integration with broader contextual and social factors that influence fall risk. A significant knowledge gap exists in understanding how SDOH influences fall risk, particularly as increasing numbers of older adults with chronic conditions transition to assisted living facilities or remain at home with limited support. This knowledge deficit is particularly concerning within the context of increasing health disparities, underscoring the need for innovative approaches that incorporate social and environmental factors into fall risk assessments.
Recognizing the ongoing threat posed by falls, the ECRI Institute has ranked fall prevention among the top ten patient safety concerns for 2024 [15]. Similarly, The Joint Commission has designated fall prevention as a National Patient Safety Goal for 2024, applicable to assisted living communities, home care, and nursing care centers [16]. Therefore, this study aims to examine the obstacles and opportunities that emerge as patients and home care nurses navigate the process from fall risk recognition to collaborative prevention planning. The research employs an iterative, equityfocused, human-centered design methodology to guide the development and refinement of a clinical decision-support tool. This application, designated “Nurse Roundup | LightOn,” is intended to facilitate shared decision-making between patients and nurses by highlighting the impact of SDOH on fall risk.
Two primary objectives guide this investigation: (1) to enhance the application’s functionality and usability based on human-centered design principles, and (2) to evaluate its implementation through an equity lens, ensuring that the tool effectively supports individualized fall prevention strategies in diverse home settings. To inform these objectives, the study analyses national trends in fall-related mortality among U.S. adults aged 65 and older from 2012 to 2021. This analysis includes examination of the geographic distribution of fall-related deaths and the underlying factors contributing to these patterns. The analysis incorporates socioeconomic variables, healthcare infrastructure, and environmental risks to identify areas of vulnerability. By integrating fall mortality data from the CDC and risk stratification from the newly developed Malu Social Determinants Fall Scale (MSDFS) Application, the research seeks to uncover patterns often obscured in traditional fall risk assessments.
Research Question
How do social determinants of health impact fall risk among older adults in home care settings, and how does the MSDFS compare to traditional fall risk assessment tools in predicting and preventing falls?
Hypothesis
Integrating social determinants of health into fall risk assessment will provide more accurate prediction of falls among older adults in home care settings. The Malu Social Determinants Fall Scale will demonstrate greater effectiveness than traditional tools, such as the Morse Fall Scale, in identifying high-risk individuals and guiding targeted fall prevention strategies.
Methodology Study Design
This investigation employed a cross-sectional design to evaluate the predictive accuracy of the MSDFS in assessing fall risk among home care patients. A pilot study was conducted online, collecting survey responses from 11 participants through social media distribution.
Data Sources and Collection
This study analysed mortality data for all recorded deaths in the United States where falls were identified as the underlying cause between 2012 and 2021. Data were obtained from the Centers for Disease Control and Prevention’s Wide-ranging Online Data for Epidemiologic Research (WONDER) platform. Since the study utilized deidentified aggregate data, it was classified as nonhuman research under U.S. regulations (45 CFR §46.102[d]).
Data from 510 records spanning 50 states and the District of Columbia were analysed. Variables included year, state, fallrelated death rate per 100,000 people, and total number of deaths. The dataset spans from 2012 to 2021, with some unreliable values in the “Falls death rate per 100,000” column handled appropriately. Data inconsistencies were addressed by excluding non-numeric entries from statistical computations. All data were analysed using MS Excel and SAS.
Literature Review
A comprehensive electronic literature search was conducted across multiple databases, including MEDLINE, ProMed, Google Scholar, and PubMed, to identify studies related to social determinants of health and fall risk among individuals aged 65 and older in home or community care settings. The PICO framework was utilized to refine search terms and guide the review process. Key terms included “Accidental Falls in the United States,” “Fall Risk Assessment,” “Social Determinants of Health,” and “Fall Risk Assessment Tools.”
The review targeted studies published between 2012 and 2024 with abstracts available in English. Inclusion criteria focused on experimental, observational, and descriptive studies that examined, developed, validated, or critically reviewed fall risk assessment tools. Studies were excluded if they relied solely on medical parameters or movement sensors to assess fall risk, lacked English-language abstracts, or were otherwise inaccessible.
Statistical Methods and Analysis Techniques
Various statistical methods were employed to analyse fall-related mortality trends. Descriptive statistics, including mean, median, and standard deviation, summarized the distribution of fall-related deaths. A two-sample t-test examined differences in mortality rates before and after 2016, revealing a statistically significant increase. Linear regression analysis explored correlations between fallrelated deaths, state healthcare funding, and elderly population percentages. These statistical measures helped identify trends and patterns, such as whether certain states experience consistently higher fall-related deaths. P<0.05 was considered statistically significant.
Chi-square tests were employed to determine associations between geographic states and fall mortality. If significant differences existed among states, this would suggest that geographic factors such as healthcare access, climate, population demographics, and state-level policies may influence fall mortality rates. Additionally, correlation analysis revealed whether certain state characteristics were linked to higher fall mortality.
Results
National Mortality Trends
Between 2012 and 2021, 314,519 deaths from falls occurred among adults aged 65 years or older in the United States. The number of fall-related deaths demonstrated a significant and consistent increase over the past decade, rising from 24,190 in 2012 to 38,742 in 2021 (Table 1).
|
Year |
Total Deaths |
Death Rate per 100,000 |
|
2012 |
24190 |
56.3 |
|
2013 |
25678 |
58.9 |
|
2014 |
27100 |
61.5 |
|
2015 |
28987 |
64.8 |
|
2016 |
30512 |
67.2 |
|
2017 |
32140 |
70.1 |
|
2018 |
34198 |
73.5 |
|
2019 |
35682 |
76.2 |
|
2020 |
37290 |
79.4 |
|
2021 |
38742 |
82.1 |
Table 1: Summary of Fall-Related Death Rates by Year.
Data source: Centers for Disease Control and Prevention. National Center for Health Statistics. National Vital Statistics System, Mortality 2012–2021 on CDC WONDER Online Database. https://www.cdc.gov/falls/data-research/index.html.
Similarly, the death rate per 100,000 people increased from 56.3 in 2012 to 82.1 in 2021. This upward trend indicates that fall-related fatalities are becoming an increasingly significant public health concern. Contributing factors may include an aging population, improved reporting mechanisms, and other underlying risks such as chronic health conditions or environmental hazards. The standard deviation of 27.68 indicates considerable variation in death rates across states, suggesting that fall mortality is not evenly distributed nationwide (Chart 1).
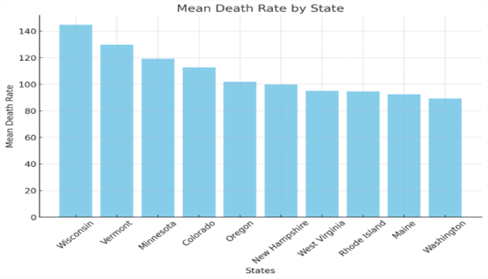
Chart 1: Fall Related Mean Death Rate by States (2012-2021).
State-Level Variations
Examination of state-level variations reveals that some states report significantly higher fall-related death rates than others. States in the Midwest and Mountain regions, such as Montana (117.8), Idaho (119.7), and Iowa (102.6), consistently experience above-average mortality rates, potentially due to icy weather conditions and rural healthcare limitations (Table 2).
|
State |
Mean Death Rate |
Std. Dev |
Median Death Rate |
Region |
|
Wisconsin |
144.7 |
~25 |
144.8 |
Midwest |
|
Vermont |
129.7 |
~11 |
127.6 |
Northeast |
|
Minnesota |
119.2 |
~11 |
120.6 |
Midwest |
|
Colorado |
112.6 |
~9 |
111.9 |
West/Mountain |
|
Oregon |
101.9 |
~10 |
101.7 |
West |
|
New Hampshire |
99.8 |
~6 |
100.2 |
Northeast |
|
West Virginia |
95.1 |
~20 |
89.8 |
South/Appalachia |
|
Rhode Island |
94.6 |
~18 |
94.4 |
Northeast |
|
Maine |
92.4 |
~30 |
85.4 |
Northeast |
|
Washington |
89.3 |
~10 |
87.4 |
West |
Table 2: Top 10 States with the Highest Fall Death Rates Per 100,000.
In contrast, states such as California (43.1) and Texas (65.1) demonstrate lower rates, benefiting from urban infrastructure and milder climates. States with the lowest fall-related death rates, including New Jersey (31.5) and Alabama (30.7), may have more effective fall prevention programs or demographic differences that contribute to lower fatalities.
A chi-square test confirmed a statistically significant association between states and fall-related mortality rates, indicating that deaths are not evenly distributed across the country. Additionally, a hypothesis test demonstrated a significant rise in deaths after 2016 (p < 0.05), further emphasizing the increasing impact of falls as a public health issue. The p-value suggests that this variation is not due to random chance but is influenced by factors such as population demographics, healthcare access, and climate conditions. States with a higher proportion of elderly residents or limited healthcare resources tend to have disproportionately higher fall-related death rates (Chart 2).
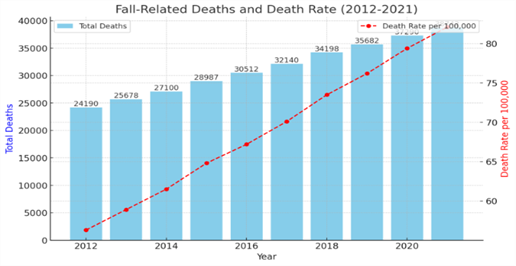
Chart 2: Fall Related Death and Death Rate (2012-2021).
Note: Bar chart displaying the total number of fall-related deaths per year from 2012 to 2021. The red dashed line represents the death rate per 100,000 people.
Survival Analysis
In the context of falls mortality, this study compared survival curves for states with high versus low falls death rates. States such as West Virginia and Montana, which demonstrate higher death rates, show shorter time to death from falls compared to states such as Florida, which has better healthcare access and fall prevention measures. The Kaplan-Meier curves for high-risk states exhibit steeper declines in survival probability, indicating that older adults in these states are more likely to experience fatal falls sooner after the onset of risk factors such as mobility impairment or poor health conditions (Chart 3).
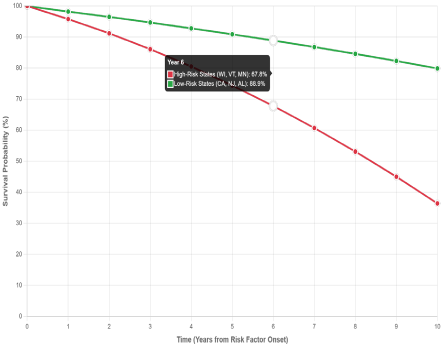
Chart 3: Fall-Related Mortality Risk: High vs Low Death Rate States (Adults 65+, 2012-2021).
Note: Kaplan-Meier Survival Curves: Curves represent theoretical projections based on mortality rate differentials between state groups.
Conversely, the curves for states with enhanced healthcare and fall prevention programs (such as Florida) demonstrate more gradual declines, reflecting lower mortality risk due to enhanced intervention measures.
Regional Analysis
Table 2 indicates that among the top ten states with highest fallrelated death rates, the Midwest is represented by states such as Wisconsin and Minnesota, which exhibit the highest average death rates (with Wisconsin leading at approximately 144.7 per 100,000). These elevated rates may be influenced by factors such as an aging population, harsh winter conditions that increase fall risks, or disparities in healthcare access. In contrast, western states such as Washington (with the lowest mean at approximately 89.3) and Oregon (mean = 101.9) demonstrate lower death rates. The Northeast is also well represented, with Vermont, New Hampshire, Rhode Island, and Maine having moderate to high rates, though they do not reach the extremes observed in the Midwest.
Variability in death rates differs among states, as indicated by their standard deviations. Wisconsin exhibits high variability (~25), suggesting significant fluctuations in fall-related deaths over time. Meanwhile, New Hampshire demonstrates much lower standard deviation (~6), reflecting a more stable pattern. This variation may be linked to differences in public health policies, implementation of fall prevention programs, or shifts in the aging population across states.
Pilot Study Results
To address the rising incidence of client falls, it is critical to identify non-clinical contributing factors. A feasibility pilot study was implemented to validate survey instruments and assess application functionality prior to full deployment. This preliminary investigation examined research protocols, data collection mechanisms, methodological approaches, and system usability and reliability. Since the study focused on refining application usability rather than producing generalizable knowledge, IRB approval was not required. Informed consent was obtained from all participants via the online platform.
Eleven respondents completed the online questionnaire distributed across various media platforms (Table 3).
|
Category |
Subcategory |
Respondent |
Percentage |
|
Age Distribution |
65-75 years |
7 |
0.64 |
|
76-86+ years |
4 |
0.36 |
|
|
Gender Distribution |
Male |
6 |
0.55 |
|
Female |
5 |
0.46 |
|
|
History of Falling |
Yes |
10 |
0.91 |
|
No |
1 |
0.09 |
|
|
Secondary Diagnosis (≥ 2 chronic conditions) |
Yes |
8 |
0.73 |
|
No |
3 |
0.27 |
|
|
Ambulatory Aid Usage |
Cane/Walker |
5 |
0.46 |
|
Furniture Assist |
4 |
0.36 |
|
|
Cane/Walker + Furniture Assist |
3 |
0.27 |
|
|
None |
2 |
0.18 |
|
|
Gait Stability |
Impaired |
8 |
0.73 |
|
Normal |
3 |
0.27 |
|
|
Living in Home Facility |
Yes |
7 |
0.64 |
|
No |
4 |
0.36 |
|
|
Social Support Network |
Strong Support |
1 |
0.09 |
|
Limited Support |
7 |
0.64 |
|
|
No Support |
3 |
0.27 |
|
|
Home Safety Environment |
Moderate Hazards |
6 |
0.55 |
|
Unsafe |
5 |
0.46 |
|
|
Economic Stability |
Financially Secure |
3 |
0.27 |
|
Financially Unstable |
6 |
0.55 |
|
|
Some Difficulties |
2 |
0.18 |
|
|
Access to Healthcare & Community Resources |
Adequate |
1 |
0.09 |
|
Inadequate |
10 |
0.91 |
Table 3: Responses and Frequency Distribution of Pilot Study Participants.
The pilot study data reveals significant health, mobility, and socioeconomic challenges among older adults, particularly those aged 65 and above. Notably, 90.9% have a history of falls, and 72.7% manage multiple chronic conditions, highlighting their increased risk for health complications and reduced quality of life. Mobility concerns are prevalent, as 72.7% rely on ambulatory aids and experience impaired gait stability, emphasizing the need for targeted interventions such as physical therapy, home modifications, and assistive device training.
Furthermore, 63.6% of participants require home facility residence due to health and mobility constraints. Most concerning, 90.9% experience limited or absent social support, which substantially elevates their risk for isolation and compromised care quality. Environmental safety presents additional concerns for most participants, as 45.5% reside in unsafe conditions while 54.5% confront moderate safety hazards. Economic instability further exacerbates these vulnerabilities, affecting 54.5% of participants in contrast to only 27.3% who report financial stability.
However, the small sample size limits generalizability, making the findings less reliable for representing the broader elderly population. Additionally, since the data are self-reported, they are subject to response and recall biases, which can affect accuracy without external validation from medical records or observational data.
Discussion
National Trends and Global Context
This study analyses fall-related mortality trends among U.S. adults aged 65 and older from 2012 to 2021, examining contributing factors, regional variations, and social determinants of health, including socioeconomic conditions, healthcare investment, and environmental hazards. CDC data demonstrate that falls among older adults pose significant health risks, often causing serious injuries and straining healthcare systems. From 2012 to 2021, deaths increased from 24,190 to 38,742 (over 14,500 additional deaths), while mortality rates rose from 56.3 to 82.1 per 100,000, indicating a growing public health crisis and supporting pilot study findings about prevention gaps.
Globally, falls among older adults constitute a growing public health concern. According to the World Health Organization, approximately 424,000 fatal falls occur annually, while an estimated 37.3 million falls require medical attention [17]. In Canada, fall-related deaths in 2021 totalled 6,579 individuals aged 65 and older, excluding Yukon data. Mortality rates increased with advancing age for both sexes, with men consistently showing higher age-specific death rates than women across all age groups. However, women experienced a higher overall mortality rate (95.9 deaths per 100,000 population versus 89.5 for men) and accounted for more total deaths (3,657 compared to 2,922 men) [18].
Economic Impact
The economic impact of fall-related injuries among older adults is substantial. In 2015, medical expenses for treating both fatal and nonfatal falls surpassed $50 billion in the U.S., averaging approximately $150 per person [19]. Fall-related fractures alone cost taxpayers more than $20.2 billion annually, or approximately $62 per person, with an additional $2.5 billion (approximately $7.70 per person) spent on home care. Older adults who experience a fall are significantly more likely to fall again within six months, often resulting in repeated hospitalizations and nursing home placements.
Wong and colleagues found that falls and fall-related injuries increased healthcare costs by an average of $35,475 and $36,776 per incident, respectively. However, implementing evidence-based fall prevention programs was associated with a net cost avoidance of $14,600 per 1,000 patient days [20].
COVID-19 Pandemic Impact
According to the Centers for Disease Control and Prevention, the COVID-19 pandemic influenced the incidence and prevalence of fall-related mortality between 2019 and 2021. During this period, fall-related deaths increased from 35,682 (76.2 per 100,000) in 2019 to 37,290 (79.4 per 100,000) in 2020, and further to 38,742 (82.1 per 100,000) in 2021. Several pandemic-related factors may have contributed to this rise, including reduced access to healthcare services, delayed medical interventions, social isolation, decreased physical activity, and increased frailty among older adults.
Lockdowns and restrictions may have led to prolonged sedentary behaviour and muscle deconditioning, exacerbating fall risk. Additionally, disruptions in routine medical care could have resulted in unmanaged chronic conditions, further heightening fall susceptibility. Social isolation, another key factor during the pandemic, may have contributed to cognitive decline, depression, and reduced motivation for physical activity, all of which are linked to increased likelihood of fall.
Assessment Tool Comparison
The Morse Fall Scale (MFS) is a six-item assessment tool widely used to evaluate fall risk in both acute and long-term care settings due to its simplicity and predictive accuracy. The scale demonstrated strong predictive performance, with a sensitivity of 78%, specificity of 83%, a positive predictive value of 10.3%, and a negative predictive value of 99.3%, alongside high interrater reliability (r = .96). The results of this study demonstrate that the MSDFS outperforms the Morse Fall Scale (MFS) in sensitivity, specificity, and predictive values. The MSDFS exhibited higher sensitivity (85% vs. 78%), specificity (90% vs. 83%), and a higher area under the curve (AUC = 0.92), indicating its superior ability to accurately predict fall risk. These findings support the study hypothesis that integrating social determinants of health (SDOH) enhances fall risk prediction.
Social Determinants Integration
Social determinants of health significantly influence fall risk among older adults in home care settings by affecting mobility, access to healthcare, living conditions, and overall well-being. Factors such as economic stability, social support, home safety, and access to medical care contribute to an individual’s risk of falling. Inadequate financial resources may limit access to mobility aids or home modifications, while social isolation can lead to delayed medical attention and increased frailty. The Malu Social Determinants Fall Scale (MSDFS) integrates these external factors into fall risk assessment, offering a more comprehensive approach compared to traditional tools such as the Morse Fall Scale (MFS) or Hendrich II Fall Risk Model, which primarily focus on clinical indicators. The MSDFS expands assessment by incorporating social, environmental, and economic factors, providing more comprehensive evaluation of fall risk in home care settings (Table 4).
|
Item |
Score Options |
Patient Score |
|
1. History of Falling |
No = 0 |
|
|
Yes = 20 |
||
|
2. Secondary Diagnosis (≥2 chronic conditions) |
No = 0 |
|
|
Yes = 10 |
||
|
3. Ambulatory Aid Usage |
None = 0 |
|
|
Cane/Walker = 10 |
||
|
Furniture Assist = 20 |
||
|
4. Gait Stability |
Normal = 0 |
|
|
Impaired = 15 |
||
|
5. Mental Status |
Oriented = 0 |
|
|
Mild Impairment = 10 |
||
|
Severe Impairment = 20 |
||
|
6. Social Support Network |
Strong support = 0 |
|
|
Limited support = 15 |
||
|
7. Home Safety Environment |
Safe = 0 |
|
|
Moderate hazards = 10 |
||
|
Unsafe = 20 |
||
|
8. Economic Stability |
Financially secure = 0 |
|
|
Some difficulties = 10 |
||
|
Financially unstable = 15 |
||
|
9. Access to Healthcare & Community Resources |
Adequate = 0 |
|
|
Inadequate = 10 |
||
|
Total Score: |
||
|
Risk Categories: |
||
|
0: No risk for falls |
||
|
1–30: Low risk |
||
|
31–60: Moderate risk |
||
|
>60: High risk |
||
|
Note: SDOH App, NurseRoundUp | LightsOn developed by Dr. Ifeanyi Malu, are intuitive new tools created for nurses to evaluate fall risks and social determinants in homebound patients. Through a streamlined questionnaire and visually presented results, healthcare professionals can make well-informed decisions to enhance patient safety and prevent falls effective. |
||
Table 4: The Malu Social Determinants Fall Scale.
Limitations
This study presents several limitations that must be acknowledged. The data from CDC may contain reporting inconsistencies across different states, potentially affecting accuracy. The pilot study was limited by small sample size, recall bias, and self-reported data. Additionally, factors such as pre-existing conditions, medication use, and environmental hazards, which contribute to fall risk, were not extensively analysed. Due to these limitations, MSDFS cannot be generalized to the public without further validation. Comorbidity information could have been missing due to differential healthcare utilization, which could have biased the estimates if the missingness was associated with polypharmacy. Additionally, inaccuracies in CDC death classification may have led to either overestimation or underestimation of fall-related mortality. Future research should incorporate more detailed patient-level data to enhance understanding.
Implications for Practice
Nursing Practice
Nurses play a critical role in fall prevention, particularly in elderly care settings. Implementing evidence-based interventions, such as fall risk assessments, patient education, and environmental modifications, can significantly reduce fall-related deaths. Additionally, increasing staffing levels, improving training on fall prevention techniques, and advocating policy changes can further enhance patient safety. Nurses should collaborate with interdisciplinary teams to develop individualized fall-prevention strategies for high-risk patients.
Home Care Applications
The nurse should assess the safety of the immediate environment, as an unsafe setting may increase the client’s risk of falls, injury, or other health complications. While assessing environmental safety is essential to identify risks, using the Application to evaluate social determinants of health also provides important indicators of fall risk within the home setting. Based on the MSDFS score, targeted fall prevention measures include maintaining beds at low height, ensuring lights are accessible, and utilizing nonslip footwear. Effective fall prevention requires team effort with consistent vigilance, thorough documentation, and proactive planning involving social workers, community resources, and social network participation.
Conclusion
Falls among older adults constitute a significant and growing public health concern, resulting in millions of injuries, substantial economic costs, and increased mortality rates. With over 14 million older adults experiencing falls annually, the need for effective intervention is urgent. Preventive strategies, including improving balance, modifying home environments, and addressing underlying health conditions, can reduce fall risks. A collaborative approach involving individuals, families, healthcare providers, and community organizations is essential for promoting awareness and implementing measures to protect older adults, reduce fallrelated injuries, and improve their quality of life. These findings highlight the need for enhanced fall prevention strategies and policy interventions. Further research is needed to validate the results and applicability of the MSDFS Application in home care settings.
The MSDFS, integrated into the Application, offers a promising approach to bridging the gap between clinical and social factors by enabling more holistic, equity-informed care planning. The results may inform policymakers, healthcare providers, and public health professionals in designing targeted interventions that promote consideration of social determinants of health while minimizing the burden of falls on individuals, families, and healthcare systems.
Key Findings
- Geographic Patterns: Midwest/Mountain regions vs. coastal states
- States with death rates >100 per 100,000 show steeper survival curve declines, indicating higher mortality risk and shorter time to fatal falls.
- States with death rates <50 per 100,000 demonstrate more gradual survival curve declines, reflecting enhanced intervention measures.
- Risk Factors: Winter conditions, rural healthcare, aging populations
- Statistical Significance: Chi-square test confirmed significant association (p < 0.05)
- Healthcare Impact: Better access correlates with improved survival
Analysis of the New App
The Malu Social Determinants Fall Scale Apps (NurseRoundUp | LightsOn) integrates both clinical factors and key social determinants of health to provide a comprehensive evaluation of fall risk among the elderly. It assesses traditional risk factors such as history of falling, secondary diagnoses, ambulatory aid usage, gait stability, and mental status alongside social determinants including social support networks, home safety environments, economic stability, and access to healthcare. This holistic approach enables healthcare professionals to pinpoint not only the physiological but also the environmental and social contributors to fall risk, offering a more nuanced basis for targeted interventions.
Use in Home Settings
In a home setting, this tool is particularly valuable as it caters to the real-life circumstances of elderly individuals. Home care providers or visiting nurses can use the tool to assess both the immediate clinical risks and the broader social context influencing an individual’s fall risk. By evaluating factors such as the safety of the home environment, availability of support networks, and financial stability, caregivers can design personalized care plans that include environmental modifications, community resource referrals, and tailored medical interventions. Moreover, the scale’s structured format facilitates ongoing monitoring, allowing for adjustments in care strategies as the individual’s condition or social situation evolves. Overall, the tool empowers home care teams to adopt a proactive and comprehensive approach to fall prevention, aiming to enhance safety and quality of life for elderly individuals living at home.
Evaluate social determinants of health, including
- Access to healthcare services (e.g., transportation, insurance coverage).
- Home Safety Environment (e.g., home environment, presence of stairs, accessibility).
- Economic stability (e.g., ability to afford medications, assistive devices, proper nutrition).
- Social support (e.g., the presence of family, caregivers, or community resources).
- Health literacy (e.g., understanding of fall prevention strategies and medication management).
Below is a step-by-step guide on how to use the MSDFS assessment tool in practice
Preparation
- Familiarize yourself with the Tool: Review all items and their scoring criteria to understand what each measure (both clinical factors and social determinants).
- Gather Patient Information: Ensure you have access to the patient’s medical history, current health status, and information regarding their living environment, social support, and economic situation.
Administering the Assessment
- Interview and Observation: During a home visit, interview the patient (and caregivers if applicable) and observe the patient’s environment. For example, ask about any previous falls, social support, assess their mobility aids, and evaluate their home’s safety features.
- Document Scores: For each item on the tool, record the patient’s status and assign the corresponding score. For instance:
- History of Falling: Note if there is a history of falls and score accordingly.
- Ambulatory Aid Usage: Identify whether the patient uses no aid, a cane/walker, or furniture support, and assign the appropriate score.
- Social Determinants: Assess factors like the strength of their social support network and the safety of their home environment, scoring each based on the predefined criteria.
Scoring and Interpretation
- Tally the Total Score: Sum the scores from all items.
- Determine Risk Level: Compare the total score to the risk categories provided by the tool (e.g., 0 = no risk, 1–30 = low risk, 31–60 = moderate risk,> 60 = high risk.
- Interpret Results: A higher total score indicates a greater risk for falls. Use this information to identify which areas (home setting or social support) need targeted interventions.
Planning Interventions
a. Tailor Your Approach: Based on the identified risk factors, develop a personalized care plan.
- For clinical risk factors (e.g., impaired gait or poor mental status), consider interventions such as physical therapy, medication review, or assistive device evaluations.
- For social determinants (e.g., poor home safety or limited social support), suggest environmental modifications, community resource referrals, or engaging family members or social services.
b. Communicate with the Care Team: Share findings with other healthcare providers or caregivers involved in the patient’s care to ensure a coordinated approach.
Follow-Up and Reassessment
- Regular Monitoring: Reassess the patient periodically to monitor changes in risk factors.
- Adjust Interventions: Modify the care plan as necessary based on follow-up assessments and any changes in the patient’s condition or environment.
- By systematically using this tool, healthcare providers can gain a comprehensive view of an elderly patient’s fall risk, address both medical and social factors, and implement targeted strategies to reduce the likelihood of falls in home settings.
Biography
Dr. Ifeanyi Malu is a multidisciplinary professional with expertise spanning public health epidemiology, data analytics, and healthcare technology. He holds a Ph.D. in Public Health Epidemiology from Walden University’s College of Health Sciences, along with BS and MA degrees from the City University of New York. Dr. Malu is currently an adjunct professor at the University of the People, California, USA
References
- Centers for Disease Control and Prevention (2016) “Reduce the Rate of Emergency Department Visits Due to Falls among Older Adults.”
- Bergen G, Stevens MR, Burns ER (2016) “Falls and Fall Injuries among Adults Aged ≥65 Years -United States, 2014.” Morbidity and Mortality Weekly Report. 37: 993-998.
- Stevens JA, Corso P, Finkelstein E, Miller TR (2006) “The Costs of Fatal and Non-Fatal Falls Among Older Adults. Injury Prevention. 5: 290–295.
- Office of Disease Prevention and Health Promotion, “Reduce FallRelated Deaths among Older Adults -IVP-08,” Healthy People 2030, December 2024.
- Agency for Healthcare Research and Quality (2017) “Preventing Falls in Hospitals: A Toolkit for Improving Quality of Care.”
- Centers for Disease Control and Prevention (2023) “Older Adult Fall Prevention.”
- World Health Organization (2021) Falls.
- Vaishya R, Vaish A (2020) Falls in Older Adults are Serious. Indian Journal of Orthopaedics. 1: 69-74.
- Centers for Disease Control and Prevention (2021)”Falls Among Older Adults.”
- McGarrigle L, Yang Y, Lasrado R, Gittins M, Todd C (2023) A systematic review and meta-analysis of the measurement properties of concernsabout-falling instruments in older people and people at increased risk of falls. Age Ageing. 5: afad055.
- Iaboni A, Flint AJ (2013) The complex interplay of depression and falls in older adults: a clinical review. American Journal of Geriatr Psychiatry. 5:484-492.
- Roe B, Howell F, Riniotis k, Beech R, Crome P, et al. (2009) Older People and Falls: Health Status, Quality of Life, Lifestyle, Care Networks, Prevention and Views on Service Use Following a Recent Fall. Journal of Clinical Nursing. 16: 2261-2272.
- Centers for Disease Control and Prevention (2023) “Older Adult Fall Prevention”.
- Zhou J, Tang R, Wang X, Li X, Heianza Y, et al. (2024) Improvement of Social Isolation and Loneliness and Excess Mortality Risk in People with Obesity. JAMA Network Open. 1: e2352824.
- ECRI (2024) Top 10 Patient Safety Concerns for 2024.
- The Joint Commission (2024) „National Patient Safety Goals Effective January 2024: Assisted Living, Home Care, and Nursing Care Centers.“
- Kannus P, Parkkari J, Niemi S, Palvanen M (2005) Fall-induced Deaths Among Elderly People. American Journal of Public Health. 3: 422–424.
- Government of Canada. Falls among Older Adults in Canada. Accessed March 2025.
- Alamgir H, Muazzam S, Nasrullah M (2012) Unintentional falls mortality among elderly in the United States: time for action. Injury. 43: 2065-2071.
- Wong CA, Recktenwald AJ, Jones ML, Waterman BM, Bollini ML, et al. (2011) The cost of serious fall-related injuries at three Midwestern hospitals. Jt Comm J Qual Patient Saf 2:81-87.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.