Analysis of the Current Status and Influencing Factors of Agitation during the Recovery Period after General Anesthesia
by Ying Long, Ruyue Han, Weinan Sun, Yi Wu, Zemin Zhan*
Department of Nursing Nansha Division of The First Affiliated Hospital, Sun Yat-sen University, Guangdong 511400, China
*Corresponding author: Zemin Zhan, Department of Nursing Nansha Division of The First Affiliated Hospital, Sun Yat-sen University, Guangdong 511400, China
Received Date: 14 August 2025
Accepted Date: 21 August, 2025
Published Date: 25 August, 2025
Citation: Long Y, Han R, Sun W, Wu Y, Zhan Z (2025) Analysis of the Current Status and Influencing Factors of Agitation during the Recovery Period after General Anesthesia. Int J Nurs Health Care Res 8:1662. DOI: https://doi.org/10.29011/2688-9501.101662
Abstract
Objective: Emergence agitation during the recovery period can negatively affect the quality of awakening, increase patient risks, prolong postoperative recovery time, and reduce postoperative comfort. Early identification of risk factors for postoperative agitation is critical for timely intervention. This study aims to analyze the factors influencing emergence agitation in patients undergoing general anesthesia during the recovery period. Design: This study was conducted as a cross-sectional, prospective descriptive study. Methods: A total of 1,998 cases of patients undergoing general anesthesia were selected using a convenience sampling method from the anesthesia recovery room of a tertiary hospital between May 2023 and December 2024. Clinical medical records were reviewed, and logistic stepwise regression analysis was conducted to identify the influencing factors of emergence agitation in these patients. Results: Among the 1,998 patients, 122 experienced emergence agitation, with an incidence rate of 6.5%. Logistic regression analysis revealed that the main influencing factors for emergence agitation included age 60–74 years, history of smoking and alcohol use, tracheal intubation duration >4 hours, presence of postoperative drainage tubes, urological surgery, postoperative hypothermia, and postoperative pain (P<0.05). Conclusion: The occurrence of emergence agitation in patients undergoing general anesthesia is influenced by multiple factors. This suggests that nursing staff should enhance patient assessment, closely monitor postoperative vital signs, and implement measures to reduce the incidence of emergence agitation, thereby improving awakening quality and patient prognosis.
Keywords: Postoperative; General anesthesia; Agitation; Influencing factors
Introduction
Emergence agitation (EA) is a self-limiting state of excessive neurological excitation that occurs as patients regain consciousness from general anesthesia [1], It is characterized by a brief period of dissociation between consciousness and behaviour during the transition from unconsciousness to full awareness [2], Clinical manifestations include a combination of excitement, agitation, and disorientation, accompanied by involuntary movements of the limbs, irrational speech, crying or moaning, and delusional thinking [3], EA is a common postoperative complication in patients undergoing general anesthesia, with an incidence rate of 17.09%- 24.80% [4]. The occurrence of EA can negatively affect the quality of awakening, increase patient risks, prolong postoperative recovery time, and reduce postoperative comfort. Prolonged agitation may result in hazardous behaviours, such as unintentional removal of endotracheal tubes or vigorous struggling, which could lead to hypoxia, falls, or accidental dislodgement of medical devices, thereby endangering patient safety. The recovery phase of anesthesia is a critical period in the perioperative process.
Early identification of risk factors for postoperative agitation is essential for timely intervention and provides a scientific basis for anesthesia recovery room nurses to develop appropriate care plans.
Materials and Methods
Design
This study was conducted as a cross-sectional, prospective descriptive study.
Inclusion and Exclusion Criteria
This study adopted a convenience sampling method to select patients who underwent general anesthesia, were awaiting recovery, and were admitted to the post-anesthesia care unit (PACU) of a tertiary hospital in Guangzhou, China, between May 2023 and December 2024. A total of 1,998 eligible patients were included.
Inclusion Criteria:
- Patients aged >18 years with good reading comprehension, language communication, and cognitive abilities;
- Patients who voluntarily or as per medical advice underwent general anesthesia with endotracheal intubation, rather than local or regional anesthesia;
- Patients who were aware of their medical condition and voluntarily agreed to participate in this study.
Exclusion Criteria:
- Patients whose health status could influence the results, such as those with severe complications or diseases affecting anesthesia outcomes;
- Patients with severe mental or neurological disorders that precluded cooperation with the study;
- Patients with known allergies to specific drugs or a history of adverse reactions to anesthesia;
- Patients requiring postoperative admission to the
intensive care unit (ICU);
- Patients who were too debilitated to communicate;
- Patients requiring reintubation. A total of 1998 patients were ultimately included in this study.
Instruments
Clinical Data Collection:
A self-designed clinical data survey form was used by the research team. The survey included variables such as gender, age, BMI, history of smoking and alcohol use, anesthesia history, surgical history, blood transfusion history, cardiac function classification, airway assessment, presence of urinary catheters, drainage tubes, or nasogastric tubes, ASA classification, postoperative hypothermia, intubation duration, surgical type, postoperative pain severity, and pain management methods (Table 1).
|
Item |
Number
of cases (N=1998) |
Postoperative
agitation group (N=122) |
Non-Postoperative
agitation group (N=1876) |
t |
P-Value |
|
Gender |
|||||
|
Male |
962 (48.1) |
79 (64.8) |
883 (47.1) |
-3.757 |
<0.001*** |
|
Female |
1036 (51.9) |
43
(35.2) |
993
(52.9) |
||
|
Age |
|||||
|
18y-44y |
881 (44.1) |
39 (32.0) |
842
(44.9) |
6.758 |
<0.001*** |
|
45y-59y |
644 (32.2) |
34 (27.9) |
610 (32.5) |
||
|
60y-74y |
429 (21.5) |
44
(36.1) |
385
(20.5) |
||
|
≥75y |
44
(2.2) |
5
(4.1) |
39
(2.1) |
||
|
BMI |
|||||
|
<18.5
kg/m2 |
106 (5.3) |
3
(2.5) |
103
(5.5) |
0.882 |
0.45 |
|
18.5-23.9
kg/m2 |
1010 (50.6) |
61 (50.0) |
949
(50.6) |
||
|
24-26.9 kg/m2 |
642 (32.1) |
44
(36.1) |
598
(31.9) |
||
|
≥27 kg/m2 |
240 (12.0) |
14
(11.5) |
226
(12.0) |
||
|
History of tobacco and alcohol |
|||||
|
Yes |
275 (13.8) |
34
(27.9) |
241
(12.8) |
-3.526 |
<0.001*** |
|
No |
1723 (86.2) |
88
(72.1) |
1635
(87.2) |
||
|
History of anesthesiology |
|||||
|
Yes |
1010 (50.6) |
69
(56.6) |
941
(50.2) |
-1.371 |
0.006** |
|
No |
988 (49.4) |
53
(43.4) |
935
(49.8) |
||
|
History of blood transfusion |
|||||
|
Yes |
37 (1.9) |
2 (1.6) |
35 (1.9) |
0.180 |
0.717 |
|
No |
1961 (98.1) |
120 (98.4) |
1841 (98.1) |
|
|
|
Cardiac function ratings |
|||||
|
I |
1632 (81.7) |
90 (73.8) |
1542 (82.2) |
3.06 |
0.047* |
|
II |
361 (18.1) |
32 (26.2) |
329 (17.5) |
||
|
III |
5 (0.3) |
0 |
5 (0.3) |
||
|
Mallampati airway classification |
|||||
|
Ⅰ |
1269 (63.5) |
72
(59.0) |
1197 (63.8) |
1.933 |
0.122 |
|
Ⅱ |
688 (34.4) |
44
(36.1) |
644 (34.3) |
||
|
Ⅲ |
33 (1.7) |
5
(4.1) |
28 (1.5) |
||
|
Ⅳ |
8 (0.4) |
1
(0.8) |
7 (0.4) |
||
|
Urinary Catheter |
|||||
|
Yes |
866 (43.3) |
81 (66.4) |
785 (41.8) |
-5.049 |
<0.001*** |
|
No |
1132 (56.7) |
41 (33.6) |
1091 (58.2) |
||
|
Drainage tube |
|||||
|
Yes |
799 (40.0) |
82 (67.2) |
717 (38.2) |
-5.806 |
<0.001*** |
|
No |
1199 (60.0) |
40 (32.8) |
1159 (61.8) |
||
|
Stomach tube |
|||||
|
Yes |
44 (2.2) |
8 (6.6) |
36 (1.9) |
-2.091 |
<0.001*** |
|
No |
1954 (97.8) |
114 (93.4) |
1840 (98.1) |
||
|
ASA grade |
|||||
|
Ⅰ |
163 (8.2) |
7 (5.7) |
156 (8.3) |
4.239 |
0.015* |
|
Ⅱ |
1484 (74.3) |
82 (67.2) |
1402 (74.7) |
||
|
Ⅲ |
351 (17.6) |
33 (27.0) |
318 (17.0) |
||
|
Postoperative hypothermia |
|||||
|
Yes |
62 (3.1) |
20 |
42 (2.2) |
-4.493 |
<0.001*** |
|
No |
1936 (96.9) |
102 |
1834 (98.3) |
|
|
|
Duration of tracheal intubation |
|||||
|
0h-2h |
454 (22.7) |
6 (4.9) |
448 (23.9) |
37.968 |
<0.001*** |
|
2h-4h |
1105 (55.3) |
47 (38.5) |
1058 (56.4) |
||
|
4h-6h |
312 (15.6) |
41 (33.6) |
271 (14.4) |
||
|
>6h |
127 (6.4) |
28 (23.0) |
99 (5.3) |
||
|
Surgical type |
|||||
|
Urology |
416 (20.8) |
28 (23.0) |
388 (20.7) |
44.038 |
<0.001*** |
|
Abdominal surgery |
620 (31.0) |
46 (37.7) |
574 (30.6) |
||
|
Thoracic
surgery |
319 (16.0) |
11 (9.0) |
308 (16.4) |
||
|
Head and neck surgery |
385 (19.3) |
10 (8.2) |
375 (20.0) |
||
|
Orthopedic surgery |
246 (12.3) |
15 (12.3) |
231 (12.3) |
||
|
Others |
12 (0.6) |
12 (9.8) |
0 |
||
|
Postoperative pain |
|||||
|
Yes |
51 (2.6) |
19 (15.6) |
32 (1.7) |
4.662 |
<0.001*** |
|
No |
1947 (97.4) |
103 (84.4) |
1844 (98.3) |
||
|
Analgesic modalities |
|||||
|
PCVA |
514 (25.7) |
46 (37.7) |
468 (24.9) |
-2.766 |
<0.001*** |
|
No |
1484 (74.3) |
76 (62.3) |
1408 (75.1) |
||
|
BMI, body mass index; ASA, American Society of Anesthesiologists;
PVCA, Patient Controlled Vein Analgesia; t, t-test. *P<0.05; **P<0.01; ***P<0.001 |
|||||
Table 1: Univariate analysis of the occurrence of agitation during the resuscitation period after general anesthesia (N=1998).
Postoperative Agitation Diagnostic Criteria:
The Richmond Agitation-Sedation Scale (RASS) [5] was used to assess agitation. The scale includes 10 sedation levels, with scores ranging from -5 to +4, reflecting levels of consciousness from “combative” to “unresponsive.” Specifically, a score of -5 indicates coma; -4, deep sedation; -3, moderate sedation; -2, light sedation; -1, drowsy; 0, alert and calm; +1, restless; +2, agitated; +3, very agitated; and +4, combative. A score ≥1 was used to diagnose EA.
Data Collection
The researchers collected data based on clinical records, including patient demographics and anesthesia recovery-related information, which were recorded in the hospital’s surgical anesthesia information system. Relevant data were retrieved from this system. On the day of surgery, the patients’ agitation levels were assessed. The entire process adhered to the dual-review principle to ensure accuracy and reliability.
Statistical Analysis
Data entry and statistical analysis were performed using SPSS 25.0 software. Continuous variables were expressed as medians and interquartile ranges, while categorical variables were presented as frequencies, percentages, or proportions. Univariate analysis of postoperative agitation was conducted using t-tests and analysis of variance (ANOVA). Multivariate analysis was performed using logistic stepwise regression. P<0.05 was considered statistically significant.
Result
Occurrence of Emergence Agitation
Between May 2023 and December 2024, a total of 2476 patients underwent surgery. Postoperatively, 106 patients were admitted to the ICU, and 32 patients were transferred to the ward, thus being excluded from the study. A total of 2338 patients under general anesthesia were transferred to the PACU after surgery. In the postoperative agitation group, 3 patients underwent repeated surgery within 2 weeks, 5 patients were under 18 years old, 5 patients had other mental disorders, and 4 patients had missing data. In the postoperative non-agitation group, 31 patients underwent repeated surgery within 2 weeks, 243 patients were under 18 years old, 20 patients had other mental disorders, and 29 patients had missing data. According to the exclusion criteria, a total of 1998 patients were included in the final analysis (Figure 1). Based on whether patients experienced postoperative agitation, 1998 patients who underwent general anesthesia were divided into the agitation group and the non-agitation group. There were 122 cases in the postoperative agitation group and 1876 cases in the non-agitation group, with an incidence rate of 6.5%.
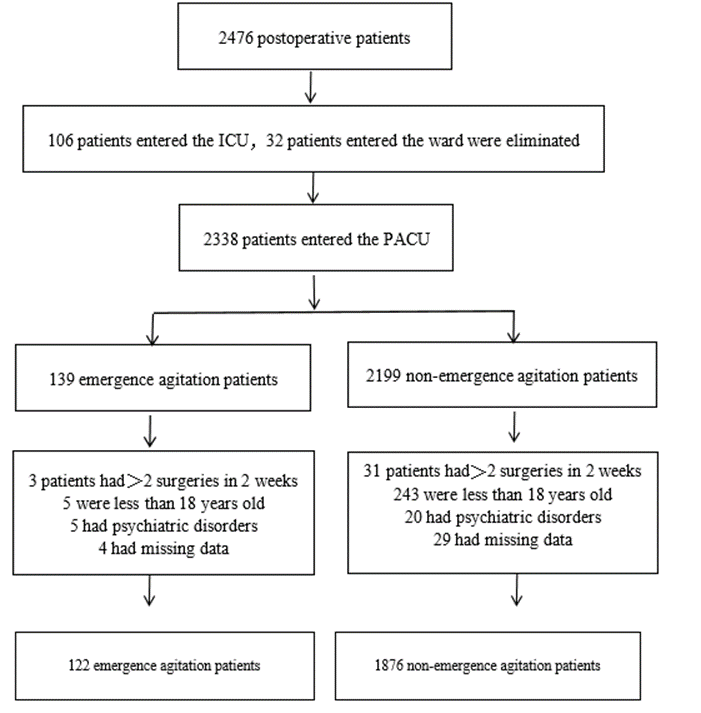
Figure 1: Flow chart of patients in this study. Data for study eligibility, screening, and exclusion were obtained from our institution. Patients who were admitted to the ICU after surgery or had psychiatric disorders, who underwent >2 surgeries in 2 weeks, who had missing data, and who were younger than 18 years old were excluded. ICU: intensive care unit; PACU: anesthesia recovery unit.
Analysis of Influencing Factors of Emergence Agitation
The results of univariate analysis for factors affecting postoperative agitation are shown in Table 1. It can be seen that gender (P<.001), age (P<.001), smoking and drinking history (P<.001), history of anesthesia (P<.01), cardiac function classification (P<.05), urinary catheter (P<.001), drainage tube (P< .001), nasogastric tube (P<.001), ASA classification (P<.005), postoperative hypothermia (P<.001), duration of tracheal intubation (P<.001), surgical method (P<.001), and postoperative pain (P<.001) were significantly different between the two groups. However, no significant differences were found between the groups in terms of BMI, history of anesthesia, blood transfusion history, and airway classification (all P>.05, Table 1).
Risk Factors for Emergence Agitation
With postoperative agitation during the recovery period after general anesthesia as the dependent variable, and the risk factors with statistical significance in the univariate analysis (gender,
age, BMI, smoking and drinking history, history of anesthesia, cardiac function classification, presence of indwelling urinary catheter, drainage tube, nasogastric tube, ASA classification, postoperative hypothermia, duration of intubation, type of surgery, postoperative pain, and analgesic method) as independent variables, a logistic stepwise regression analysis was performed. The results showed that age 60 -74 years, having a history of smoking and drinking, intubation duration >4 hours, postoperative indwelling drainage tube, type of surgery being urological surgery, postoperative hypothermia, and postoperative pain were the main influencing factors for the occurrence of agitation during the postoperative recovery period (P<0.05) (Table 2). All these factors were identified as risk factors, among which postoperative pain had the greatest risk for postoperative agitation (Figure 2).
|
Wald |
|||||
|
Item |
B |
SE |
P-value |
OR (95% CI) X2 |
|
|
Age (18-44 years as reference) |
|||||
|
60-74 |
0.444 |
0.23 |
3.721 |
0.054 |
1.560(0.993-2.450) |
|
Smoking and alcohol history (None as |
|||||
|
reference) |
|||||
|
Yes |
1.012 |
0.242 |
17.456 |
<0.001*** |
2.751(1.711-4.422) |
|
Intubation duration (0-2h as reference) |
|||||
|
4-6h |
1.17 |
0.256 |
20.818 |
<0.001*** |
3.222(1.949-5.325) |
|
≥6h |
1.655 |
0.316 |
27.465 |
<0.001*** |
5.231(2.817-9.713) |
|
Drainage tube (None as reference) |
|||||
|
Yes |
0.525 |
0.252 |
4.353 |
.037* |
1.691(1.032-2.769) |
|
Surgical type Abdominal as reference) |
|||||
|
Urological surgery |
0.63 |
0.256 |
6.08 |
.014* |
1.878(1.138-3.100) |
|
postoperative hypothermia (No as |
|||||
|
reference) |
|||||
|
Yes |
1.503 |
0.346 |
18.874 |
<0.001*** |
4.496(2.282-8.859) |
|
Postoperative pain (No as reference) |
|||||
|
Yes |
1.997 |
0.364 |
30.101 |
<0.001*** |
7.369(3.610-15.041) |
|
Model summary |
Method |
Forward: LR |
|||
|
Model |
χ²=226.833; df=9; P<0.001 |
||||
|
R2 |
0.291 χ²=4.644, P=.590 |
||||
|
H-L |
|||||
|
test,χ² |
|||||
|
B, regression coefficient; SE, standard error; OR, odds ratio; CI, confidence interval; H-L, Hosmer and Lemeshow test; df, degrees of freedom;R2, Nagelkerke R Square. *P<0.05 **P<0.01 ***P<0.001 |
|||||
Table 2: Logistic regression analysis results of agitation occurring during the resuscitation period after general anesthesia(N=1998).
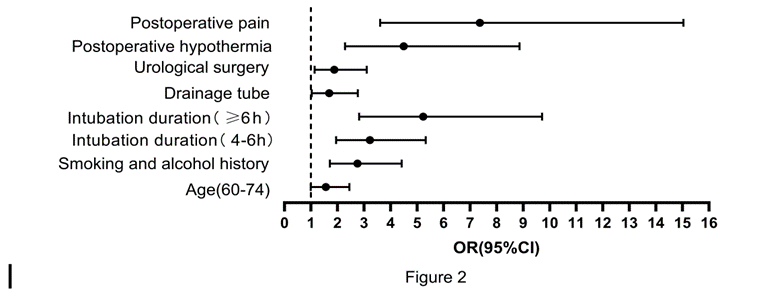
Figure 2: The greatest risk for postoperative.
Discussion
At present, the influencing factors of EA are not yet clear in clinical practice. It is generally believed that the central nervous system is inhibited to varying degrees by general anesthetic drugs, leading to reflexive resistance and abnormal consciousness [4, 6]. Among the 1998 cases included in this study, the incidence of this complication was 6.5%. The results of this study showed that a history of smoking and drinking, intubation duration>4 hours, postoperative indwelling drainage tube, urological surgery type, postoperative hypothermia, postoperative pain, and age of 60-74 years were risk factors for agitation during the recovery period after general anesthesia.
Analysis of Risk Factors for Agitation during the Recovery Period after General Anesthesia
A history of smoking and drinking is a risk factor for agitation during the postoperative recovery period. This may be related to the reduced function of the respiratory system, the impact on the circulatory system, and the decreased metabolic function. Smoking can affect the function of the respiratory tract, leading to coughing and increasing the likelihood of postoperative agitation [7]. The combustion of tobacco produces CO, and the nicotine stimulates the sympathetic and parasympathetic nerve ganglia, causing a series of physiological reactions that increase the probability of postoperative agitation [8]. Alcohol is metabolized by the liver, and alcohol dependence can reduce the patient’s liver metabolic function [9]. In this study, postoperative hypothermia was identified as a risk factor for postoperative agitation. This may be related to the slowed metabolism of anesthetic drugs and the disorder of body temperature regulation. A decrease in body temperature during surgery can affect the liver’s metabolic function of anesthetic drugs [10], leading to incomplete metabolism of anesthetic drugs within the corresponding time, increasing the risk of EA. The long-term exposure of the surgical site can affect the body’s temperature regulation function, leading to a decline in various bodily functions and increasing the risk of EA.
Intubation duration>4 hours is a risk factor for the occurrence of EA. The results showed that when the intubation time>4 hours, the OR value steadily increased, indicating that the longer the intubation time, the higher the incidence of EA. Tracheal intubation for more than 2 hours can cause edema of the tracheal mucosa, and local damage can cause discomfort, thereby increasing the risk of postoperative agitation [11].An increase in intubation time also leads to an increase in the dosage of anesthetic drugs used, thereby inhibiting the patient’s various bodily functions to varying degrees and reducing the patient’s metabolic function [12]. Urological surgery is a significant influencing factor, which may be related to hyponatremia and bladder irritation. The use of non-electrolyte fluids for irrigation during urological surgery can easily lead to hyponatremia, increasing the risk of postoperative agitation [13]. Most minimally invasive urological surgeries are performed through the urethra. When surgical instruments or urinary catheters enter the bladder through the urethra, they promote the release of inflammatory mediators, thereby causing or exacerbating bladder irritation. When patients wake up, the discomfort can cause agitation [14].
Postoperative indwelling drainage tube is also a significant risk factor for the occurrence of EA. Surgeries with postoperative indwelling drainage tubes cause greater surgical trauma. Moreover, patients are unconscious during this process. In the early stages of anesthesia recovery, patients’ reactions to sensations are in a hyper-sensitive state, and any uncomfortable stimulation can cause their agitated behaviour [15]. In addition, postoperative pain is also a significant risk factor for causing postoperative agitation, as postoperative pain can cause patients to have a reflexive resistance phenomenon, stimulating the patient’s central nervous system and causing symptoms such as moaning and agitation [16].
This study showed that age between 60-74 years was a nearly significant influencing factor (P = 0.054). Clinical experience has found that age is of great significance for postoperative agitation. The reasons are considered to be related to abnormal secretion of melatonin and the decline of various bodily system functions [17]. The older the age, the worse the physical condition, and the functions of the circulatory and respiratory systems also decline accordingly. Moreover, the pain tolerance is relatively lower than that of the younger group [18], At the same time, due to the decline of physical functions, patients are more likely to become anxious. [19], thereby increasing the occurrence of postoperative agitation. In the results of this study, patients aged 60 - 74 years were a risk factor for postoperative agitation, but the results for those aged ≥ 75 years were not significant. The reason may be that the sample size of this age group is relatively small, significantly lower than other groups, or it may be due to the stricter surgical and anesthetic management for the elderly. Some studies have shown that male patients, postoperative indwelling urinary catheters, ASA classification>II, and abdominal surgery are risk factors for postoperative EA [20], in this study; the above factors were not obvious. This may be due to the differences in the main surgical patients and surgical types conducted in different hospitals, or it may be that effective preventive measures were adopted for the above factors in this study, reducing the possibility of them becoming risk factors.
Measures to Prevent Agitation during the Recovery Period after General Anesthesia
Healthcare professionals should place emphasis on assessing patients’ age, history of smoking and alcohol use, postoperative body temperature, intubation duration, patients undergoing urological surgery, and postoperative pain. For elderly patients, it is essential to enhance intraoperative management and closely monitor various indicators. Preoperatively, pain threshold assessments can be conducted for patients, and for those with a low threshold, appropriate doses of analgesic drugs can be administered prophylactically. For patients with alcohol dependence, anesthetic drugs should be used judiciously, and drugs that are metabolized by the kidneys can be selected to alleviate the metabolic burden on the liver [9]. Patients with a history of smoking should be encouraged to quit smoking prior to surgery. For patients undergoing urological surgery, local anesthesia such as lidocaine ointment can be applied for surface anesthesia of the urethral orifice to reduce the likelihood of bladder irritation postoperatively [8], Preoperative communication and explanation should be thorough to prevent stress reactions during postoperative awakening. For patients with prolonged intubation, the surgical workflow can be optimized to minimize surgery time. The body temperature of patients should be closely monitored, and if a large volume of fluid needs to be infused during surgery, a fluid warmer should be used. After entering the recovery room, a warm air blower can be used for warming based on the patient’s body temperature, which can effectively enhance the metabolism of anesthetic drugs [21]. Stimulations to patients, such as suctioning and other irritating procedures, should be minimized.
Limitation
This study is a single-center investigation that only assessed factors related to the patient’s own condition, as well as intraoperative and postoperative factors that may influence postoperative agitation. However, preoperative factors that could potentially lead to postoperative agitation remain unknown. Future research could explore preoperative factors, patient psychological factors, intraoperative drug factors, and the qualifications of nursing staff. Additionally, while numerous factors contribute to postoperative agitation in patients under general anesthesia, the interrelationships between these factors warrant further investigation.
Conclusion
The occurrence of postoperative agitation in patients under general anesthesia is influenced by multiple factors, with age 60-74 years, history of smoking and drinking, intubation duration>4 hours, postoperative indwelling drainage tube, urological surgery type, postoperative hypothermia, and postoperative pain being the main risk factors. This suggests that nursing staff can strengthen the assessment of the above factors when receiving patients in the anesthesia recovery room, and predictively judge whether patients are at risk of EA; closely monitor patients’ postoperative vital signs, and provide effective nursing care, thereby reducing the incidence of postoperative agitation, improving the quality of awakening, and improving patient prognosis.
Reference
- Lee S, Sohn JY, Hwang IE, Lee HJ, Yoon S, et al. (2023) Effect of a repeated verbal reminder of orientation on emergence agitation after general anaesthesia for minimally invasive abdominal surgery: a randomised controlled trial. Br J Anaesth 130: 439-445.
- DeSouza IS, Thode HJ, Shrestha P, Allen R, Koos J, et al. (2022) Rapid tranquilization of the agitated patient in the emergency department: A systematic review and network meta-analysis. Am J Emerg Med 51:363-373.
- Bağcaz A, Ayhan A (2023) Emergence Agitation with EarthquakeRelated Traumatic Stress Symptoms after Intravenous Sedation. Turk Psikiyatri Derg 34:136-139.
- Lee SJ, Sung TY (2020) Emergence agitation: current knowledge and unresolved questions. Korean J Anesthesiol 73: 471-485.
- Medlej K (2021) Calculated decisions: Richmond Agitation-Sedation Scale (RASS). Emerg Med Pract 23: D3-D4.
- Wei B, Feng Y, Chen W, Ren D, Xiao D, et al. (2021) Risk factors for emergence agitation in adults after general anesthesia: A systematic review and meta-analysis. Acta Anaesthesiol Scand 65:719-729.
- Alexander D, Keogh B F (2005) Pathophysiology of respiratory disease and its significance to anaesthesia. Anaesthesia & Intensive Care Medicine. 6: 384-385.
- Darabseh MZ, Aburub A, Morse CI, Degens H (2024) The association between smoking/vaping habits and self-reported respiratory symptoms. Multidiscip Respir Med 19: 976.
- Liu Y, Xia Q, Ding Z, Gu L, Xu Y, et al. (2024) Prevalence and risk factors of low bone mineral density in Chinese Han male patients with alcohol dependence. J Int Med Res 52: 3000605241291759.
- Grote R, Wetz A, Bräuer A, Menzel M (2020) Short interruptions between pre-warming and intraoperative warming are associated with low intraoperative hypothermia rates. Acta Anaesthesiol Scand 64: 489-493.
- Li Y, Sun J, Cui K, Li J, Cai L (2024) Endotracheal Tube Cuff Deflation Methods Reduce Stress Response and Incidence of Postoperative Pharyngeal Complications in Patients Treated with Gynecological Laparoscopic Surgery. Ann Ital Chir 95: 801-808.
- Berger M, Neuman MD (2024) Anesthesia Dose and Delirium-A Picture Coming Into Focus. JAMA, 332:107-108.
- Chuang YH, Nandwani GM, Szewczyk-Bieda M Kernohan N, et al. (2022) Primary small cell carcinoma of the ureter with associated hyponatremia and rapid progression to bladder involvement: a case report. African Journal of Urology. 28:1.
- Chi J, Wu J, Lou K, Ma J, Wu J, et al. (2023) The systematic review and meta-analysis evaluated the efficacy and safety of nefopam for catheter-related bladder discomfort based on randomized controlled trials. Front Pharmacol 14:1305844.
- Ireland KC, Lalkhen AG (2024) Postoperative analgesia. Anaesthesia & Intensive Care Medicine. 25: 823-830.
- Moyano AJ, Moyano LC (2025) Perioperative pain management for appendicectomy: a systematic review and procedure-specific postoperative pain management recommendations. Eur J Anaesthesiol 42: 80-81.
- Kalkan KT, Esrefoglu M, Terzioglu-Usak S, Yay A (2024) Protective effect of melatonin on blood-brain barrier damage caused by Endotoxemia. Neurol Res 46:195-206.
- Rajput K, Ng J, Zwolinski N, Chow RM (2025) Pain Management in the Older Adults: A Narrative Review. Clin Geriatr Med 41:131-151.
- Liu Q, Li L, Wei J, Xie Y (2023) Correlation and influencing factors of preoperative anxiety, postoperative pain, and delirium in elderly patients undergoing gastrointestinal cancer surgery. BMC Anesthesiol 23:78.
- Song SS, Lin L, Li L, Han XD (2024) Influencing factors and risk prediction model for emergence agitation after general anesthesia for primary liver cancer. World J Gastrointest Surg 16: 2194-2201.
- Alkan B F, Meyanci K G, Bulut A, Sengul I (2024) Intraoperative Patient Warming Instead of Gas on the Management of Postoperative Pain in Laparoscopic Colectomy and Cholecystectomy: A Randomized Controlled Trial. Cureus. 16: e57989.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.