A Collaborative Healthcare Response to The Mpox Epidemic: Lessons from A Nurse–Assistant–Physician Triage and Vaccination Model in France
by Benjamin Davido1,2*, Nadege Letilly1, Vinciane Philippe1, Malika Bouzerara1, Morgane Leminoux1, Celine Delhoum de Castro1, Beatrice Touraine1, Carla Amorim1
1AP-HP, Raymond-Poincaré Hospital, Garches, France
2University of Versailles-Saint-Quentin, Paris Saclay University, UMR 1173, Versailles, France
*Corresponding author: Benjamin Davido, AP-HP, Raymond-Poincaré Hospital, Garches, France
Received Date: 15 November 2025
Accepted Date: 24 November, 2025
Published Date: 27 November, 2025
Citation: Davido B, Letilly N, Philippe V, Bouzerara M, Leminoux M, et al. (2025) A Collaborative Healthcare Response to The Mpox Epidemic: Lessons from A Nurse–Assistant–Physician Triage and Vaccination Model in France. Int J Nurs Health Care Res 8:1682. https://doi.org/10.29011/2688-9501.101682
Abstract
During the 2022 Mpox outbreak in France, a nurse–assistant–physician triage model was implemented at Raymond-Poincaré Hospital to optimize screening and vaccination. This pre-post evaluation compared July–August 2022 operational metrics and staff perceptions. Vaccinations increased by 235%, while screenings declined as activities shifted toward prevention. Staff reported lower workload (p=0.05) and improved collaboration (p<0.01) after workflow reorganization. Qualitative feedback highlighted enhanced coordination and morale. The model demonstrated that nurse-led task sharing improves outbreak response efficiency and workforce resilience. Findings support expanding Advanced Practice Nurse (APN) roles in infectious disease management and integrating structured feedback systems for future epidemics.
Keywords: Mpox; Epidemic preparedness; Nurse-led triage; Teamwork; Vaccination; France
Introduction
The 2022 Mpox outbreak, driven by the clade IIb variant, rapidly expanded beyond its historically endemic regions in Central Africa to affect large parts of Europe and North America [1]. France became one of the most affected countries and responded by establishing dedicated Mpox screening and vaccination centers across selected hospitals. These measures built upon structural innovations introduced during the COVID-19 pandemic, such as mass testing logistics and decentralized vaccination hubs. Simultaneously, France was formalizing the role of Advanced Practice Nurses (APNs), a category legally recognized in 2016 and deployed operationally since 2019 [2,3]. However, the scope of APNs remained restricted, primarily limited to chronic disease management, and did not yet include infectious disease coordination, in contrast to practices observed in the U.K. and the U.S., where APNs were active contributors during previous outbreaks including Ebola and COVID-19 [4,5].
To support a more adaptive and scalable epidemic response, the French health authority issued Directive DGS-Urgent No. 2022_58 in June 2022, allowing nurse-led Mpox vaccination under emergency conditions [6], echoing earlier COVID-19 decrees authorizing broader nurse responsibilities [7]. Given this evolving policy context and the need for decentralized and efficient care structures, we implemented and assessed a novel triage model involving nurse assistants, registered nurses, and physicians. The primary objectives were to measure operational impact, vaccination throughput and screening volume and to capture the lived experience of frontline staff. These insights are timely in light of the 2024 resurgence of Mpox in the Democratic Republic of Congo, where more than 21,000 cases of clade I infections have been reported as of June 2025 [8], reaffirming the importance of preparedness in non-endemic regions.
Methods
The study was conducted at Raymond-Poincaré Hospital (AP-HP, Garches, France), a tertiary referral center with prior involvement in pandemic response. The Mpox triage and vaccination unit operated from July to August 2022 on weekdays between 9 a.m. and 5 p.m. The clinical pathway was structured into two main physical areas: a medical evaluation and vaccination room operated jointly by nurses and physicians, and a separate administrative intake zone managed by nurse assistants. Patient appointments were centralized through a dedicated telephone hotline and institutional email system, facilitating structured scheduling and flow control.
A pre-post design was adopted, comparing key metrics from July (baseline) to August (post-intervention). Quantitative data on vaccination numbers, screening activity, incoming calls and emails, and patient geographic origins were logged in the Orbis electronic medical record platform (Dedalus Healthcare Systems Group, Bonn, Germany). The model’s operational efficacy was supplemented by qualitative and quantitative staff feedback. A sixmonth post-intervention survey was distributed to 21 non-medical staff members involved in the intervention (9 in July and 12 in August). The questionnaire included Likert-scale items (assessing workload, collaboration, stress, and willingness to re-engage in future outbreaks) as well as open-ended questions regarding perceived challenges, strengths, and suggestions for improvement. Survey validity was tested in a pilot group of 5 staff (Table 1).
Please circle or highlight the items that apply to you.
Demographic Data:
- Age: ________
- Gender: F / M
- Role: Nurse (IDE) / Nurse Assistant (AS) / Administrative Assistant (AMA)
- Period of participation: July / August
1. How did you feel during this period?
- Enthusiastic
- Educational / Knowledge-enhancing
- Challenging
- Apprehensive
- Under pressure
- Other: _______________________
2. What organizational difficulties did you face?
- Rapidly changing guidelines
- Work overload
- Reception area not adapted to patient volume
- Insufficient human resources
- Other: _______________________
3. Facing a new epidemic, how would you feel?
- Ready to participate again enthusiastically
- Willing to participate if working conditions improve
- Apprehensive / Reluctant
- No longer willing to participate in epidemic response
- Other: _______________________
- ____________________ / ____________________ / ____________________
- Easy, not a hindrance
- Time-consuming
- Too many tools/platforms
- Required multitasking
- Other: _______________________
6. What did you take away from this experience?
- Difficulty switching between testing and vaccination
tasks
- For AS: unable to test or vaccinate
- Inspired interest in developing a nurse/assistant vaccination protocol
- Felt effective and contributed to vaccination campaign
- Other: _______________________
7. How would you describe the collaboration between medical and non-medical staff?
- Efficient
- Unique
- Rapid
- Mutual
- Imperfect
- Other: _______________________
8. Would you like to leave a personal comment?
Table 1: Staff questionnaire
Responses were manually coded for thematic content, and Fisher’s exact test was used for statistical comparisons (p<0.05), in consideration of the small sample size. Ethics approval was not required as the intervention was conducted under the legal framework of public health emergency response (Article L31311, French Public Health Code). No identifiable patient data were collected for research purposes, and all records were anonymized.
Results
Over the two-month period, 1,965 patient contacts were recorded, comprising 1,516 in July and 449 in August. A total of 610 appointment requests were received, 9% of which were not fulfilled. The majority of patients (96%) self-identified as men who have sex with men (MSM), with a mean age of 41±12 years. Most patients were from the Paris metropolitan area (n=344) and the local department (n=249), with others coming from different regions of France.
Vaccination activity increased by 235% from July to August (145 to 341 vaccinations), while the number of Mpox screenings declined from 42 to 28 (-66%) as illustrated in Figure 1A. This shift reflects a transition from diagnostic surveillance toward mass preventive vaccination.
Among the 21 survey participants (9 in July, 12 in August), staff in August reported significantly lower perceived workload. In July, 5 out of 9 (55.6%) respondents described their workload as “high,” compared to only 1 of 12 (8.3%) in August (p=0.05). Perceived collaboration with physicians also improved markedly— from 22.2% in July to 83.3% in August reporting positive interprofessional dynamics (p<0.01). Willingness to re-engage in future outbreak responses was also higher in August, where 9 of 12 respondents (75%) expressed enthusiasm without preconditions, compared to 8 of 9 (88.9%) in July who would re-engage only if specific conditions (such as better protocols) were met (p=0.02).
Qualitative feedback revealed stark differences in experience. In July, staff reported confusion due to daily-changing protocols, multitasking pressure, and inter-role tensions. In contrast, August respondents highlighted smoother workflows, better task distribution, and enhanced patient cooperation. A word cloud generated from open-ended responses (Figure 1B) identified key recurring descriptors: “demanding,” “formative,” “collaborative,” and “effective.”
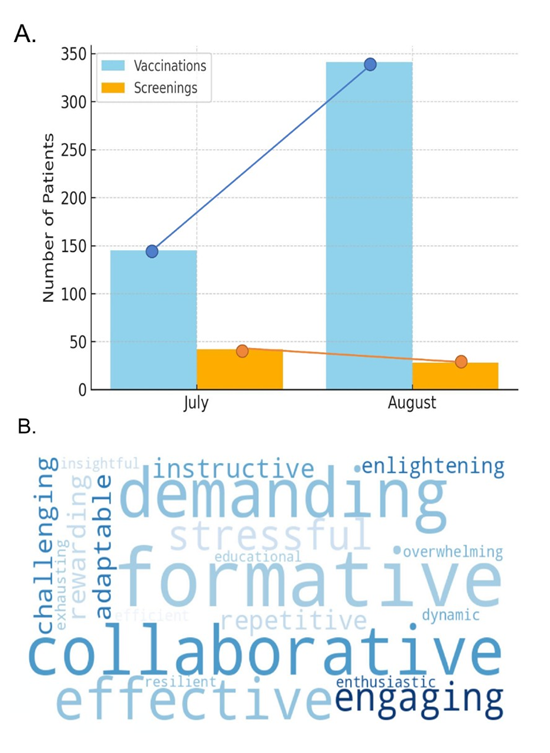
Figure 1: A. Monthly Trends in Mpox Vaccination and Testing (July-August 2022). B. Keywords Used by Staff to Describe the Mpox Consultation Experience (Word Cloud).
Discussion
This decentralized triage and vaccination model proved operationally efficient and was positively received by staff, particularly after process improvements were implemented. The structured redistribution of tasks led to a significant increase in vaccination capacity, a decrease in perceived burden, and enhanced physician collaboration. These results mirror international examples where nurse-led efforts in the U.S where Mpox vaccination clinics demonstrated task-sharing efficacy [9] and in the UK, where clear communication during the COVID-19 campaign helped reduce vaccine hesitancy [10]. The model also offers valuable lessons in workforce management. Staff feedback collected six months post-intervention revealed improved morale, clearer interprofessional communication, and willingness to reengage-critical factors in sustaining healthcare operations during prolonged outbreaks. The use of visual tools such as word clouds helped capture staff perceptions in a dynamic and digestible format, adding an innovative feedback dimension that is seldom reported. In contrast, Alquwez [11] highlighted staff nurses’ adaptive leadership and lessons learned during COVID-19, focusing exclusively on quantitative outcomes.
Our findings remind us that the current epidemiology advocates for infection prevention and control [12], and thus infectious disease staff must be prepared in time for the next epidemic that occurs sooner or later. Although APNs were not directly involved in this response, the success of this nurse-led model supports future integration of APNs into outbreak coordination roles. Given the legal recognition of APNs since 2019, expanding their scope to include infectious disease and emergency response would align with broader EU policy goals. The 2023 European Nurse Staffing Directive aims to upskill 50% of the nursing workforce by 2030 [13], and experiences like ours underscore the feasibility and benefits of this approach.
Indeed, the demographic shift in the healthcare workforce also demands urgent attention. With a large proportion of experienced nurses nearing retirement, and a limited pipeline of young professionals, especially in rural areas [14]. Therefore, creating meaningful, resilient roles for nurses is essential, including psychosocial support, investment in epidemic-specific training, and structured team feedback systems to promote retention.
Conclusion
The nurse–assistant–physician triage model successfully addressed key challenges of the 2022 Mpox epidemic in France, improving vaccine throughput and staff collaboration while highlighting the potential for broader APN involvement. By integrating scalable operational processes with innovative feedback tools, this approach offers a replicable model for future outbreaks. Policy actions should focus on expanding APN scope, providing emotional and logistical support to frontline teams, and embedding structured training and communication tools within epidemic response frameworks.
Acknowledgments
We would like to thank all the staff from the infectious diseases department
Author Contributions
Study design: BD, CA, BT, Data collection: NL, VP, MB, ML, CDC, Data analysis: BD, BT, CA, Study supervision: CA, Manuscript writing: BD, Critical revisions for important intellectual content: BT, CA and BD
Data Availability
Data are available upon reasonable request from the corresponding author.
Informed Consent
Informed consent was not gained from patients involved in this outbreak. All patients were treated according to clinical judgement and infection control practices in order to treat them and control the outbreak according to local guidelines. Patients did not undergo randomisation or intervention for the purpose of this report. Data has been analysed and presented anonymously.
This work was presented at the French National Infectious Diseases Days (JNI) in Grenoble in June 2023.
Grants/Funding: None
References
- Kraemer MUG, Tegally H, Pigott DM, Dasgupta A, Sheldon J, et al. (2022) Tracking the 2022 monkeypox outbreak with epidemiological data in real-time. Lancet Infect Dis 22:941-942.
- Devictor J, Burnet E, Henriot T, Leclercq A, Ganne-Carrie N, et al. (2023) Implementing advanced practice nursing in France: A countrywide survey 2 years after its introduction. Nurs Open 10:1437-1448.
- De Rosis C, Duconget L, Jovic L, Bourmaud A, Dumas A (2024) The deployment of advanced practice nurses in the French health system: From clinics to professional networks. Int Nurs Rev 71:362-374.
- Maier CB, Aiken LH (2016) Task shifting from physicians to nurses in primary care in 39 countries: A cross-country comparative study. Eur J Public Health 26:927-934.
- Kleinpell RM, Grabenkort WR, Kapu AN, Constantine R, Sicoutris C (2019) Nurse Practitioners and Physician Assistants in Acute and Critical Care: A Concise Review of the Literature and Data 2008-2018. Crit Care Med 47:1442-1449.
- Haute Autorité de Santé - Avis n°2022.0034/SESPEV du 20 mai 2022 du collège de la Haute Autorité de santé relatif à la vaccination contre Monkeypox n.d.
- Décret n° 2021-384 du 2 avril 2021 modifiant les décrets n° 2020-1262 du 16 octobre 2020 et n° 2020-1310 du 29 octobre 2020 prescrivant les mesures générales nécessaires pour faire face à l’épidémie de covid-19 dans le cadre de l’état d’urgence sanitaire - Légifrance n.d.
- Outbreak of mpox caused by Monkeypox virus clade I in the Democratic Republic of the Congo n.d.
- Thornhill JP, Barkati S, Walmsley S, Rockstroh J, Antinori A, et al. (2022) Monkeypox Virus Infection in Humans across 16 CountriesApril–June 2022. New England Journal of Medicine. 387: 679-691.
- Pennisi F, Genovese C, Gianfredi V (2024) Lessons from the COVID-19 Pandemic: Promoting Vaccination and Public Health Resilience, a Narrative Review. Vaccines (Basel).12: 891.
- Alquwez N (2025) Adapting Nursing Care During the COVID-19 Pandemic: Staff Nurses’ Experiences, Lessons Learned, and Implications for Nursing Management. J Nurs Manag 2025: 6178630.
- Health Emergency Preparedness and Response (HERA) - European Commission n.d.
- De Raeve P, Bolzonella F, Davidson PM (2022) A Theoretically Derived Approach to Impact: Implementing Policy Influence Strategies. Policy Polit Nurs Pract 23:150-161.
- Greenley R, Aiken LH, Sermeus W, et al. (2024) Strengthening Europe’s Nursing Workforce: Strategies for Retention [Internet]. Copenhagen (Denmark): European Observatory on Health Systems and Policies; (Policy Brief, No 66) POLICY BRIEF 2024.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.