A Case Study in Implementing Integrated Care for Older People in Ireland; Getting from Complex Challenge to Complex Adaptation
by Patrick Harnett1*, Peter Williams2, Cathal Heavey2, Siobhan Kennelly1, Dei Conroy1, Des Mulligan1, Jennifer Hardiman1, Sarah Barry3
1Health Service Executive, Ireland
2University of Limerick, Ireland
3Royal College of Surgeons, Ireland
*Corresponding author: Patrick Harnett, Health Service Executive, Ireland.
Received Date: 27 October, 2023
Accepted Date: 02 November, 2023
Published Date: 05 November, 2023
Citation: Harnett PJ, Williams P, Heavey C, Kennelly S, Conroy D, et al. (2023) A Case Study in Implementing Integrated Care for Older People in Ireland; Getting from Complex Challenge to Complex Adaptation. Int J Geriatr Gerontol 6: 171. DOI:10.29011/2577-0748.100071
Abstract
Introduction: With people living longer and associated increased multi-morbidity and social care needs, implementing a change in balance was required between the prevalent hospital-focused model designed for acute episodic care, and longitudinal, population-based care. ‘Barometric’ indicators such as emergency department attendance, self-referrals, and trolley waits for those aged 75+ indicated poorer outcomes rooted in this mismatch and fragmentation. History indicated fragmentation to be persistent. Integrated Care was proposed as a policy solution, but systemic examples in practice were limited. Integrated care faces two challenges: it is polymorphous, with confusion over objectives among different actors and stakeholders; health and social care occurs within a complex adaptive system, complicating any change of the magnitude required. Methods: Adopting an Action Research methodology, a programme to design and test a systemically scalable model of integrated was led by the author. A literature search addressed two simultaneous question: (1) what were the key ingredients required to integrate care for older persons, and (2) what is a more-effective methodology to support systemic implementation. Consensus on the first, but not on the second, and drawing on the balanced socio-technical perspective of Greenhalgh et al. (2004), led to a research hypothesis that a framework methodology incorporating ‘hard edges’ and ‘soft edges’ identified in the literature would solve this ‘wicked problem’ in practice. Literature review yielded five key ingredients: Personal/ Professional, Culture, Process, Leadership, Organisational. In multiple rounds of collaboration with practitioners, a resultant 10-Step Framework was evolved, incorporating elements including governance, population planning, mapping resources, service/care pathways, new ways of working, MDT/hub, personcentred planning and delivery, supports to live well, monitoring/evaluation, and national enablers on workforce, IT, finance. It functioned as both conceptual model and implementation roadmap, and was mobilized at six pioneer sites, later thirteen, in tandem with a choreographing methodology which included communicating vision, and a deep and active programme of engagement in loco, networking events, and timely key metrics, with a core principle of ‘direction without dictat’. Results: A mix of quantitative and qualitative data was collected over two years, including surveying the utility of the framework to participant actors, and capturing and presenting timely data on emergent care-process performance. The framework has shown a high degree of utility to the local clinical and managerial leaders tasked with implementation. Pioneer sites demonstrated fidelity to the model, improving access and efficiencies. Site specific changes included bed use saving (1,000 bed days), reduced length of stay (2-5 days) and improved access (49% seen within 7 days), and growth in multi-disciplinary teams (101 posts) and age attuned pathways (45). Conclusions: The contribution of the work is to provide a means of bridging the intent-realization gap in systematic implementation within the complex adaptive system that delivers older persons health and social care. It facilitates balance between latitude and prescription, emergence and fidelity, especially for high autonomy actors tasked with implementation in a context of professional regulation and accountability on the one hand, and the lived experience of older population on the other. In consonance with Action Research, further research on discrete aspects are identified.
Keywords: Older People, Integrated care, Systemic change
Introduction
The Integrated Care Programme Older People (ICPOP) in Ireland was established in 2016 to design and test a new model of integrated care for older persons. The context included demographic pressures and an acute hospital-centric care system, unattuned to the needs of older people whose complex care needs highlighted problems with access and fragmentation leading to sub-optimal outcomes. The proposed model needed to be scalable nationally but two immediate challenges were identified. Integrated care is a polymorphous concept whose lack of conceptual clarity was described as a modern day Tower of Babel [1] with differences in interpretations amplified in inter-sectoral and interdisciplinary discussion. The second challenge involved implementing systemic change in health systems [2-12]. Limited evidence existed on how to implement integrated care models that supported front line clinical and managerial leaders whose focus on the ‘day job’ limits their capacity (knowledge, time, resource) to deliver the desired change. This paper describes how ICPOP addressed the implementation challenge using a 10 Step Framework in tandem with an implementation methodology that builds on insights into systemic change in health systems. A revised version of the framework is presented post utilisation in the field and a conceptual schema is offered that address the implementation challenge.
Background
Demographic aging in Ireland, as in other countries, leads to associated increased multi-morbidity and social care needs. Barometric’ indicators such as access block, emergency department patient experience times and associated trolley waits for those aged 75+ indicate system fragmentation and poorer outcomes. A rapid review of integrated care for older people highlighted some key findings that supported it as a policy solution [13-19]. It also has a body of supportive evidence in improving health and social care outcomes [20-26], decreasing carer burden [27] and improving efficiency and effectiveness of service provision [28-30]. Growing evidence on ‘what works’, in improving discrete aspects of care for older persons [31-37] included;
- bespoke care pathways,
- multidisciplinary teams working in the community
- a case management approach.
However, implementing a new model of care focused on longitudinal, population-based care is a substantial organizational, cultural and professional challenge. A parallel review of the literature on systemic change highlighted five key domains [38] to be simultaneously addressed in order to meet the following implementation challenge;
- There is uncertainty about ‘what works’ at a systemic level outside of closed systems [39-43]
- “The scale and complexity of implementing integrated care can easily overwhelm even strong leadership and project management…” [44]
- It generally takes 2 years to bed-in a new model of this type and 7-10 for it to mature and 3-5 years to implement and yield the desired change [45,46].
- Deficiencies of consistency, fidelity and complexity of attribution, and random confounding external effects where variables cannot be controlled [47].
- It takes a substantial amount of time for demonstrable patient/ population outcome effects s to emerge [48].
- Complexity of accurate costing and value determination across the health system.
Theoretical considerations
A synthesis of findings [49] indicate that conventional methods of health system change, presented as scientifically rational within a linear, reductionist epistemology, [50-53] are compelling when using high reliability industries as a point of reference. However, difficulties in getting evidence into practice in a stepwise fashion indicate a need for a paradigm shift. Traditional research designs are problematic in complex and dynamic human systems whose social forces make certainty unattainable [54]. Over the past 20 years, research on change in health systems has begun to apply complexity theory [55-58]. This recognizes that the collective activities and relationships between a large numbers of autonomous agents in complex adaptive systems (CAS) give rise to inherent unpredictability which are not necessarily replicable in the same way in a different local context. This recognizes that healthcare organizations contain multiple, diverse and interconnected elements whereby the analogy of a living organism rather than a machine was more appropriate in reflecting the complexity dimension. As a consequence, complexity science embraces a rich mix of anthropology, sociology and organizational psychology [59-61]. Consequently, the need to reframe the approach to improvement as a social problem, most effectively addressed through a professional “grassroots” movement is a fundamental methodological starting point. This means that structures, leadership and process are essential but not sufficient for systemic improvement. These ‘hard edges’ [62] have to be framed within a common sense of purpose and meaning which capitalizes on trusted personal/professional networks and sets improvement within a sociological context. This is a key differentiation, as the behavior of agents within a CAS is heavily influenced by social rules [63]. Consequently, change methodologies need to provide social nudges rather than programmatic management which recognize that change is embedded in complex social systems, whose actors are highly autonomous and whose views are influenced by powerful, shared professional narratives.
Conceptual frameworks in use
One approach to support implementation is the use of frameworks. A review of integrated care frameworks [64] identified conceptual frameworks describing the key features of integrated care. The evolution of integrated care frameworks included [65] five laws of integrated care, [66] ‘domains’ of integrated care and [67] philosophical and policy pre-requisites and care management components. A more contemporary and comprehensive review, Project INTEGRATE [68] presented a compendium of strategic policy direction statements [69,70]. In addition, the Rainbow Model of Integrated Care, (RMIC), [71], is a well-established conceptual framework, describing integration at three ‘levels’ (Macro, Meso and Micro). Furthermore, the Developmental Model of Integrated Care (DMIC) [72] describes discrete conceptual elements of integration care across four distinct phases; initiation and design, experimentation and execution, expansion and monitoring, consolidation and transformation.
Utilizing a 10 Step Framework to frame and mobilize implementation
The early development of a 10 Step Framework to support implementation for ICPOP emerged from a literature review [40] and underwent a series of iterations through feedback from pioneer sites, clinical programme staff, experts in the area of public health, gerontology, system change experts and service users. In tandem with an iterative co-productive process, the use of a framework as a means of implementation draws on a rich range of interdisciplinary insights in social psychology. This includes including positive psychology [73], organizational development [74], social cognitive theory [75,76], solution focused approaches , motivational theory [77] and established social-technical theory [78]. The working hypothesis was that a framework that combined ‘hard and soft edges’ would give structure to implementation [79] and allow for the complexity of the challenge that simultaneously addressed philosophical, practice and organizational issues [80].
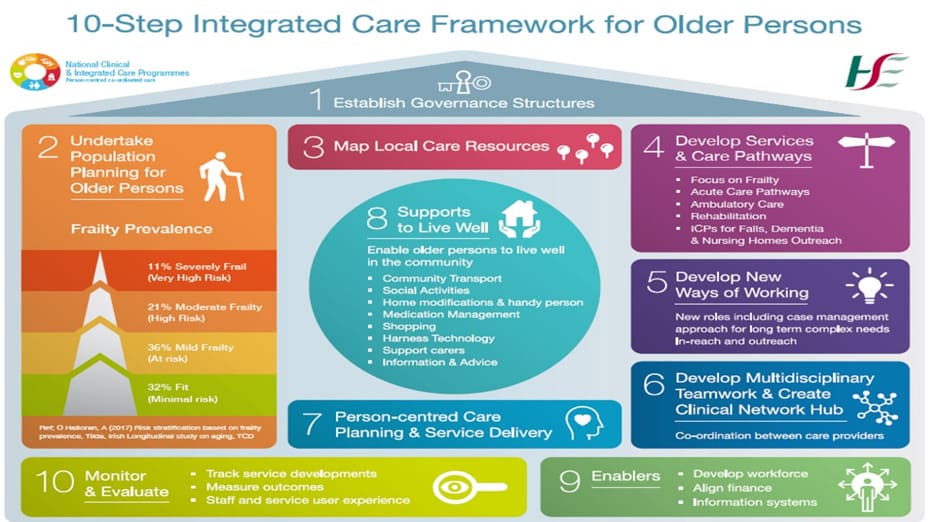
Figure 1: Whilst founded on the 10 Step Framework, the ICPOP teams’ approach used a 5 step approach to support redesign of older person services when working with pioneer sites [91]. This involved a series of engagements as outlined inFigure 2.
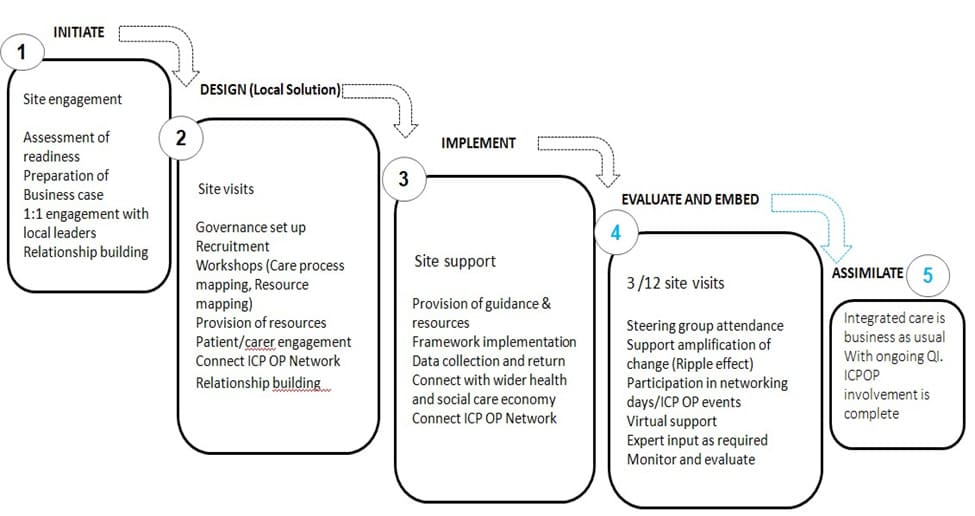
Figure 2: 5 step approach to local implementation.
ICPOP supported the development of aspiring pioneer site business-cases (pre-initiation) as a means of testing intent, capacity and commitment which required local executive sponsorship that underpinned local sustainability and strategic scaling of the project. Beyond this initiation stage, ICPOP facilitated local care pathway mapping. This dynamic, hands-on process involved ICPOP in locus with the local leadership team, service users/carers and the wider ecosystem of health and care (including local authority and NGOs) as partners in the process. This (patient) journey mapping exercise highlighted duplication of effort and roles with resultant loss of value for all involved in established practice. It strengthened the case for change, identified priority pathways and publicly committed all involved. This surfaced their contribution to the change and enabled care pathways to become more coherently designed. This (initiation and design) process was not dependent on substantial investment, ‘softened up’ the potential for change, secured leadership commitment and allowed a different narrative to be introduced (e.g. ‘perhaps we can do more with what we have’ or ‘actually we have a lot of the resources we need but they are not coordinated’). The engagement process allowed ICPOP to operate in an insider/outsider capacity thus acting as a catalyst for change whilst challenging assumptions. The mapping process also allowed local leaders to publicly articulate a shared vision of the future service model for older people which inevitably challenged institutional ‘silos’ thus allowing a focus on solution-focused objectives.
Bespoke events such as speed networking allows local agencies to engage with one another. This served a pragmatic purpose (sharing information), built capacity and reinforced the multi-agency aspect of integrated care. In addition, it sent a psychological signal as to the importance of the work for all involved. The programme actively promoted the inclusion of service users in co-producing the future state pathways. This diluted professional agendas and legitimised aspects of service design important to service users. As a consequence, pioneer sites had service user representatives/patient champions sitting on local governance groups. Finally, data was collected from all pioneer sites that supported future investment locally and nationally, drawing on lessons learned. This process of ‘building the road as one travels on it’ allows for greater efficiency and local ownership.
All of these five sequential steps involved the ICPOP team as a whole as well as a dedicated ICPOP Service Improvement Manager (SIM) working with local sites. The SIM worked closely with the local project lead(s), to establish local governance, provide practical support (e.g. ICT hardware) or support emergent initiatives. This relationship management was critical to local success, acting as a facilitator, challenging thinking, engaging service users, promoting fidelity to the framework, mobilizing national resources as well as providing psychological support including peer support and formal networking days.
Findings
A full description of the results is beyond the scope of this paper and addressed elsewhere but a sample of findings are offered to give an overview of the early impact. These reflect the fact that the 10 Step Framework was one component within the broader methodology adopted by ICPOP. In assessing the reliability of the 10 Step Framework, the internal reliability for each latent variable within the framework was assessed using Cronbach’s Alpha (Table 1). This measure indicates how well each indicator ‘hangs’ together within a single construct. A Cronbach’s alpha of at least 0.7 indicates good internal consistency for a set of indicators.
|
10 –Step Framework |
Number of Indicators |
Chronbach’s Alpha value CA |
|
Governance |
3 |
.905 |
|
Population Approach |
3 |
.6002 |
|
Mapping Existing Resources |
3 |
.726 |
|
Care Pathways |
3 |
.702 |
|
Case management |
3 |
.872 |
|
MDT Working |
5 |
.754 |
|
User Input |
3 |
.839 |
|
Collaboration |
2 |
.2463 |
|
Technology |
3 |
.6422 |
|
Measurement |
4 |
.718 |
Table 1:10 Step Framework, assessing internal reliability
- Cronbach’s Alpha – Ought to exceed 0.7 for good internal consistency
- Mean inter-item correlation is within the acceptable range of .2 to .4 (when CA fails to achieve 0.70)
- Constructs with a small number of items often fail to exceed 0.7
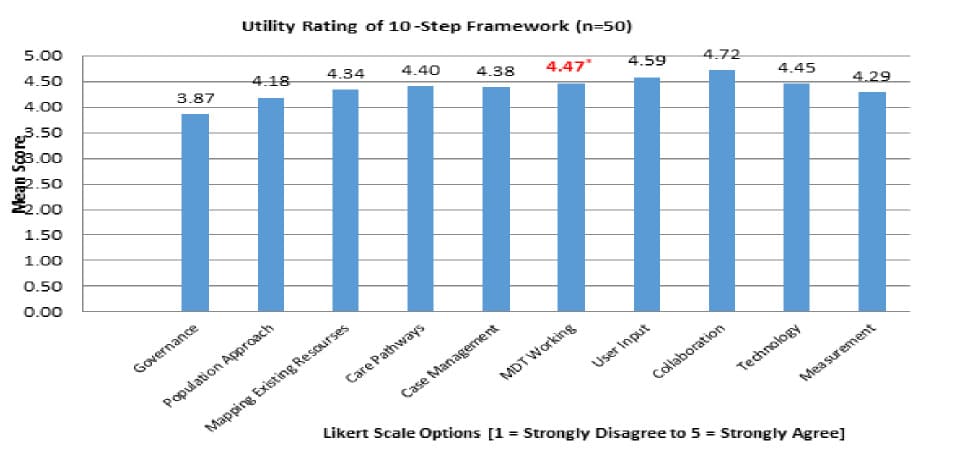
Table 2: Utility of 10-step framework: All participants.
In tandem with the frameworks reliability, its utility was evaluated with clinical leaders and managers. Much is made of the gap between managerial and clinical worldview [81] with assumed loyalties. However, in terms of the constructs within the 10 Step Framework, observed differences were deemed mostly compatible. The survey results indicate that the framework has utility in implementation and the constructs within the 10 Step Framework as having validity. This is supported by the respondents understanding of the intention of the constructs within the framework. Their responses validated the reliability of the constructs as representing the right combination of elements.
It has to be acknowledged that the 10 Step Framework was a new conceptual framework which challenged many of the established way of working. Participants for example were invited to consider new models of shared governance that challenged the familiarity of working in their respective clinical and managerial areas. Where minor difference surfaced this was unsurprising as participants in pioneer sites had to consider how shared authority and decision making operated and to set aside institutional interests in favour of the population needs. In addition, working within multidisciplinary teams, whilst again not unfamiliar, posed a different challenge when working outside the familiar comfort of institutional structures and settings.
From a service perspective, a sample of early data in (2017/18) indicated 6,050 new referrals were received by pioneer sites resulting in 3,530 Comprehensive Geriatric Assessments. 49% of patients were seen within seven days of referral. In order to coordinate care and develop services coherently, seven pioneer sites established an integrated care team ambulatory hub, with five more having plans underway at the time. In terms of service impact, significant positive service impact was observed, as evidenced from a selection of data from selected pioneer sites (n=4) comparing 2016 v 2017 and 2017 v 2018:
|
Indicator |
Change (2016 v 2017) (reduction) |
Notional savings |
|
AvLos |
(2.6 days) or (22%) |
€3.2m |
|
Bed days saved ( Hip Fracture) |
(5.6 days) or (1,000 bed days) |
€0.842m |
|
Bed days saved (Medical Bed) |
(3,938) |
€3.34m |
|
Readmissions within 28 days |
3% (national average in same period =9.8%) |
|
|
Admissions 85yrs+ |
(34%) |
€1.3m |
|
Total |
€8.7m |
Table 3: Sample of pioneer site impacts
In the selected pioneer sites (Table 3), a total of €1.1m invested was shown to yield a return on investment of €8.7m in terms of notional savings based on bed-days saved or admissions avoided. The early evidence in pioneer sites arguably points to significant return on investment when local leaders (clinicians and managers) have the autonomy to redesign services.
National saving are in terms of incremental efficiencies gained rather than in any increased revenue
A closer examination of data from one pioneer site (A), attributable to the establishment of an ambulatory hub, was especially encouraging when compared with another site (B) which operated a more ‘peripatetic’ MDT model. It is interesting to note that despite an increase in attends (14.4%) for people aged 75-84yrs in pioneer site A, admission rates reduced by 2.5% (75-84yrs) when comparing Jan 2018 v 2019. Pioneer site B saw attends (9%) and admission rate increase (3.2%) in the same period (Table 4). This suggests that there is a tendency to default to admission in pioneer site B when people use an acute hospital as a point of access and suggests that the availability of ambulatory alternatives to hospitalization in pioneer area A and reduces the likelihood of admission.
|
Pioneer site B |
Pioneer site A |
|||||
|
Jan 2018 |
Jan 2019 |
% Change |
Jan 2018 |
Jan 2019 |
% Change |
|
|
Attendance 75+ yrs |
864 |
942 |
9.0% |
555 |
635 |
14.4% |
|
Admission rate 75+ yrs |
53.3% |
56.1% |
3.2% |
49.3% |
48.0% |
-2.5% |
|
Admission rate 85+ yrs |
56.2% |
56.4% |
0.4% |
60.6% |
53.2% |
-12.3% |
|
Unscheduled returns 75+ yrs |
0% |
0% |
- |
6.1% |
5.0% |
-17.5% |
Table 4: Comparison of 75+yr attends and admits: B v A
Revising the 10 Step Framework in the light of emergent use
As the experience of implementation evolved and as a second cycle of pioneer sites came on stream from 2017 to 2019, the ICPOP team gained further insights into the sequencing of implementation steps. The second cycle of implementation provided the opportunity for a more nuanced approach, without changing its fundamental components.
The updated version of the framework (Figure 4) sets out the ‘arrived’ condition of the framework based on this initial cycle. The original framework still stands as a reference model for programme embarking on a comparable implementation campaign in another health/social care setting.
Discussion
In deploying change, the importance of adaptable approaches coupled with autonomy on the part of participants’ decision making, facilitates implementation as an ‘adaptive and self-organising’ approach. This allows for emergence and grounds implementation within a series of feedback loops rather than a linear process. This reflects the healthcare context as one of ‘complexity’, whereby the goal is not about establishing a solution to well defined problem but instead generating insights (wisdom) in a context which allows for emergent causality. This approach results in a plurality of voices rather than one authoritative voice whereby a disjunction of simplification and abstraction gives way to a conjunction with separate parts comprising a rich nuanced picture. In the case of ICPOP, in applying an action research approach, this ‘bricolage’ of perspectives suggests that participants are acting as ‘bricoleurs’ over time, and ‘making the road while walking’.
This points to all integration being theoretic at a policy and strategic level but local in practice and implementation. This does not mean that national signals are not important and it does mean that an enabling environment must be created. However, the complexity of the undertaking requires a process that maintains the umbilical cord between policy, strategy and local implementation. In that regard, the establishment of local governance structures remains fundamental. This provides an executive mandate to address change but also ensures practical, programmatic support. This latter point is critical to ensuring the minutia of implementation is addressed without the tyranny of an overly programmatic burden. This also allows a philosophy of person-centeredness to be embedded in the design and approach to implementation (for example by including service users/carers/ patient champions on the governance group) through the use of patient narrative data and involving patient champions in care pathways mapping.
However, the difficulty of showing benefit and measuring the ‘impact’ of investment is hugely problematic given the complex and interdependent nature of health and social care. The indications are that it may take at least three years to show impact on service use [83-85], implementing at scale [86], addressing professional satisfaction [87], developing care pathways [88] and addressing complexity [101]. These all speak to the multidimensional nature of implementation with key studies [89-92] representing the closest approximation to the work of ICPOP in addressing the critical ingredients associated with implementation.
A reasonable critique of the approach may be that it is weighted towards specialist secondary service integration albeit with a community emphasis rather than integrated, person centred care for individuals. However, it is important to remember that integrated care is a polymorphous concept with a poor track record of spread beyond exemplar sites. In this regard, addressing integrated services, founded on a community facing hub is arguably a necessary stepping stone. This facilitates operational and clinical change and grounds integrated care in a more tangible manifestation, which counters the ‘uniqueness’ of pioneer sites (opportunity, leadership, necessity) as well as undermining the idea that the ideal may not travel well outside of a local context. This arguable reflects the reason for a lack of spread in innovation whereby powerful professional networks will adopt or reject change depending on the prevailing professional norm. This is substantially influenced by their ‘worldview’ and cultural context.
In Ireland (and other jurisdictions), this worldview is dominated by a hospital-centric perspective shaped by public expectation, professional education/induction and organization priorities and perspectives. In response, a cultural accommodation of the change strategy is critically important to ensure the change has sufficient time and opportunity to be adopted as the norm. In that regard, powerful actors must be able to evolve a model that they can relate to and makes sense in their world.
The development of an ambulatory hub is a practical manifestation of this shift away from hospitals towards community oriented (and located) specialist secondary integrated services. To address this the influence of social networks in the process to date, especially between clinical (health and social care) practitioners cannot be underestimated. The bi-annual ICPOP networking events, held in the Royal College of Physicians or prominent government buildings, had a significant influence. This peer-topeer exchange thematically followed the 10-step framework, and allowed each site to explore the operational delivery of abstract and/or new concepts (case management, nursing home outreach, ambulatory hub). In turn, these sessions allowed ICPOP to shape the agenda, get feedback and fine-tune strategic changes to the programme (e.g. measurement) and reflects some of the lessons from implementation of systemic change [93,94]. This latter point is critical in terms of growing a social movement that endorses and supports change in complex adaptive systems. As a result the number of sites grew from six to fourteen (2016-2018) and a further eight sites submitted business cases with the intent of becoming a pioneer site. This represented a three-fold increase in participation over 2 years.
Would this change have happened anyway?
It is worth considering if the change would have happened anyway in the absence of ICPOP. It is certainly true that integrated care is gaining a higher policy profile internationally and in Ireland by virtue of a 10 year strategic transformation plan (Slaintecare). However, the existence of a concept (or indeed a service model) does not automatically translate into implementation. A policy document published in 1988 had proposed district teams with case managers dedicated to ‘the elderly’. This was met with widespread approval but did not get implemented. In fact, despite a review of public health policy/transformation, indicating 27 out of 34 policy documents published since 1990 cites integrated care as a key rationale there have been very few practical examples. Therefore, it cannot be assumed that either government setting out policy, or professional bodies defining best practice will translate into operational reality without attending to implementation.
A more recent acceleration of integrated, community care as the dominant model was prompted by COVID 19. This has resulted in a substantial investment of resources to develop 32 ICPOP teams that gives full population coverage across Ireland. We believe this is the first systemic (national) provision of integrated care for a target population receiving publicly funded services internationally. Whilst circumstantial, the readiness of and professional acceptability of the ICPOP approach and 10 Step Framework had primed the ground for scaling up beyond an initial spread. This readiness reflects the fact that the approach adopted was underpinned by well established, socio-technical theory as well as reflecting contemporary insights from change in complex systems [82]. This recognised complex social systems as a context and that ‘Newtonian’ approaches which introduce change in a stepwise manner is not feasible due to the probabilistic and stochastic rather than deterministic nature of healthcare.
Insights and recommendations
As indicated by Valentijn [53], implementing integrated care is as much an art as a science. Attending to the micro-politics and taking the time to build social capital and trust is key. This is founded on a common vision, based on mutually agreed goals, which in turn becomes the shared currency on which the change process is mobilized.
Attending to national and local governance is critically important. Whilst oversight and accountability are important, good governance serves a more anthropological function organizationally. A national programme governance structure, the National Working Group, Older Persons fulfilled a role as an important focal point for national service redesign by providing a forum for ‘mandating’ of older person initiatives. Similarly local governance provided a scaffold for discussion, visioning, mobilizing and creating a shared sense of purpose. This in turn provided organizational ‘air cover’ for implementation.
The need to describe the older person care pathway in a manner that is flexible enough to accommodate local opportunity, context, and history is an important tangible action. Key activities include mapping the care journey elements across primary/ community, ambulatory and inpatient settings. This captures a common vision to be developed incrementally and can harness good practice already in situ.
An ambulatory hub is a key design feature that provides a service architecture around which integrated services can be further developed. This offers opportunities for emergent or disconnected service offerings to be connected-in. It also has the effect of streamlining care pathways, and in turn generating efficiencies. From a patient and career perspective, it provides a single point of access.
Finance is not a passive enabler. Any new resource must be used considered as an enablement to redesign, mobilizing existing resources more coherently and therefore not simply a compensation for historic underinvestment. It can and should play a dynamic role in mobilizing integrated services/care by explicitly developing a local resource heat-map to show current resources and where new resources can enable these to be redesigned. This avoids a passive dependence on new resources in order to change and reminds everyone that existing resources are often poorly aligned.
The implementation of integrated care needs dedicated national and local programmatic support to succeed. The daily ‘grind’ to develop a new way of working, pathways, structures and processes cannot be an ‘add on’ to the day job of clinical and managerial leaders. Whilst all sites had an ICPOP Service Improvement Lead (SIL), the more successful sites had either a dedicated person (or protected time) devoted to supporting the change. These posts were to provide a key point of contact for ICPOP in addressing the programmatic aspect of implementation. However, programme management is simply a means of delivering a project and the quality of relationships a key determinant of progress that is not easily captured in the metrics.
Within all of this, there is a need to accommodate service users and carers as partners in this process. ICPOP engaged with Age Friendly Ireland as a means of harnessing the inputs of service users and carers as prosumers of services rather than passive recipients
Conclusions
At a macro level, the use of and contents of the 10 Step Framework as both a concept map and to augment implementation reinforces the need for an accompanying agile mixture of emergent, negotiated and planned approaches. This reflects Greenhalghs’ [68] conceptual framework, which recognized that implementing large scale change in health systems is extremely complex and comprises a mix of emergent (adaptive, unplanned) and orderly (planned, managed) dynamics. The underpinning theory of her framework recognizes the importance of complexity as a context, the role of social networks and the tensions with classical management theory. In particular, when a proposed change is to be spread, there is a fine balance to be struck, especially where influence carries more currency than strategic dictat.
The central importance of the 10 Step Framework is as a conceptual anchor. However, the framework needs to be given life with surrounding methodology. In reflecting on the overall process of implementation at an aggregate level, there are now a number of important methodological schematics that came into play to action the 10 Step Framework. These involve both the 10-Step Framework and the 5-stage ICPOP engagement process. Figure 4 provides a dynamic representation of this wider implementation process in action. This represents the ‘arrived’ state of the methodology reported by Harnett [91].
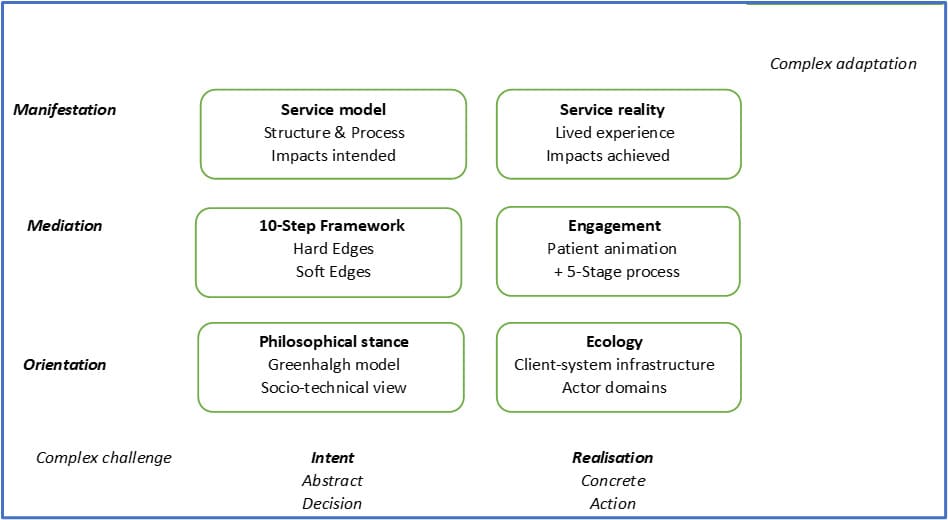
Figure 3: Moving from complex challenge to complex adaption
In order to mobilize change/address a challenge in a complex adaptive environment there are a number of domains to be harnessed in unison to achieve complex adaptation. As a fundamental starting point (orientation), this involves the adapted Greenhalgh model [68] amended to reflect key insights from implementing integrated care (described above). This acts as an underpinning theoretical change principle. This ‘guiding light’ is critical in informing any prospective adopters’ awareness of/ informing their developmental thinking. This draws upon, and highlights the necessary philosophical stance to accommodate the work, thus deliberately blending the balance between emergence and enablement. In tandem with the previous point, there is a need to understand the dynamics of the ecosystem (ecology) in which the change is taking place (e.g. what’s important to whom and how does change happen?).
The 10 Step Framework provides a conceptual shorthand (map), acting as a mediating force in supporting the translation of polymorphous intent into more concrete steps. This mediation is mobilized with key actors through a stepped (5 stage) process of incremental, active support in locus. Key messaging, achieved through animated storytelling such as Nora, (seewww.icpop.org) provides an emotional ‘call to arms’) A Service Model describes the broader landscape and provides a definition of structures (service architecture) and processes (care pathways) to be attended to.
Finally, the manifestation of the change (complex adaptation) is reflected in the new service (structures and processes) and impacts achieved. This combined set of methodologies comprises the full model and represents a combination of orientation (philosophy, theory) moving towards manifestation. The assembly of these domains enables the abstract to be mobilized (intent) towards taking action, resulting in concrete realization of complex adaptation.
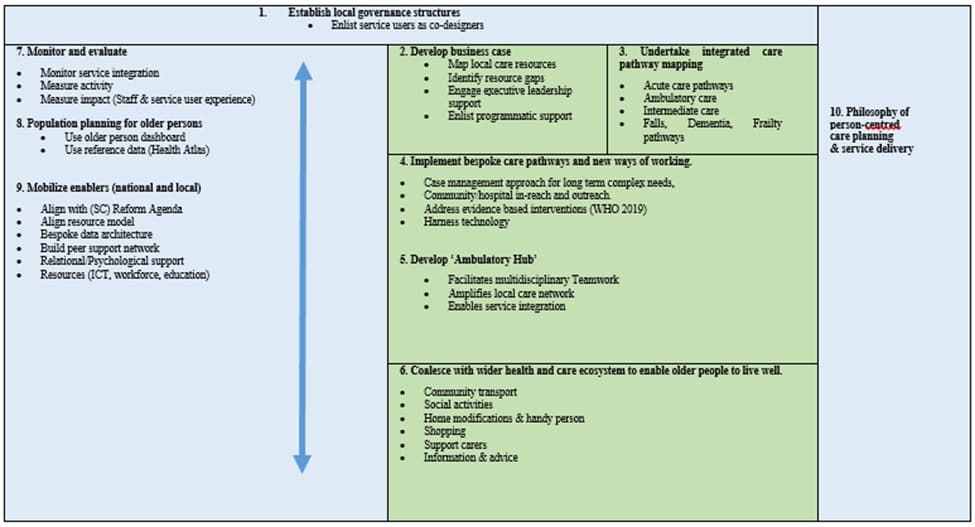
Figure 4: A revised 10-Step Framework for later sites (incorporates refinement of focus and direction).
Declarations
I can confirm that ethical approval and consent to participate was granted for the research undertaken and outlined in this submission. Consent to publish was obtained and data and materials are available on request. There are no competing interests and no funding was provided for this study which was completed as part of a PhD study.
The author’s contribution represent the inputs in the work described as members of the implementation team. The corresponding author would like to acknowledge Dr A Carroll and Michael Fitzgerald for sponsorship and Drs Cathal Heavey and Peter Williams for their support and guidance.
References
- Kodner D, Spreeuwenberg C. (2002) Integrated Care: Meaning, logic, applications and implications, A discussion paper, International Journal of Integrated Care, 2:e12.
- Herbert R, Durand P, Dubuc N, Touringy A. (2003) PRISMA: a new model of integrated service delivery for the frail older people in Canada. International Journal of Integrated Care, 3:e08.
- Nolte E, McKee M. (2008). Caring for People with Chronic Conditions: A Health System Perspective, Maidenhead: Open University Press
- Boult C, Reider L, Leff B, Frick KD, Boyd CM, et al. (2011) “The Effect of Guided Care Teams on the Use of Health Services: Results from a Cluster-Randomized Controlled Trial,” Archives of Internal Medicine, 171:460–66.
- Best A, Greenhalgh T, Lewis S, Saul JE, Carroll S, et al. (2012) ‘LargeSystem Transformation in Health Care: A Realist Review’, Milbank Quarterly, 90:421–456.
- Trivedi D, Goodman C, Gage H, Baron N, Scheibl F, et al. (2013). The effectiveness of inter-professional working for older people living in the community: a systematic review. Health Soc Care Community. 21:113-28.
- Ham C, Walsh N. (2013) Making Integrated Care happen at scale and pace, lessons from experience, Kings Fund London,
- Bodenheimer T, Sinsky C. (2014) From triple to quadruple aim: care of the patient requires care of the provider, Annals of Family Medicine, 12:573-6.
- Pike B, Mongan D. (2014) .The integration of health and social care services, Health Research Board, Ireland.
- Booker C, Turbutt A, Fox R. (2016) Models of care for a changing healthcare system: are there foundational pillars for design? Australian Health Review, 40:136-40.
- Nuffield Trust (2015). Putting Integrated Care into practice, the North West London experience. Nuffield Trust Oct 2015.
- May C, Johnsson M, Finch T (2016) Implementation, context and complexity, Implementation science, BMC, 11:2-12.
- Bodenheimer T (2007). The science of spread: how innovations in care become the norm. California Health Care Foundation.
- Borgermans L, Marchal Y, Busetto L, Kalseth J, Kasteng F, et al. (2017) How to Improve Integrated care for people with chronic conditions: Key findings from EU FP-7 Project INTEGRATE and Beyond. International Journal of Integrated Care, 17 :7.
- Hendry A, Taylor A, Mercer S, Knight P. (2016). Improving outcomes through transformational health and social care integration-The Scottish experience. Healthcare Quarterly, 19:73-79.
- Billings JR, Leichsingring, S Eds (2006) Definitions of integrated care from the stakeholder perspective, in Integrating health and social care services for older people. Evidence from nine European countries, Public Policy and Social Welfare, Ashgate. 51-78.
- Billings J, Mijanovich T, Dixon J. (2006). Case finding algorithms for patients at risk or rehospitalisation: PARR1 and PARR. King’s Fund Health Dialog Analytic Solutions, NYU Centre for Health and Public Service Research
- Keong HC, Mun WL, Feng L, Huang J, Cheah J. (2012) Singapore programme for integrated care for the elderly (SPICE)—an integrated model of care to enable frail elderly to be cared for in the community, International Journal of Integrated Care. 12:e144.
- Carswell, P. (2015) Te Whiringa-Ora: person-centred and integrated care in the Eastern Bay of Plenty, New Zealand, Int J Integr Care. 15: e014.
- Bernabei R, landi F, Gambassi G, Sgadari A, Zuccala G, et al. (1998) Randomised trial of model of integrated care and case management for older people living in the community, British Medical Journal;316:1348-51.
- Counsell, SR. Callahan CM. Clark D (2007) “Geriatric Care Management for Low-income Seniors: A Randomized Controlled Trial,” Journal of the American Medical Association,; 298:2623–33
- Bielaszka-DuVernay C. (2011). The ‘GRACE’ model: in-home assessments lead to better care for dual eligibles. Health Affairs, 30:431-434.
- Boult C, Leff B, Boyd CM, Wolff JL, Marsteller JA, et al. (2013). A matched-pair cluster-randomized trial of guided care for high-risk older patients. J Intl Med 28:612-621.
- Thistlethwaite P (2011). Integrating health and social care in Torbay: improving care for Mrs Smith. King’s Fund, London.
- Berglund H, Blomberg S, Duner A, Kjellgren K (2015). Organising Integrated care for older persons: strategies in Sweden during the past decade, Journal of Health Organisation and Management.29:128-151.
- Naylor C, Alderwick H, Honeyman, M (2015), ‘Acute hospitals and integrated care’, Kings Fund, London.
- Boyd MJ, Koziol-McLain J, Yates K, Kerse N, McLean C, et al. (2008). Emergency Department Case-finding for High-risk Older Adults: The Brief Risk Identification for Geriatric Health Tool (BRIGHT). Academic Emergency Medicine, Jul, 15: 598-606.
- Camero ID, Fairhall N, Langron C, Lockwood K, Monaghan N, et al. (2013) A Multifactorial interdisciplinary intervention reduces frailty in older people : Randomised trial. BMC Med 11:65
- Nolte E (2015). Does integrated care deliver the benefits expected:RAND EU report on integrated care pilot sites in the UK. RAND Europe
- Goodwin N, Smith J. (2011). The evidence base for integrated care, Resource pack, The Kings Fund, (accessed 12.5.16)
- Davies S, Goodman C, Bunn F, Victor C, Dickinson A, et al. (2011). A systematic review of integrated working between care homes and health care services. BMC Health services Research, 11: 320.
- Roland M, Lewis R, Stevenson A, Abel G, Adams J, et al. (2012) Case management for at-risk elderly patients in the English integrated care pilots: observational study of staff and patient experience and second-ary care utilisation, International Journal of Integrated Care. 12:e130.
- Nolte, E (2012) National evaluation of the Department of Health Integrated Care Pilots, Final report, RAND Europe
- Stewart MJ, Georgiou A, Westbrook JI (2013). Successfully integrating aged care services: a review of the evidence and tools emerging from a long-term care program. Int J Integr Care. 13.
- Mitchell GK, Burridge L, Zhang J, Donald M, Scott IA, et al. (2015). Systematic review of integrated models of health care delivered at the primary-secondary interface: how effective is it and what determines effectiveness. J Prim Health. 21:391-408
- ADVANTAGE (2018). European Joint Action on Frailty. Personal correspondence M Andrews, EU JA Meeting, Glasgow 28.2.2018
- Harnett PJ (2018). Improvement attributes in healthcare: implications for integrated care. International journal of health care quality assurance, 31:214-227.
- Jha A, Perlin J, Kizer K, Dudley RA. (2003) Effect of the transformation on the Veterans Affairs Healthcare system on the quality of care, New England Journal of Medicine, 348:2218-27.
- Ovretveit J (2011) ‘Understanding the conditions for improvement: research to discover which context influences affect improvement success’, BMJ Quality and Safety , 20:i18-i2.
- Ovretveit J, Leviton L, Parry GJ (2011). Increasing the generalisability of improvement research with an improvement replication programme. BMJ Quality and Safety. 20:i87-i91.
- Greenhalgh T, Humphrey C, Hughes J, MacFarlane F, Butler C, et al. (2009), ‘How Do You Modernize a Health Service? A Realist Evaluation of Whole-Scale Transformation in London’, Milbank Quarterly, 87: 391–416.
- Macfarlane F, Barton-Sweeney C, Woodard F, Greenhalgh T. (2013) Achieving and sustaining profound institutional change in healthcare: using neo-institutional theory. Social Science and Medicine, 80:10-18.
- Goodwin, N (2015b) Making change happen, a route map for implementation, EU Observatory summer school.
- Busse R, Stahl J. (2014). Integrated care experiences and outcomes in Germany, the Netherlands, and England. Health Affairs, 33:15491558.
- Rutten-van Mölken M. (2017). Common challenges faced in EU-funded projects on integrated care for vulnerable persons. International journal of integrated care, 17:1-4.
- NAO (2017a) Health and Social Care Integration, National Audit Office, Feb 2017.
- Valentijn P, Schepman S, Opheij W, Bruijnzeels M. (2013) Understanding integrated Care; a comprehensive conceptual framework based on the integrative functions in primary care, International Journal of Integrated Care, 13:e010.
- Wren MA, Keegan C, Walsh BM, Bergin A, Eighan J, et al. (2017). Projections of demand for healthcare in Ireland, 2015-2030: First report from the Hippocrates Model. Dublin: Economic and Social ResearchInstitute.
- De Graffenried-Ruffin Jr M (2000), ‘Building a framework to transform health care’, Physician Executive, 26:46-51.
- Clark DM, Silvester K, Knowles S. (2013), ‘Lean management systems: creating a culture of continuous quality improvement’, Journal of Clinical Pathology, 66:638–643.
- Fursule N, Bansod S, Fursule S (2012). ‘Understanding the benefits and limitations of six sigma methodology’. International Journal of Scientific Research and Publication, 2:1-9.
- Feng Q, Manueal CM. (2007). ‘Under the knife; A national survey of six sigma programmes in US Healthcare organizations’, International Journal of Health Care Quality Assurance, 21:535-547.
- Braithwaite J, Churruca K, Long J, Ellis L, Herkes J. (2018) When complexity science meets implementation science: a theoretical and empirical analysis of systems change. BMC Medicine, 16.63.
- Fraser SW, Greenhalgh T. (2001). Coping with complexity. Educating for capability, British Medical Journal, 323:799–803.
- Plsek P and Greenhalgh T (2001). Complexity science: The challenge of complexity in health care. BMJ 323: 625-628.
- Plsek P, Wilson T. (2001) Complexity, leadership, and management in healthcare organisations, BMJ 323: 746–749.
- Wilson T, Holt T, Greenhalgh T (2001). Complexity science, complexity and clinical care, BMJ, 323:658-688.
- Begun JW, Zimmerman B, Dooley K (2003) Health care organizations as complex adaptive systems, In: Mick S, Wyltenbach M (editors), Advances in Health Care Organization Theory. San Francisco, CA: Jossey-Bass; 253–288.
- Greenhalgh T, MacFarlane F, Barton-Sweeney C, Woodard F (2012),If We Build It, Will It Stay?’ A Case Study of the Sustainability of WholeSystem Change in London’, Milbank Quarterly, 90:516–547.
- Greenhalgh T, Robert G, Bate P, Kyriakidou O, Macfarlane F, et al. (2004) ‘How to spread good ideas. A systematic review of the literature on diffusion, dissemination and sustainability of innovations in health service delivery and organisation.’ Report for the NCCSDO, London: NHIR.
- Dixon-Woods M, Bosk CL, Aveling EL, Goeschel CA, Pronovost PJ. (2011), ‘Explaining Michigan: Developing an Ex Post Theory of a Quality Improvement Program’, Milbank Quarterly, 89:167–205.
- Halpern D (2017), Inside the Nudge Unit: How small changes can make a big difference. Penguin Books, London
- MacAdam M. (2008) Frameworks of Integrated care for the elderly: A systematic review, Canadian Policy Research Networks Report, www.cprn.org (accessed 11.10.17)
- Leutz W. (1999) Five laws for integrating medical and social services: lessons from the US and the United Kingdom, Millbank Quarterly, 77:77-110.
- Kodner D. (2009) All together now, a conceptual exploration of integrated care, Healthcare Quarterly, 13:6-15.
- Hollander M, Prince M. (2008) Organising health care delivery systems for persons with ongoing care needs and their families: a best practices framework Healthcare Quarterly, 11:44-54.
- Borgermans L, Devroey D. (2017) A policy guide on integrated care (PGIC): lessons learned from EU projects INTEGRATE and Beyond. International Journal of Integrated Care, 17: 8.
- Wagner H, Austin B, Davis C, Hindmarsh M, Schaefer J, et al. (2001) Improving chronic illness care, Translating evidence into action, Health Affairs, 20:64-78.
- WHO (2010) Framework on Integrated people centred health services.
- Valentijn P. (2016). Rainbow of Chaos: A study into the Theory and Practice of Integrated Primary Care. Int J Integr Care.16:3.
- Minkman M. (2015) Effectively organising integrated care, the developmental model of integrated care, EU Observatory Summer School. Venice, July 2015.
- Seligman M, Csikzentmihalyi M. (2000) Positive Psychology. An introduction. Flow and the foundations of Human Psychology, Springer, Dordrecht.
- Cooperrider D, Srivastava S. (1987) Appreciative Inquiry in Organisational Life. In W Pasmore& R Woodsman (Eds), Research in Organisational Change and Development 1:129-169.
- Wallston BS, Wallston KA. (1978) Locus of control and health; A review of the literature, Health Education Monographs, 6:107-117.
- Bandura A. (1977) Self-efficacy: toward a unifying theory of behavioral change, Psychological Review, 84: 191-215.
- De Shazer S, Kim-Kerg I. (1997) What works? Remarks on research aspects of solution focused therapy. Journal of family Therapy Blackwell Publishers. 19:121-124.
- Trist E, Bamforth KW. (1951). Some social and psychological consequences of the longwall method of coal getting: an examination of the psychological situation and defences of a work group in relation to the social structure and technological content of the work system. Human Relations, 4:3-38.
- Dixon-Woods M, Baker R, Charles K, Dawson JF, Jerzembek G, et al. (2014), ‘Culture and behaviour in the English National Health Service: overview of lessons from a large multi-method study’, BMJ Quality and Safety. 23:106–115.
- Sadler E, Sandall J, Sevdalis N, Wilson D. (2019). The contribution of implementation science to improving the design and evaluation of integrated care programmes for older people with frailty. Journal of Integrated Care, 27: 232–240.
- Harnett PJ. (2020) The development, application and evaluation of a framework as a change methodology in implementing integrated care for older persons; From rhetoric to reality to reality through action research. PhD Thesis. University of Limerick.
- Miller R. (2016). Crossing the cultural and value divide between health and social care. International journal of integrated care, 16:10.
- Miller R, Stein KV. (2020). The Odyssey of Integration: Is Management its Achilles’ Heel? International Journal of Integrated Care, 20: 7, 1–14.
- Hoogendijk EO. (2016) How effective is integrated care for community-dwelling frail older people? The case of the Netherlands. Age Ageing.45:585-8.
- Nolte E (2018). How do we ensure that innovation in health service delivery and organization is implemented, sustained and spread? Policy Brief. Copenhagen: WHO Regional Office for Europe
- Janse B, Huijsman R, de Kuyper RDM, Fabbricotti IN. (2016) Delivering Integrated Care to the Frail Elderly: The Impact on Professionals’ Objective Burden and Job Satisfaction. Age Ageing. 45:585-8.
- Ní Shé É, McCarthy M, O’Donnell D, Collins O, Hughes G, et al (2018) The systematic approach to improving care for Frail Older Patients (SAFE) study: A protocol for co-designing a frail older person’s pathway. HRB Open Res.1:9.
- Inzitari M, Pérez LM, Enfedaque MB, Soto L, Díaz F, et al. (2018) Integrated primary and geriatric care for frail older adults in the community: Implementation of a complex intervention into real life. Eur J Intern Med. 56:57-63.
- Asthana S, Gradinger F, Elston J, Martin S, Byng R. (2020). Capturing the Role of Context in Complex System Change: An Application of the Canadian Context and Capabilities for Integrating Care (CCIC) Framework to an Integrated Care Organisation in the UK. International Journal of Integrated Care. 20:4
- Leijten FRM, Struckmann V, van Ginneken E, Czypionka T, Kraus M, et al. (2018) The SELFIE framework for integrated care for multi-morbidity: Development and description. Health Policy, 122: 12–22.
- SUSTAIN (2019). SUSTAIN Roadmap. Proceedings of final conference 2019,
- Casebourne, J (2014) ‘Why motivation matters in public sector innovation.’ London.
- Massoud R, Barry D, Murphy A, Albrecht Y, Sax S, et al. (2016) How do we learn about improving healthcare, the call for a new epistemological paradigm. International Journal for Quality in Healthcare, 28:420–424.
- Robins, J (1988) The Years Ahead: A Policy for the Elderly: report of the Working Group Chaired by Joseph Robins. Dublin: Stationary Office.
- Barry S, Dalton R, Eustace-Cook J. (2019). Understanding change in complex health systems: A review of the literature in change management in health and social care systems (2007-2017). Dublin: HSE.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.