WhatsApp Usage during COVID-19 in Sudan for Diagnosis, Management and Follow-up of Severe Tinea Infection of Upper and Lower Extremities: Clinical Case: Severe Bilateral Tinea Pedis, Followed by Severe Bilateral Tinea Manuum
by Musa Basheer Mansour MBBS, MD, MSc, PPCR, Dip1*, Sara Elsheikh Ahmedana MBBS, MD, MSc, Dip2, Amr Musa Basheer3
1Primary Health Care Corporation, Umm Ghuwailina Health Center, Doha, P.O. Box 26555, Qatar
2Primary Health Care Corporation, Abu Baker Al-Siddiq Health Center, Doha, Qatar
3Medical Student at The Royal College of Surgeons in Ireland, Medical University of Bahrain, P.O. Box 15503, Adliya, Bahrain
Musa Basheer Mansour ORCID: https://orcid.org/0000-0002-5278-2601
Sara Ahmedana ORCID: https://orcid.org/0009-0006-8084-2719
Amr Musa Basheer ORCID: https://orcid.org/0009-0006-9734-5997
*Corresponding authors: Musa Basheer Mansour, MBBS, MD, MSc, PPCR, Dip, Primary Health Care Corporation, Umm Ghuwailina Health Center- Doha-Qatar. Mobile: +97430188872. P.O. Box 26555. Email: musabasheer97@yahoo.com mbasheer@phcc.gov.qa
Received Date: 28 April, 2024
Accepted Date: 03 May, 2024
Published Date: 06 May, 2024
Citation: Mansour MB, Ahmedana SE, Basheer AM (2024) WhatsApp Usage during COVID-19 in Sudan for Diagnosis, Management and Follow-up of Severe Tinea Infection of Upper and Lower Extremities: Clinical Case: Severe Bilateral Tinea Pedis, Followed by Severe Bilateral Tinea Manuum. J Family Med Prim Care Open Acc 8: 256. https://doi.org/10.29011/2688-7460.100256
Abstract
Our case details a 48-year-old female, asthmatic, not pregnant or lactating or at risk presenting with itching and erythema on both feet. Initially treated as a severe contact dermatitis with dermatologist for nine months in three visits without improvement. Six months later from the first visit, the patient observed that the problem involved both hands. Subsequent follow up and treatment regimens were failed, and the patient referred to internal medicine and oncology units. WhatsApp communication and follow up during COVID-19 was continued for three months with patient. Laboratory investigations potassium hydroxide [KOH] test, visualized scraping skin under microscopy confirmed the diagnosis of severe tinea pedis and tinea manuum. Liver and renal function tests, screening for diabetes and complete blood picture were normal. Terbinafine tablets 250 mg, Fucidin ointment for the inflamed red skin, desloratadine 5 mg, an emollient cream was administered. Despite prior misdiagnosis and treatment as contact dermatitis, our case demonstrates severe tinea pedis and tinea manuum with laboratory confirmation. Significant improvement includes well healed skin and no pruritis was achieved after 8 weeks course of oral terbinafine. Although tinea pedis and manuum diagnose clinically and sometimes cures without treatment but our case underscores the importance of accurate diagnosis in distinguishing severe tinea pedis and tinea manuum from conditions such as contact dermatitis, psoriasis, and pompholyx.
Keywords: Tinea pedis; Tinea manuum; Terbinafine; Contact dermatitis; Potassium hydroxide
Background
Tinea pedis or Athlete’s foot is the fungal infection of the foot and Tinea manuum is the fungal of hand [1]. Athlete’s foot reported in 1908 [2]. Worldwide, the dermatophyte infection prevalence about 10% to 25%. Tinea infection of feet and hands are the most common and athlete’s foot prevalence around 70% in adult population [1]. The lifetime risk is up to 70% with a peak age of incidence is between 16 and 45 years, and prevalence of tinea pedis is approximately 3% [3]. Around 0.3%-13%, represents the prevalence of Tinea manuum depending on geographic distribution [1] Dermatophytes are the main etiological organism of tinea infection and Trichophyton rubrum, T. mentagrophytes are the main cause of tinea pedis and less commonly due to Epidermophyton floccosum [3-5]. Like tinea pedis T. rubrum is the main cause of hand fungal infection of the hand then T. mentagrophytes, Epidermophyton floccosum, T. verrucosum, T. interdigitale, Microsporum canis. Microsporum gypseum, Trichophyton eriotrephon, and Arhroderma benhamiae are rarely causative agent. [1]. The infection is very contiguous and transmits by direct contact with infected skin, animals, contaminated soil, towels, and swimming pools [1,4, 5]. The predisposing factors include immunocompromised states, chronic diseases like diabetes and chronic kidney disease, as well as conditions fostering humidity, sweating, prolonged use of occlusive footwear, recurrent physical or chemical trauma of the hands and feet. Also seen in farmworkers and pet owners [1,3-5]. The symptoms typically begin with itching and erythema, cracking, dryness, increased skin markings, progressing to white lesions with creases, blister, and elevation of the lesions in chronic cases [1,3-5]. Confirmation of the diagnosis involves culture or a potassium hydroxide (KOH) test on the scraped infected skin, performed with direct microscopy [1,3,5]. Differential diagnoses for manuum encompass psoriasis, contact dermatitis, dyshidrotic eczema, and hand eczema [1], and for pedis may include pitted keratolysis, erythrasma, eczema, or psoriasis, bullous impetigo, bullous allergic contact dermatitis, thermal injury, oedema-related bullae, or localized bullous pemphigoid [3, 5, 6]. Interdigital lesions may appear like psoriasis, erythrasma or candida infections while Vesiculobullous lesions may resemble pustular psoriasis, dyshidrosis, acute contact dermatitis or scabies [6].
Preventive measures involve hand washing, maintaining hygiene, avoiding touching infected areas and foot scratching to prevent transmission [1,3-5]. Antifungals cream, gel, or spray are the first line of therapy for the simple uncomplicated cases. Naftifine, Terbinafine, Itraconazole, Ketoconazole, Fluconazole or Clotrimazole for 4 to 6 weeks are effective while Luliconazole or Econazole are very effective for short duration 2 to 4 weeks, [1, 3, 5]. In severe or chronic and non-responsive cases, systemic terbinafine at 250 mg daily for 4-6 weeks or Griseofulvin or Itraconazole are effective and required monitoring of liver and kidney function tests during treatment [1,3,4]. The use of corticosteroids remains controversial; however, they may provide relief in severely inflamed cases by reducing pruritus or burning sensations [1]. The complications depend on the progression of disease and occurrence of crack which lead to bacterial infection of skin, cellulitis, pyoderma, lymphangitis, nail infection, and osteomyelitis are seen more frequently in individuals with chronic diseases and immunosuppression [1,5].
Objectives
- To delineate a complex case of tinea pedis that extended to hands, initially misdiagnosed, and treated for nine months as contact dermatitis without investigations, underscores the diagnostic challenges associated with this atypical presentation and the lack of improvement for therapy.
- To document a unique and severe instance of tinea pedis and manuum in an asthmatic patient residing in a plant and waterrich region near the White Nile in Gezira state in Sudan.
Methods
We employed WhatsApp as a communication tool for data collection, treatment, and patient follow-up during COVID-19 pandemics.
Case Report
Our patient was a 49-year-old woman asthmatic initially experienced intense pruritis and redness in her feet. During her first visit, a dermatologist diagnosed her condition as severe contact dermatitis based on her bronchial asthma history. Her therapy included daily levocetirizine 5mg, fluticasone 0.05% cream twice a day, and emollient three times a day for three months.
At second visit three months later, she presented with the same complaint, and examination of her feet revealed creases, erythema, and small cracks. The physician advised her to continue the same medications for an additional three months without conducting further investigations.
During her third visit three months later, she sought medical attention for severe itching and redness in her hands, accompanied by skin changes, including cracking, scaling, and blistering (Figure 1). She was diagnosed again with severe chronic contact dermatitis of the feet and pompholyx in both hands (Figure 2). Again, her treatment included oral prednisolone (10 mg) for 7 days, salicylic acid 5% in mometasone 0.1% ointment twice a day, Vaseline cream three times a day, and desloratadine tablets (5 mg) daily for another 3 months.

Figure 1: Right and left foot before treatment.

Figure 2: Left before and after treatment.
However, after three months, there was no improvement in her condition, prompting her physician to refer her to an internal medicine specialist and an oncologist for a second opinion and further management. Throughout this period, she relied on desloratadine 5 mg daily and Vaseline for more than 3 months to alleviate itching, address skin dryness, and manage the skin lesions. She communicated with her medical team via WhatsApp, providing comprehensive medical information, including the history of her condition, prescribed medications, follow-up details, disease progression, and photos of both hands and feet from different an
After visualizing fungal infection through scraping and microscopy with KOH, positive results were obtained. Baseline investigations, including Liver Function Tests [LFT], Complete Blood Count [CBC], renal function tests [RFT], and Haemoglobin A1c (HbA1c), were normal. Treatment involved Terbinafine 250mg daily and emollient ointment three times a day for 8 weeks, Fucidin ointment for 14 days, and desloratadine daily 5 mg for one month. One month later, pruritis reduced, and lesions nearly disappeared (Figure 3). Follow-up included repeating LFT and RFT and continuing emollient ointment for an additional 4 weeks.

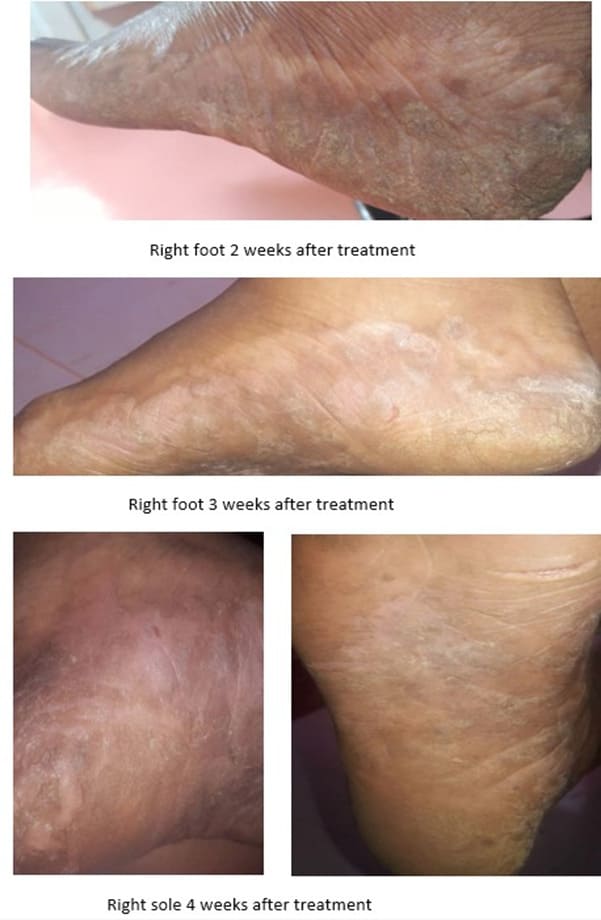
Figure 3: Right and left foot after treatment.
Finally, the patient’s hands and feet appeared nearly normal, and baseline investigations were within the normal range.
Discussion
WhatsApp is a private messaging across the world that use in more than 180 countries by more than 2 billion people with no subscription fees. The clinical diagnosis of early tinea infection relies on patient history such as residence, occupation, risk factors, and chronic diseases, analysis of the patient’s complaints i.e. itching, scaling, scratching and redness. Additionally, systematic and local physical examination is conducted to identify characteristic signs on the skin, supplemented by laboratory investigations [1,3-5]. Despite prolonged therapy, the diagnosis in our case remains uncertain. At this stage, tests such as the KOH test, direct visualization of hyphae under microscopy, or the culture of scraped infected skin can be utilized for confirmation and to exclude medical conditions that resemble severe athlete’s foot [1,3-5]. Moreover, the lesion on both feet has significantly increased, and both hands are involved, showing creases, scaling, and multiple severe cracks [3].
Tinea pedis presents in four categories: chronic interdigital (between the toes), plantar or sole (chronic scaly or “moccasin foot”), acute ulcerative (macerated lesions with scaly borders), and vesiculobullous (blisters) [3-5]. This presentation is typically observed in our case. The treatment of early cases of tinea pedis and manuum includes topical antifungals such as terbinafine, naftifine, itraconazole, ketoconazole, fluconazole, or clotrimazole for 4-6 weeks, and luliconazole and econazole for 2-4 weeks [1,3, 5]. However, these were not employed in our case despite the failure of long-term use of contact dermatitis medications. Plantartype athlete’s foot proved more resistant to topical treatments due to the presence of thickened hyperkeratotic skin on the sole, leading to the employment of terbinafine oral tablets as the drug of choice [3,5]. The preventive measures and education such as hygiene, avoid scratching and touching infected surfaces, separate infected toes with nail clipper, keeping nails short and skin dry, wearing big enough shoes and avoiding walking without shows, and changing socks daily will reduce tinea infections [1, 3-5]. A study compiling cases of tinea manuum revealed that the “two feet, one hand syndrome” accounting for 65% of cases, bilateral tinea pedis with bilateral tinea manuum (19.3%), unilateral tinea manuum (11.8%), and bilateral tinea manuum (3.9%) [1].
Our patient was initially diagnosed with severe contact dermatitis and showed no response to therapy over three subsequent visits spanning 12 months. This case is exceptionally rare and unique highlights the challenges in diagnosing and managing severe bilateral tinea pedis affecting the entire feet followed by severe bilateral manuum involving both hands, which can often be misdiagnosed and consequently mismanaged.
Therefore, early treatment is crucial to prevent the spread of the infection from the feet to the hands.
Funding
This research was conducted without funding.
Availability of Data and Materials
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Declarations
Ethics Approval and Consent to Participate: Not applicable.
Consent for Publication: Not applicable.
Competing Interests: The authors declare that they have no competing interests.
References
- Chamorro MJ, House SA (2023) Tinea Manuum. In: StatPearls. StatPearls Publishing.
- Homei A, Worboys M (2013) Fungal disease in Britain and the United States 1850-2000: mycoses and modernity. Springer. p. 44.
- Leung AK, Barankin B, Lam JM, Leong KF, Hon KL (2023) Tinea pedis: an updated review. Drugs Context 12: 2023-5-1.
- Veraldi S, Esposito L, Gorani A (2018) Tinea pedis acquired in mosques? Mycoses 61: 794-795.
- Nigam PK, Syed HA, Saleh D (2023) Tinea Pedis. In: StatPearls. StatPearls Publishing.
- Xie F, Lehman JS (2022) Bullous Tinea Pedis. Mayo Clin Proc 97: 1396-1397.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.