Validation of the Coronal Plane Alignment of the Knee Classification for Short-Leg Anteroposterior Weight-Bearing Radiograph with Use of Anatomic Axis Measurements
by Thomas L Bradbury, Anita “Alex” Bradham, Natalie L Gresham, Charlotte C Baker*, Zachary M Ricciardelli, Joseph M Schwab
Total Joint Specialists, Advanced Center for Joint Surgery and Northside Hospital Forsyth, USA
*Corresponding author: Charlotte C Baker, Total Joint Specialists, LLC, Northside Hospital Forsyth, 2000 Howard Farm Drive, Cumming, GA, USA
Received Date: October 21, 2025
Accepted Date: November 03, 2025
Published Date: November 08, 2025
Citation: Bradbury TL, Bradham AA, Greshan NL, Baker CC, Ricciardelli ZM, et al. (2025) Validation of the Coronal Plane Alignment of the Knee Classification for Short-Leg Anteroposterior WeightBearing Radiograph with Use of Anatomic Axis Measurements. J Orthop Res Ther 10: 1407. https://doi.org/10.29011/2575-8241.001407
Abstract
Preoperative assessment of coronal knee alignment is essential for total knee arthroplasty (TKA) planning. Long-leg radiographs (LLRs) are the gold standard for evaluating mechanical axes but are time-intensive, costly, and involve more radiation. Short-leg radiographs (SLRs) are more common but may be less accurate. The Coronal Plane Alignment of the Knee (CPAK) classification, based on joint line obliquity (JLO) and arithmetic hip-knee-ankle angle (aHKA), standardizes coronal alignment description. This study assessed whether a 5° correction to the short-leg lateral distal femoral angle (slLDFA) on SLRs can approximate CPAK classification from LLRs. We retrospectively reviewed 268 patients who underwent staged bilateral TKA by a single surgeon using a mechanical alignment technique. All had preoperative SLRs and LLRs. Two independent raters measured LDFA and MPTA to calculate aHKA and JLO, then assigned CPAK types using the MacDessi algorithm. Reliability was assessed with intraclass correlation coefficients (ICCs). Agreement between LLR- and corrected-SLR-derived CPAK classifications was evaluated per Kraus et al, 2025. We found a systematic difference of 6.3° between long-leg and short-leg LDFA measurements. Applying a 5° correction to the slLDFA produced identical CPAK classifications to those from LLRs in 66% (177/268) of cases. Angle measurement ICCs ranged from 0.780 to 0.965. Applying a 5° slLDFA correction to SLRs offers a valid, reliable, and cost-effective approximation of CPAK classification when LLRs are unavailable, supporting efficient preoperative planning while reducing patient burden.
Keywords: Knee alignment; CPAK; Short-leg radiographs; Measurement reliability; Lateral distal femoral angle
Introduction
Accurate visualization of knee alignment, particularly in the coronal plane, is crucial for preoperative planning for total knee arthroplasty (TKA). Preoperative weight-bearing anteroposterior (AP) and lateral radiographs of the knee with a field of view from mid-femur to mid-tibia, so-called “short-leg” radiographs (SLRs), are commonly used for preoperative planning. However, full-length (long-leg) AP weight-bearing radiographs (LLRs) have been deemed the gold standard for visualizing many of the radiographic measurements of knee alignment [1,2]. The Coronal Plane Alignment of the Knee (CPAK) system uses joint line obliquity (JLO) and arithmetic hip-knee-ankle angle (aHKA) to determine coronal knee alignment, which has been validated on LLRs [3].
While seemingly more accurate, the use of LLRs as opposed to SLRs involves significantly increased radiation exposure, carries additional costs, and requires more time to capture a clear image [2,4,5]. However, SLRs do not contain all of the anatomic landmarks to exactly reproduce the angles that comprise the CPAK classification. While previous studies have concluded that standard (short-leg) AP radiographs inaccurately assess several factors of lower limb alignment and cannot adequately replace LLRs [2,6], some authors have advocated for their use anyway, including a “correction factor” based on differences in anatomic tibiofemoral angle and mechanical tibiofemoral angle [5,7-12]. This technique, however, has not been previously validated. Kraus et al employed SLRs with a correction factor of 5° added to the anatomical LDFA to determine CPAK classification in a recent publication investigating the relationship between CPAK retention and patient-reported outcome measures [7].
We therefore asked the following questions: 1) How does interrater and intrarater agreement compare between LDFA and MPTA measurements on short-leg and long-leg radiographs? 2) Is there a systematic difference for LDFA when measured on short-leg radiographs versus long-leg radiographs? 3) What LDFA correction for short-leg radiographs provides the optimal CPAK agreement?
Materials and methods
Study Design
This study included a retrospective radiographic review of 271 patients who underwent staged bilateral TKA with mechanical alignment approach at an ambulatory surgery center by a single orthopedic surgeon. Patients were included if they had both SLRs and LLRs from before and after surgery. Patients were excluded if they had a fracture malunion, fracture fixation, osteotomy, or other surgery altering bony alignment. Patients who underwent additional surgery (other than a TKA) on the operative leg in the time between preoperative and postoperative imaging were also excluded (n=3).
Radiographic Assessment and Calculations
Preoperative SLRs and LLRs were utilized for measurement. Two independent raters reviewed all patients’ short- and long-leg AP weight-bearing radiographs to assess knee alignment. Long-leg radiographic measurements included the lateral distal femoral angle (LDFA) and the medial proximal tibial angle (MPTA). From these, the arithmetic hip-knee-ankle angle (aHKA) was calculated as MPTA minus LDFA, and the joint line obliquity (JLO) was calculated as the sum of LDFA and MPTA. For short-leg radiographs, measurements included the short-leg LDFA (slLDFA) and short-leg MPTA (slMPTA). Corresponding calculations included the short-leg arithmetic HKA (slaHKA), defined as slMPTA minus slLDFA, and the short-leg JLO (slJLO), defined as the sum of slLDFA and slMPTA. Long-leg radiographic measurements were obtained following the methodology described by Graden et al and others [2,13-15]. For SLRs, in cases where the hip and ankle were not visualized, lines were drawn through the center of the femoral and tibial diaphysis (Figure 1).
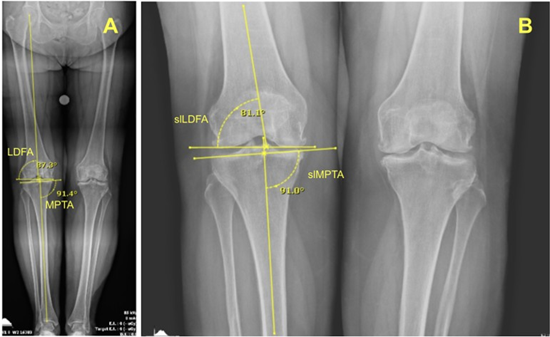
Figure 1: Long-leg (A) and short-leg (B) radiographs of a knee showing the lateral distal femoral angle (LDFA) and the medial proximal tibial angle (MPTA) measurements to determine Coronal Plane Alignment of the Knee (CPAK) classifications.
Measurements were completed in a blinded manner using OpalRad software (Version 2.4.4.7), which ensures accurate magnification calibration via a standard 25.4 mm orthosphere. After completing all analyses and re-measuring 50 cases, inter- and intra-rater reliability were calculated. CPAK classifications were determined with the algorithms described by MacDessi et al. [3,16].
Data Analysis
For all alignment angles (LDFA, MPTA, aHKA, JLO), we first assessed intra- and inter‐rater reliability using the intraclass correlation coefficient (ICC) and Kappa Statistics [17]. To compare short-leg and long-leg measurements, we conducted paired t-tests and calculated Pearson correlation coefficients with simple linear regression. Differences exceeding the minimal clinically important difference (MCID) of 2°, as defined by Graden et al, were considered both statistically and clinically significant [2]. Agreement in CPAK classification was quantified in three ways: JLO agreement, aHKA agreement, and exact CPAK agreement, summarized in contingency tables. Finally, to identify the optimal LDFA correction for SLRs, we plotted JLO agreement, aHKA agreement, and CPAK agreement versus LDFA corrections from 2° to 10° by .001° increments. The maximum composite agreement (defined by the average of the JLO and aHKA agreements) was identified, and the range of LDFA correction values that demonstrated a composite agreement within 0.2% of the maximum composite agreement was marked. Statistical analyses were performed using R version 4.4.2 (Vienna, Austria).
Results
Patient characteristics
A total of 268 preoperative SLRs and LLRs, each from a unique patient, were examined. The patients’ mean ± SD (range) age was 70.51 ± 7.53 (42-91). Of 268, male patients made up 102 (38%) of the limbs, the rest were female (166 (62%)). Laterality was recorded with right knees comprising 143 (53%) and left knees comprising 125 (47%) of the 268 radiographs. In the sample of 268 knees, preoperatively, 42.5% of knees were classified as CPAK I, 22.4% CPAK II, and 18.7% CPAK III, aligning with common phenotypes of an arthritic population [3].
Interrater and Intrarater Agreement
The intra-observer reproducibility (ICCs) ranged from 0.82 to 0.97 for long-leg and 0.78 to 0.96 for short-leg measurements. The inter-observer reliability (ICCs) ranged from 0.90 to 0.91 for longleg and 0.79 to 0.91 for short-leg measurements (Table 1).
|
Inter Rater Correlation Coeff |
Intra Rater 1 Correlation Coeff |
Intra Rater 2 Correlation Coeff |
|
|
Long-Leg LDFA |
0.90 |
0.95 |
0.97 |
|
Long-Leg MPTA |
0.91 |
0.87 |
0.82 |
|
Short-Leg LDFA |
0.79 |
0.78 |
0.81 |
|
Short-Leg MPTA |
0.91 |
0.96 |
0.94 |
|
Tibial angle (MPTA) and femoral angle (LDFA) measurements on long-leg and short-leg radiographs. |
|||
Table 1: Inter- and intra-rater correlation coefficients for lateral distal femoral angle (LDFA) and medial proximal tibial angle (MPTA).
Systematic Differences in LDFA Measurements between SLR and LLR
The measured LDFA was assessed for the entire cohort and within each CPAK classification (Table 2). On SLRs, the mean (range) LDFA was 81.4° (73.3-97.9°). On corresponding LLRs, the mean LDFA was 87.7° (78.1-96.3°). The average difference between long-leg and short-leg LDFA measurements was 6.3°(2.9-9.3°).
|
Characteristic |
Overall N = 2681 |
I N = 1141 |
II N = 601 |
III N = 501 |
IV N = 171 |
V N = 71 |
VI N = 191 |
VII N = 11 |
|
Short-Leg LDFA |
81.4 (73.2-97.9) |
82.6 (78.3-88.7) |
80.8 (75.9-87.0) |
79.0 (73.3-82.5) |
84.3 (80.2-97.9) |
81.1 (78.8-83.1) |
80.3 (77.9-83.7) |
86.2 (86.2-86.2) |
|
Long-Leg LDFA |
87.7 (78.1-96.3) |
89.5 (85.5-94.3) |
86.4 (80.1-88.9) |
83.9 (78.1-86.8) |
92.6 (90.0-96.3) |
89.2 (88.0-90.2) |
86.4 (82.5-88.4) |
95.4 (95.4-95.4) |
|
Delta LDFA |
6.3 (2.9-9.3) |
6.2 (2.9-9.3) |
6.6 (3.9-9.0) |
6.8 (4.6- 9.0) |
5.9 (3.9-8.7) |
5.0 (3.8- 7.9) |
6.2 (4.4-8.0) |
7.5 (7.5-7.5) |
|
SL LDFA, short-leg lateral distal femoral angle; LL LDFA, long-leg lateral distal femoral angle. 1Mean (Min - Max). |
||||||||
Table 2: Descriptive Statistics of short-leg and long-leg LDFA measurements by corresponding CPAK classification, and the difference (delta) between them.
Optimal LDFA correction factor for SLRs
To identify the slLDFA correction that maximizes agreement between SL and LL CPAK phenotypes, we plotted JLO agreement, aHKA agreement, and CPAK agreement versus slLDFA corrections from 2° to 10° (Figure 2). The optimal correction threshold fell between 4.8° and 5.1°, yielding ≥66% agreement. Applying the 5° slLDFA correction to the SLRs and then comparing the predicted CPAK classifications against the gold standard LLR classifications (Table 3) yielded a JLO agreement of 237/268 (88%), while aHKA agreement was 201/268 (75%).
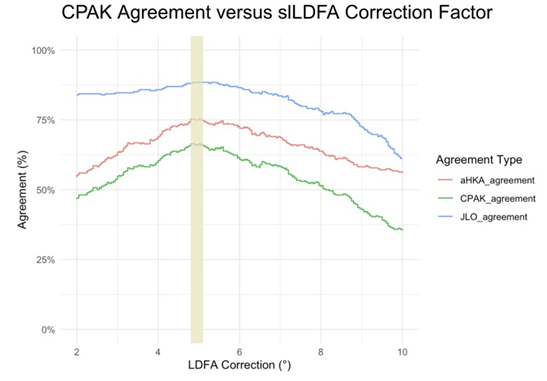
Figure 2: Agreement between short-leg and long-leg radiographic classifications across a range of slLDFA correction factors. JLO, aHKA, and CPAK agreements are plotted as functions of slLDFA correction from 2° to 10°. The shaded region denotes the range of maximal composite agreement. Abbreviations: JLO, joint line obliquity; aHKA, arithmetic hip-knee-ankle angle; CPAK, coronal plane alignment of the knee; slLDFA, short-leg lateral distal femoral angle.
|
Characteristic |
Overall N=2681 |
I n=1141 |
II n=601 |
III n=501 |
IV n=171 |
V n=71 |
VI n=191 |
VII n=11 |
|
SL CPAK |
||||||||
|
I |
105 (39%) |
87 (76%) |
10 (17%) |
0 (0%) |
8 (47%) |
0 (0%) |
0 (0%) |
0 (0%) |
|
II |
89 (33%) |
26 (23%) |
43 (72%) |
14 (28%) |
2 (12%) |
5 (57%) |
0 (0%) |
0 (0%) |
|
III |
53 (20%) |
0 (0%) |
6 (10%) |
35 (70%) |
2 (12%) |
2 (29%) |
8 (42%) |
0 (0%) |
|
IV |
4 (1.5%) |
1 (0.9%) |
1 (1.7%) |
0 (0%) |
1 (5.9%) |
0 (0%) |
0 (0%) |
1 (100% |
|
V |
5 (1.9%) |
0 (0%) |
0 (0%) |
0 (0%) |
3 (18%) |
1 (14%) |
1 (5.3%) |
0 (0%) |
|
VI |
11 (4.1%) |
0 (0%) |
0 (0%) |
1 (2%) |
0 (0%) |
0 (0%) |
10 (53%) |
0 (0%) |
|
VII |
1 (0.4%) |
0 (0%) |
0 (0%) |
0 (0%) |
1 (5.9%) |
0 (0%) |
0 (0%) |
0 (0%) |
|
JLO |
237 (88%) |
113 (99%) |
59 (98%) |
49 (98%) |
4 (24%) |
1 (14%) |
11 (58%) |
0 (0%) |
|
aHKA |
201 (75%) |
88 (77%) |
43 (72%) |
36 (72%) |
10 (59%) |
5 (71%) |
18 (95%) |
1 (100%) |
|
CPAK |
177 (66%) |
87 (76%) |
4v3 (72%) |
35 (70%) |
1 (5.9%) |
1 (14%) |
10 (53%) |
0 (0%) |
|
SL: short-leg; LL: long-leg; CPAK, Coronal Plane Alignment of the Knee; sLLDFA, short-leg lateral distal femoral angle; JLO, joint line obliquity; aHKA, arithmetic hip-knee-ankle angle 1n(%) |
||||||||
Table 3: Agreement between Short-Leg and Long-Leg CPAK classifications after applying a 5° slLDFA correction.
Synthesis
Surgeons use LLRs preoperatively to determine CPAK classification, which guides alignment strategy and surgical approach. LLRs are considered the gold standard for CPAK classification, but are more costly, require greater patient mobility, and expose patients to higher levels of radiation [2,3,5]. Some authors suggest that applying a 5° correction to the slLDFA allows accurate CPAK classification using only an SLR [5,7-12]. No prior studies, however, have validated the accuracy of using SLRs for CPAK classification.
This study, which compared CPAK classification based on LLRs and SLRs, revealed the following findings: 1) SL and LL radiographic measurements demonstrated good to excellent inter- and intrarater reliability across all parameters; 2) there is a systematic bias of 6.3° difference between the anatomic and mechanical LDFA; 3) yet the use of a 5° correction factor applied to short-leg LDFA measurements best reconciles the CPAK classification derived from LLRs with an accuracy of 66%.
Limitations
This study has limitations. All angular measurements are subject to a ±2° margin of error and variability in image acquisition [18-20]. Factors such as rotational malpositioning, fixed flexion contractures, and bone loss associated with advanced osteoarthritis may have contributed to measurement error and could not be excluded. Because this alignment type was not represented, there is insufficient data to validate the methodology across all CPAK classifications. Variability is present in the degree of osteoarthritis, which may influence radiographic measurements. There was also variability in the amount of distal femur and proximal tibia able to be visualized on SLRs. Our study population lacked patients in CPAK categories VII, VIII, and IX. Although rare, our findings are not applicable to these phenotypes [3]. The lack of these phenotypes likely contributed to the high JLO agreement rate of 88%. Patients with these less common phenotypes may be more likely to receive additional imaging beyond short-leg radiographs. Therefore, we caution against generalizing the 5° correction factor to these categories, as we were unable to validate its use in this subset of patients.
Analysis
Our results show good to excellent inter- and intra-rater reliability on short-leg radiographic measurements. While both inter- and intra-rater reliability and reproducibility have been reported for LDFA and MPTA measurements on LLRs, only inter-rater reliability has been studied for these measurements on SLRs. Park et al reported inter-observer reliability of 0.90 for long-leg MPTA, 0.91 for long-leg LDFA, 0.89 for short-leg MPTA, and 0.91 for short-leg LDFA; however, no intra-rater reproducibility was performed [21]. In comparison, our study found similarly high inter-observer reliability for long-leg measurements (≥0.896) and slightly lower values for short-leg measurements (≥0.792). The increased variability observed in short-leg measurements may be attributed to the limited availability of anatomical landmarks for accurate referencing. Bouché et al demonstrated an intra-observer reproducibility good to excellent for long-leg LDFA (ICC = 0.85 and 0.92) and moderate to good for MPTA (ICC = 0.72 and 0.75). Inter-observer reliability was excellent for LDFA (ICC = 0.91) and good for MPTA (ICC = 0.80) [22]. Our findings are consistent with these prior studies and further support the reproducibility of alignment measurements, particularly when using SLRs in the context of CPAK classification.
When comparing the short- and long-leg LDFA, there was a systematic bias that averaged to a difference of 6.3°. Chang et al found that in elderly knees (mean age of 70 ± 5.4) with advanced OA, this difference between mechanical and anatomical tibiofemoral angles (TFAs) fell in the range 6-7.5° [8], which aligns with our average difference of 6.3° LDFA in patients with a mean age of 70.51 ± 7.53. Our technique for identifying MPTA and LDFA estimates coronal alignment using anatomic axes, similar to the approach described by Chang et al [8] when measuring the TFA. Cooke described a consistent 4-5° offset between the femoral mechanical and anatomical axes, allowing approximation of mechanical alignment when LLRs are unavailable [12]. Similarly, Luis and Varatojo observed that the anatomic tibiofemoral angle tends to underestimate the mechanical axis by 4-6° of valgus [10]. Kraus et al recently used a 5° correction to the aLDFA on SLRs to determine the mechanical LDFA for CPAK classification; however, their study did not directly compare CPAK classifications derived from SLRs versus LLRs [7].
Although we observed a systematic 6.3° difference between short- and long-leg LDFA, applying a 5° correction factor yielded the highest CPAK classification agreement. With the 66% overall agreement in CPAK classification, this study demonstrates that SLRs, which are more widely available and easier to obtain, can reliably approximate CPAK classification compared to LLRs. This is likely explained by the fact that CPAK assigns categorical alignment types based on the intersection of distinct ranges of aHKA and JLO, rather than continuous variables [3]. As a result, even small shifts in angular measurements can cause cases near a category boundary to cross into an adjacent classification, reducing overall agreement. A 5° correction factor provided the optimal balance by minimizing misclassification across all CPAK categories, improving consistency while avoiding overcorrection.
Future Studies
An area of future study would be to identify the amount of femoral and tibial visualization necessary for an SLR to correctly classify CPAK. Also of interest may be the investigation of the differences in validity of CPAK by SLR in the preoperative versus postoperative environments, noting how deviations of aHKA and JLO between the two might affect patient-reported outcome measures and overall patient satisfaction. Another potential study would compare standard anteroposterior knee radiographs and full-length films to assess the accuracy of each CPAK component, including the aHKA, JLO, LDFA, and MPTA.
Conclusion
Our findings support the use of SLRs with a 5° correction to the LDFA as a reliable alternative to LLRs for CPAK classification. This method offers a practical, lower-cost option for preoperative alignment assessment, particularly in elderly patients with common CPAK phenotypes. While applicability may be limited in rarer alignment types, our results demonstrate strong inter- and intra-rater reliability and reinforce the utility of SLRs in settings where long-leg imaging is unavailable or impractical.
Author Contribution Statement
Conceptualization: T.B, J.S; Methodology, Supervision: T.B; Software, Validation, Formal analysis, Visualization: J.S; Investigation: A.B, N.G; Writing - Original Draft: A.B, N.G, C.B; Writing - Review & Editing: T.B, J.S, C.B, Z.R; Project administration: A.B, N.G, C.B, Z.R. All authors have read and agreed to the published version of the manuscript.
Ethics Approval Statement
This study was determined exempt by the Northside Hospital Institutional Review Board (#E297). The need for consent forms was waived due to the study design.
Acknowledgements
None
Funding
This study was unfunded.
Data Availability Statement
Data generated during this study are available from the corresponding author on reasonable request.
Conflict of Interest Statement
T.B. receives royalties and is a paid consultant for Zimmer Biomet and Total Joint Orthopaedics, and a board member of the Georgia Orthopaedic Society. J.S. is a member of the speakers bureau for DePuySynthes and is a board member of the Anterior Hip Foundation.
References
- Unal M, Ercan S, Budeyri A, Toprak U, Şalkaci A, et al. (2020) Anatomical axis validation of lower extremity for different deformities: A radiological study. SAGE Open Med 8: 2050312120923822.
- Graden NR, Dean RS, Kahat DH, DePhillipo NN, LaPrade RF, et al. (2020) True Mechanical Alignment is Found Only on Full-Limb and not on Standard Anteroposterior Radiographs. Arthrosc Sports Med Rehabil 2(6): e753-e759.
- MacDessi SJ, Griffiths-Jones W, Harris IA, Bellemans J, Chen DB, et al. (2021) Coronal Plane Alignment of the Knee (CPAK) classification. Bone Joint J 103-B: 329-337.
- Brouwer RW, Jakma TSC, Bierma-Zeinstra SMA, Ginai AZ,Verhaar JAN, et al. (2003) The whole leg radiograph Standing versus supine for determining axial alignment. Acta Orthopaedica 74(5): 565-568.
- Issa SN, Dunlop D, Chang A, Song J, Prasad PV, et al. (2007) Fulllimb and knee radiography assessments of varus‐valgus alignment and their relationship to osteoarthritis disease features by magnetic resonance imaging. Arthritis & Rheumatism 57(3): 398-406.
- Kazemi S-M, Qoreishi S-M, Maleki A, Minaei-Noshahr R, Hosseininejad SM, et al. (2022) Correlation of short knee and full-length X-rays in evaluating coronal plane alignment in total knee arthroplasty. Journal of Orthopaedic Surgery and Research 17(1): 378.
- Kraus KR, Deckard ER, Buller LT, Meding JB, Meneghini RM, et al. (2025) The Mark Coventry Award: Does Matching the Native Coronal Plane Alignment of the Knee Improve Outcomes in Primary Total Knee Arthroplasty? The Journal of Arthroplasty 40(7S1): S3-S11.
- Chang CB, Choi J-Y, Koh IJ, Seo ES, Seong SC, et al. (2010) What should be considered in using standard knee radiographs to estimate mechanical alignment of the knee? Osteoarthritis and Cartilage 18(4): 530-538.
- Alzahrani MM, Wood TJ, Somerville LE, Howard JL, Lanting BA, et al. (2019) Correlation of Short Knee Radiographs and Full-length Radiographs in Patients Undergoing Total Knee Arthroplasty. JAAOS - Journal of the American Academy of Orthopaedic Surgeons 27(11): e516-e521.
- Luís NM, Varatojo R (2021) Radiological assessment of lower limb alignment. EFORT Open Reviews 6(6): 487-494.
- Hsu RW, Himeno S, Coventry MB, Chao EY (1990) Normal axial alignment of the lower extremity and load-bearing distribution at the knee. Clin Orthop Relat Res (255): 215-227.
- Cooke TDV, Sled EA (2009) Optimizing Limb Position for Measuring Knee Anatomical Axis Alignment from Standing Knee Radiographs. The Journal of Rheumatology 36(3): 472-477.
- Hinman RS, May RL, Crossley KM (2006) Is there an alternative to the full‐leg radiograph for determining knee joint alignment in osteoarthritis? Arthritis & Rheumatism 55(2): 306-313.
- Colebatch AN, Hart DJ, Zhai G, Williams FM, Spector TD, et al. (2009) Effective measurement of knee alignment using AP knee radiographs. The Knee 16(1): 42-45.
- Kumar N, Yadav C, Raj R, Anand S (2014) How to Interpret Postoperative X‐rays after Total Knee Arthroplasty. Orthop Surg 6(3): 179-186.
- MacDessi SJ, Griffiths-Jones W, Harris IA, Bellemans J, Chen DB, et al. (2020) The arithmetic HKA (aHKA) predicts the constitutional alignment of the arthritic knee compared to the normal contralateral knee. Bone Jt Open 1(7): 339-345.
- Landis JR, Koch GG (1977) An Application of Hierarchical Kappa-type Statistics in the Assessment of Majority Agreement among Multiple Observers. Biometrics 33(2): 363-374.
- Fontalis A, Luyckx T, Vanspauwen T, Moreels R, Mancino F, et al. (2024) Strong Correlation Between Standing Long-Leg Radiographs and CT Scans in Measuring Coronal Knee Alignment. JBJS 106(15): 1373-1383.
- Ilahi OA, Kadakia NR, Huo MH (2001) Inter- and intraobserver variability of radiographic measurem nts of knee alignment. Am J Knee Surg 14(4): 238-242.
- Gieroba TJ, Marasco S, Babazadeh S, Bella CD, Bavel DV, et al. (2023) Arithmetic hip knee angle measurement on long leg radiograph versus computed tomography—inter-observer and intra-observer reliability. Arthroplasty 5(1): 35.
- Park A, Stambough JB, Nunley RM, Barrack RL, Nam D, et al. (2016) The Inadequacy of Short Knee Radiographs in Evaluating Coronal Alignment After Total Knee Arthroplasty. The Journal of Arthroplasty 31(4): 878-882.
- Bouché P-A, Stern H, Gasparutto X, Lubbeke A, Miozzari HH, et al. ( 2025) Coronal Plane Alignment of the Knee Classification in Osteoarthritic Knees: Poor to Moderate Reliability and Implications for Imaging Choice. The Journal of Arthroplasty. Epub ahead of print S08835403(25)00881-2.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.