Urinary and Hepatobiliary Complications in a Young Woman with Chronic Ketamine Use: A Case Report
by Fleurette Tatete Ambudihela1*, Sincaryl Tchouankeu2
1Department of Emergency Medicine, Helora University Hospital, Mons, Belgium
2Emergency Department of Centre Hospitalier Interrégional Edith Cavell (CHIREC) Delta site, Brussels, Belgium
*Corresponding author: Fleurette Tatete Ambudihela, Department of Emergency Medicine, Helora University Hospital, Mons, Belgium
Received Date: 07 July 2025
Accepted Date: 11 July 2025
Published Date: 14 July 2025
Citation: Tatete FA, Tchouankeu S (2025) Urinary and Hepatobiliary Complications in a Young Woman with Chronic Ketamine Use: A Case Report. Ann Case Report. 10: 2341. https://doi.org/10.29011/2574-7754.102341
Abstract
We report the case of a 24-year-old female chronic ketamine user (via inhalation), admitted to the emergency department for acute right flank pain. Clinical and paraclinical investigations revealed moderate renal impairment, biliary duct dilatation, and hepatic abnormalities. Urinalysis showed sterile pyuria with numerous granular casts. Blood tests revealed elevated liver enzymes and cholestatic markers. Abdominal CT imaging confirmed biliary and urinary tract dilatation without any identifiable obstruction. This clinical picture was consistent with ketamine-induced urinary and hepatobiliary tract injury, a rare but increasingly recognized complication among chronic users. This case highlights the importance for clinicians to consider substance use in the differential diagnosis of unexplained hepatobiliary and urinary symptoms in young patients.
Keywords: Chronic ketamine use; Substance abuse; Hepatic injury; Abdominal pain; Hydronephrosis; Urinary incontinence; Non-obstructive biliary dilatation; Case report; Urinary tract injury; Renal impairment.
Introduction
Ketamine is an N-methyl-D-aspartate (NMDA) receptor antagonist originally developed as an anesthetic agent. In recent years, its use has shifted toward recreational purposes, particularly among young adults, for its dissociative and hallucinogenic effects [1]. Alongside the rise in recreational use, a growing number of serious medical complications have been reported [2]. Urinary tract complications associated with chronic ketamine use, commonly known as “ketamine bladder syndrome,” are well documented. They include urinary frequency, pelvic pain, dysuria,
hematuria, and urinary incontinence. In severe cases, progression to bladder fibrosis, hydronephrosis, and renal failure can occur [3,4]. Hepatobiliary complications, although less frequently reported, are increasingly recognized. These include cholestasis, biliary duct dilatation, elevated liver enzymes, and, in some cases, bile duct fibrosis [5,6]. The underlying pathophysiological mechanisms remain incompletely understood but are thought to involve direct toxicity of ketamine metabolites on the biliary and urinary epithelia, microvascular injury, and chronic inflammatory processes [7]. We report the case of a 24- year-old female chronic ketamine user who presented with severe urinary and hepatobiliary complications. This case underscores the importance for clinicians to consider such complications in young patients with unexplained abdominal pain and highlights the need for early and appropriate management.
Case Report
A 24-year-old woman presented to the emergency department in January 2025, transported by ambulance for acute right flank pain. While on her way to a job interview, she experienced a vasovagal episode triggered by the intensity of the pain, which she rated as 8/10 on the Visual Analog Scale (VAS). The pain was colicky and non-radiating. The patient denied nausea, vomiting, gastrointestinal disturbances, urinary symptoms, or fever. Her medical history was notable for chronic ketamine use via inhalation, at a rate of 1 g per day for five years. She had made several attempts at detoxification in psychiatric settings. The first hospitalization in 2022 was voluntarily discontinued after one week. The second, in 2023, and the third, in January 2025, were also prematurely terminated against medical advice. Despite these attempts, the patient continued to use ketamine. Additionally, she reported longstanding urinary incontinence, which had been evolving over several months.
Upon admission, vital signs were stable: blood pressure 123/78 mmHg, heart rate 82 bpm, respiratory rate 18 breaths/min, oxygen saturation 98% on room air, body temperature 36.8°C. Clinical examination revealed right flank tenderness without signs of peritonitis. There was no costovertebral angle tenderness. Cardiopulmonary examination was unremarkable.
Initial laboratory investigations are summarized in Table 1, relevant for moderate renal impairment with a serum creatinine of 1.36 mg/dL and an estimated glomerular filtration rate (eGFR) of 48 mL/min/1.73 m². Urea was mildly elevated at 62 mg/dL. Liver function tests showed significant abnormalities with elevated transaminases (AST 98 U/L, ALT 143 U/L), marked elevation of cholestatic enzymes (GGT 1741 U/L, alkaline phosphatase 1081 U/L), and a total bilirubin of 0.28 mg/dL, indicative of cholestasis. Inflammatory markers were moderately elevated with C-reactive protein (CRP) at 15.3 mg/L, while the white blood cell count was normal at 9.81 × 10⁹/L. Urinalysis showed sterile leukocyturie with 450 leukocytes/μL and abundant epithelial cells. Numerous granular casts were observed under microscopy, indicating significant tubular injury. No bacterial growth was detected in urine culture, ruling out infectious etiology.
Abdominal computed tomography (CT) imaging revealed marked dilatation of intra- and extrahepatic bile ducts without lithiasis or obstructive mass (Figures 1 and 2). Additionally, an uneven dilatation of the urinary tract was noted (Figures 3 and 4). The liver parenchyma appeared homogeneous with no focal lesions. Irregular thickening of the bladder and urethral walls was also observed.
Following the initial diagnostic workup, the patient was admitted to the internal medicine department, where she was jointly managed by the gastroenterology and nephrology teams. Despite medical recommendations, the patient elected to leave the hospital against medical advice, before completion of further investigations and initiation of definitive management.
|
Parameters |
Results |
Normal value |
Units |
|
Hemoglobine |
10.7 |
11.7 – 15.1 |
g/dl |
|
Hematocrite |
32.3 |
35.4 - 46.1 |
% |
|
White blood cells |
9.81 |
3.80 - 9.39 |
10³/µL |
|
Neutrophiles |
5320 |
1660 – 5920 |
/mm³ |
|
Lymphocyt |
3450 |
940 - 3250 |
/mm³ |
|
Monocytes |
790 |
250 – 740 |
/mm³ |
|
Platelets |
432 |
175 - 343 |
10³/µL |
|
Fibrinogen |
5.4 |
1.7 - 4.2 |
g/L |
|
Sodium |
133 |
136 – 145 |
mmol/L |
|
Potassium |
3.8 |
3.5 - 5.1 |
mmol/L |
|
Chloride |
105 |
98 - 107 |
mmol/L |
|
HCO3- |
17 |
22 - 29 |
mmol/L |
|
Urea |
62 |
Oct-40 |
mg/dL |
|
Creatinine |
1.36 |
0.57 - 1.11 |
mg/dL |
|
eGFR |
48 |
> 60 |
mL/min/1.73m² |
|
CRP |
15.3 |
< 5 |
mg/l |
|
Total bilirubine |
0.28 |
0.20 - 1.20 |
mg/dL |
|
LDH |
217 |
125 - 220 |
U/L |
|
ALAT (SGPT) |
143 |
5 – 55 |
U/L |
|
Gamma-GT |
1741 |
< 38 |
U/L |
|
ALP |
1081 |
40 - 150 |
U/L |
|
Glucose |
114 |
70 - 105 |
mg/dL |
|
CK |
23 |
29 - 168 |
UI/L |
|
Lipase |
38 |
Aug-78 |
U/L |
Table 1: Biological findings on the day of admission.
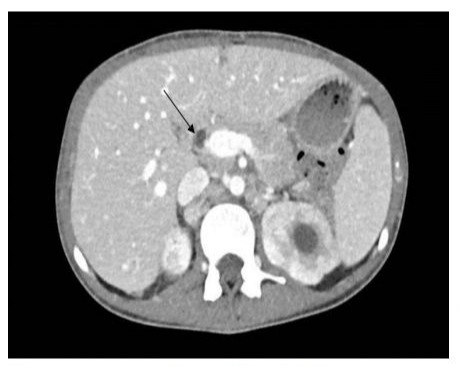
Figure 1: Contrast-enhanced abdominal CT-coronal section. (Note: Dilatation of the biliary ducts (solid black arrow)).

Figure 2: Contrast-enhanced abdominal CT–frontal section. Note: Dilatation of the biliary ducts (solid black arrow).
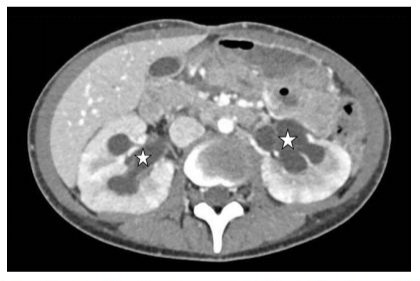
Figure 3: Coronal section of contrast-enhanced abdominal CT illustrating pyelocaliceal dilatation (white asterisk).”

Figure 4: Frontal slice of contrast-enhanced abdominal CT revealing moderate to severe pyelocaliceal dilatation (white asterisk).
Discussion
Chronic ketamine use is increasingly recognized as causing injuries to both the urinary and biliary tracts. While urinary complications are now well documented, hepatobiliary involvement remains less understood and is still underdiagnosed [1,2]. From a pathophysiological perspective, ketamine-induced urinary dysfunction involves several mechanisms. Ketamine and its metabolites exert direct cytotoxic effects on the urothelium, leading to epithelial denudation, chronic inflammation, and progressive fibrosis [3].
Additionally, microvascular injury contributes to ischemia and worsens tissue damage. These processes ultimately result in bladder wall thickening, loss of compliance, hydronephrosis, and, in advanced cases, renal failure [4]. In our patient, sterile pyuria with abundant epithelial cells and granular casts reflected significant tubular injury consistent with these mechanisms. Hepatobiliary complications, though less frequently reported, are now better characterized in chronic ketamine users.
Proposed mechanisms include direct toxicity of ketamine metabolites on cholangiocytes, leading to cholestasis and bile duct fibrosis [5]; dysregulation of bile flow, possibly mediated by interactions with NMDA receptors in biliary cells and modulation of the sphincter of Oddi [6]; and chronic inflammatory responses promoting progressive bile duct fibrosis [7].
In our patient, the combination of significant biliary duct dilatation, elevated cholestatic enzymes, and absence of obstructive lesions on imaging supported these pathophysiological hypotheses. The temporal association between chronic ketamine use and the concurrent development of urinary and hepatobiliary complications in our patient strongly suggests a causal relationship. Alternative etiologies for biliary duct dilatation and hydronephrosis were systematically excluded through comprehensive diagnostic workup. Management of these complications primarily involves immediate cessation of ketamine use [8].
Close monitoring of renal and hepatic function is necessary, along with symptomatic management and treatment of any complications (such as urinary retention or biliary obstruction). In severe cases, urological interventions (such as bladder augmentation) or hepatobiliary procedures may be required [9]. Prognosis remains variable; progression to irreversible fibrosis and permanent renal and hepatic dysfunction is possible even after ketamine cessation [10]. This case highlights the importance of considering recreational drug use, particularly ketamine, in the differential diagnosis of unexplained abdominal pain and multiorgan involvement in young patients. Early recognition and prompt management are essential to prevent irreversible damage. Moreover, greater awareness among healthcare professionals is needed given the rapid rise in recreational ketamine use and the severity of its potential complications.
Conclusion
Chronic ketamine use can cause severe complications affecting both the urinary and hepatobiliary systems, including sterile pyuria, hydronephrosis, bile duct dilatation, and hepatic dysfunction. Early recognition of these complications is crucial to initiate appropriate management and prevent irreversible damage. Clinicians should remain vigilant for this association in young patients presenting with unexplained abdominal pain and multiorgan involvement. Immediate cessation of ketamine use is the cornerstone of treatment. Close monitoring of renal and hepatic function, along with multidisciplinary management, is essential to optimize outcomes.
References
- Tsai TH, Cha TL, Lin CM, Tsao CW, Tang SH, et al. (2009) Ketamineassociated bladder dysfunction. Int J Urol. 16:826-829.
- Shahani R, Streutker C, Dickson B, Stewart RJ. (2007) Ketamineassociated ulcerative cystitis: a new clinical entity. Urology. 69:810812.
- Mak SK, Chan MT, Bower WF, Yipm SKH, Hou SSM, et al. (2011) Lower urinary tract changes in young ketamine abusers. Hong Kong Med J. 17:463-468.
- Pal R, Navaneethan U, Konjeti R, Thati V. (2017) Hepatobiliary and pancreatic complications of chronic ketamine abuse. Clin Gastroenterol Hepatol. 15:1392-1393.
- Ng SH, Lee JH, Chuang FP, et al. (2018) Hepatobiliary and pancreatic complications of ketamine abuse. J Med Imaging Radiat Oncol. 62:740-746.
- Wood D, Cottrell A, Baker SC, Southgate J. (2011) Recreational ketamine: from pleasure to pain. BJU Int. 107:1881-1884.
- Yeung LY, Rudd JH, Dhillon AP. (2014) Ketamine: a rare cause of cholangiopathy with biliary dilatation. World J Hepatol. 6:668-672.
- Chu PS, Kwok SC, Lam KM, Chu TY, Chan SWH, et al. (2007) ‘Street ketamine’-associated bladder dysfunction: a report of ten cases. Hong Kong Med J. 13:311-313.
- Cottrell AM, Gillatt DA. (2008) Ketamine-associated urinary tract pathology: the tip of a new iceberg? BJU Int. 102:117-118.
- Wong SW, Lee KF, Wong J, Ng WWC, Cheung YS, et al. (2014) Dilated common bile ducts in ketamine abusers: a novel finding. Clin Gastroenterol Hepatol. 12:1149-1150.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.