Ureteral Transitional Cell Carcinoma with Cervical Lymph Node Metastasis: A Case Report
by Mohamed Elghobashy1, Tarek Shrayyef1, Javier Mohigefer2, Abdul Matin1*
1Department of Otorhinolaryngology, Limerick University Hospital, Ireland
2Department of Histopathology, Limerick University Hospital, Ireland
*Corresponding author: Abdul Matin FRCS,FACS, Consultant ENT & Head Neck Surgeon, Limerick University Hospital, Ireland
Email: matinfrcs@yahoo.com
Received Date: 14 May 2025
Accepted Date: 17 May 2025
Published Date: 19 May 2025
Citation: Elghobashy M, Shrayyef T, Mohigefer J, Matin A (2025) Ureteral Transitional Cell Carcinoma with Cervical Lymph Node Metastasis: A Case Report. Ann Case Report. 10: 2292. https://doi.org/10.29011/2574-7754.102292
Abstract
Cervical lymph nodes are a common site of metastases for malignant tumors that originate at primary sites in the head and neck. Transitional cell carcinomas (TCCs), also termed urothelial carcinomas, account for nearly 90% of all ureteral cancers. Few cases have reported such cancer spreading to the cervical lymph nodes. We present a case of a75-year old gentleman who presented at our ENT Out Patient Department with a left side neck swelling since June 2024.
A diagnostic work up including CT neck, fine needle aspiration cytology and ultrasound guided core biopsy was done and confirmed the diagnosis of metastatic cervical transitional cell carcinoma. This man is a known case of ureteric transitional cell carcinoma with paraaortic lymph node metastasis since 2018. A recurrence of tumor in bladder and prostate was reported. Right nephroureterectomy, chemotherapy and external beam radiotherapy were applied. A brief review of this rare case including clinical presentation and diagnostic work up will be discussed.
Keywords: Transitional Cell Carcinoma; Urothelial Carcinoma; Ureter; Metastasis; Cervical Lymph Nodes.
Introduction
Ureteral transitional cell carcinoma (TCC) is a type of cancer that affects the lining of the ureter, sharing a common histological subtype and risk factor profile to bladder TCC. Gross or microscopic hematuria is the most common symptom, being present in over 75% of patients [1]. The typical spread of ureteral TCC is to regional lymph nodes such as the iliac, common iliac, external iliac, internal iliac and para-aortic nodes.
However, lymph node metastasis above the diaphragm especially in head and neck region is extremely rare. Only few reports have been published so far and with poor prognosis [2]. We report a case of patient with transitional cell carcinoma of right ureter with solitary left cervical lymph node metastasis without any bony or visceral metastasis.
Case Report
A75-year old man who was diagnosed as high grade invasive urothelial carcinoma of the right ureter (PT1 grade 3) in 02/2018. So, laparoscopic assisted right nephroureterectomy was done.
6 months later, an extensive paraaortic lymphadenopathy with metastasis to urinary bladder were reported. Then, he underwent 6 cycles of chemotherapy (carboplatin and gemcitabine).
In December 2019, a multifocal high grade tumor recurrence in bladder was recorded. So, cystoscopy and transurethral resection of tumor was done.
In 04/2021, metastasis of tumor to prostate was elicited. Then, a combined external beam radiotherapy and hormonal therapy was given.
In November 2024, he attended to ENT clinic with a history of left side painless neck swelling since June 2024. There is no dysphagia, odynophagia or difficulty in breathing with mild hoarseness of voice.
He also has mild left ear pain with no hearing impairment, tinnitus or vertigo. Also, no nasal obstruction, sneezing or headache.
External neck examination revealed, a- 3x4 cm left level 4 neck swelling was observed. It was hard, fixed and not tender, with normal overlying skin and no other neck swellings.
Otoscopic assessment showed bilateral normal external and middle ears with bilateral intact tympanic membranes.
Anterior rhinoscopy and throat examination were unremarkable.
Flexible naso-laryngoscopy reflected no pathological lesion in nose, nasopharynx, epiglottis, aryepiglottic folds, arytenoids, false and true vocal cords and pyriform fossae with bilateral freely mobile vocal cords (Figure 1).
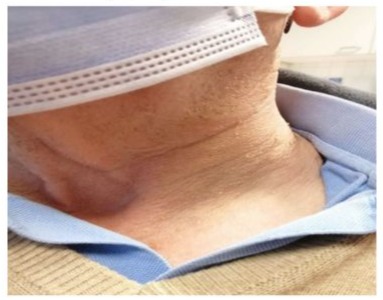
Figure 1: left level 4 cervical lymph node.
Fine needle aspiration cytology was performed and the result announced scattered predominantly small mature appearing lymphocytes with occasional larger forms and rare loose aggregate of histocytes suggestive of poorly formed granuloma. Additional tissue sampling was recommended.
CT neck was done and declared marked interval enlargement of left sided cervical chain lymph node level 3/4a measuring 3.4 cm. It is irregular in appearance, demonstrates heterogenous enhancement and has effaced/displaced local structures. Findings highly suspicious for a metastatic lymph node (Figure 2).
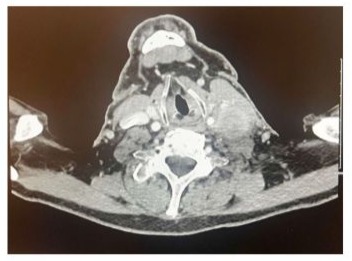
Figure 2: CT neck with contrast showing marked interval
To confirm the diagnosis, an ultrasound guided core biopsy was performed and the findings revealed lymph node fragments infiltrated by metastatic poorly differentiated carcinoma. The histopathological features and the immunological profile suggest a bladder origin (Figure 3).
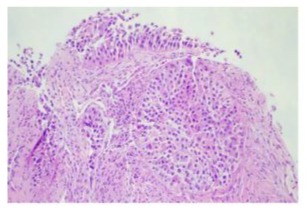
Figure 3: Malignant infiltration composed by nets of discohesive high grade cells with some rhabdoid features.
Whole body PET/CT scan was done and showed FDG avid 6.4x4.0 cm left level 3/4 cervical mass, SUV 18.5, with no suspicious FDG uptake elsewhere (Figure 4).
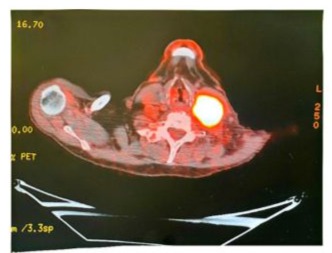
Figure 4: PET/CT scan was done and showed FDG avid 6.4x4.0 cm left level 3/4 cervical mass, SUV 18.5.
The case was discussed in the MDT meeting and the outcomes is to refer him to medical oncology department.
Discussion
The cervical lymph nodes are a common site of metastasis for cancers originating in the head and neck and upper aerodigestive tract. Rarely, cancers originating from sites other than the head and neck can metastasize to the cervical lymph node chain. However, genitourinary tract tumors especially renal cell carcinomas make up a significant proportion of these cancers and should be considered in the differential diagnosis of metastatic lesions of the head and neck [3]. According to one large retrospective autopsy data, metastases of bladder cancer to the cervical or axillary lymph node sites occur in a very low rate [4]. A 9-year review of patients with head and neck metastases from 845 urogenital tract tumors (kidney, prostate, bladder, testes, penis, urethra and ureter) showed that only 31 (3.7%) of these tumors developed metastases to the cervical and supraclavicular lymph nodes [5]. There has been one case report of transitional cell cancer of Published by Sciedu Press 61 www.sciedu.ca/jst Journal of Solid Tumors, June 2012, Vol. 2, No. 3 the bladder is mentioned that manifested as an extensive large lymph node metastasis involving the intra-parotid, supraclavicular, axillary and regional abdominal and pelvic lymph nodes without bone or visceral organs involved [6]. The possible route of spread to head and neck region is by hematogenous through vertebral veins and by lymphatics [7]. Due to few case reports and shorter survival rates; it is difficult to comment on standard treatment of metastatic cervical lymph nodes.
However, in many patients, palliative radiation therapy and chemotherapy has been offered [8]. In conclusion, genitourinary tumors especially bladder cancer has been shown to metastasize to cervical and axillary lymph nodes in rare instances.
Therefore, the work-up of new head or neck lesions with past history of bladder cancer should include metastases as part of the differential diagnosis.
References
- Kirkali Z, Tuzel E. (2003) Transitional cell carcinoma of the ureter and renal pelvis. Crit Rev Oncol Hematol 47:155–69.
- Ferlito A, Shaha AR, Buckley JG, Caruso G, Rinaldo A. (2001) Metastatic cervical lymph nodes from urogenital tract carcinoma: A diagnostic and therapeutic challenge. Acta Otolaryngol. 121:556-64.
- Ogunyemi O, Rojas A, Hematpour K, Rogers D, Head C, et al (2010) Metastasis of genitourinary tumors to the head and neck region. Eur Arch Otorhinolaryngol. 267:273-79.
- Wallmeroth A, Wagner U, Moch H, Gasser TC, Sauter G, et al (1999) Patterns of metastasis in muscle invasive bladder cancer (pT2-4): An autopsy study on 367 patients. Urol Int. 62:69-75.
- Hessan H, Strauss M, Sharkey FE. (1986) Urogenital tract carcinoma metastatic to the head and neck. Laryngoscope. 96:1352-56.
- Kancharla VP, Gulmi FA, Agheli A, Degen M, Gohari A, Jiang M, et al. (2010) Transitional Cell Carcinoma of the Bladder Manifestating as Malignant Lymphoma with Generalized Lymphadenopathy. Case Rep Oncol. 3:125-30.
- Tunio M, Rafi M, Hashmi A, Mohsin R, Raza SS. (2011) Choroidal metastasis from primary transitional cell carcinoma of urinary bladder: A case report and review of literature. Rawal Med J. 36:69-70.
- Sengelov L, Kamby C, von der Masse H. (1996) Pattern of metastases in relation to characteristics of primary tumor and treatment in patients with disseminated urothelial carcinoma. J Urol. 155:111-14.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.