Unusual Finding of a Leiomyoma in Transplanted Kidney-Review of Literature and Implications for Management
Snehal Shrivastava1, Dalia Ibrahim2, Amira Gohara3, Shobha Ratnam4
1University of Toledo Medical Center, Division of Nephrology, USA
2University of Toledo Medical Center, Department of Pathology, USA
3University of Toledo Medical Center, Department of Pathology, USA
4University of Toledo Medical Center, Division of Nephrology, USA
*Corresponding author: Snehal Shrivastava, University of Toledo Medical Center, Division of Nephrology, 2846 Maple Colony Dr. Toledo 43617, USA. TEL: +1 419 260 2689; E-mail : Snehal.shrivastava@utoledo.edu; snehalshri@gmail.com
Received Date: 29 September, 2018; Accepted Date: 30 October, 2018; Published Date: 06 November, 2018
Citation: Shrivastava S, Ibrahim D, Gohara A, Ratnam S (2018) Unusual Finding of a Leiomyoma in Transplanted Kidney-Review of Literature and Implications for Management. J Neph Urol: JNAU-111. DOI: 10.29011/ JNAU-111. 000011
1. Abstract
A 34-year-old lady presented with acute allograft dysfunction four years after renal transplant. She had stopped her immunosuppression five months prior to presentation. Biopsy of the transplanted kidney showed acute cellular rejection and a leiomyoma was reported as an incidental finding. Allograft dysfunction was attributed to rejection, that was treated with pulse dose of steroids and anti-thymocyte globulin after which renal function improved significantly. New immunosuppression regimen with Sirolimus, Mycophenolate and corticosteroid was started, and calcineurin inhibitor was excluded. Close follow up with periodic Epstein Barr Virus (EBV) testing and allograft ultrasound were planned to monitor the progression of the leiomyoma.
In this case, the etiology of the leiomyoma remains speculative; either De Novo from reactivation of EBV, or present in the donor transplanted kidney. The treatment, however was changed due to the presence of Leiomyoma.
2. Introduction
Leiomyomas are smooth muscle tumors that commonly arise in the uterus. Leiomyoma of the transplanted kidney is rare. When found, leiomyomas of renal allograft are often related to infection with or reactivation of EBV. Only two cases of these tumors have been reported, one in adult and one in pediatric transplanted kidney [1,2]. There are eighteen reported cases of leiomyomas developing in extra-renal locations, such as the brain, lungs, liver after renal transplant. Solid tumors and malignancies are common in immunocompromised state such as that introduced after renal transplant [3]. Most of these malignancies are related to reactivation or infection with viruses such as EBV, EMV and due to carcinogenic effect of immunosuppressive medications commonly used after transplant.
Thus, accurate diagnosis of Leiomyoma in the renal allograft is important and differentiation from other malignant neoplasms is essential, as this alters patient management and outcomes.
3. Case Description
A 34-year-old lady with history of renal transplant four years ago presented with worsening left sided abdominal pain located at the site of her renal allograft. Initial laboratory works up showed a sharp decline in renal function with a creatinine of 5.78 mg/dl with an estimated Glomerular Filtration Rate (GFR) of 9ml/min. Pertinent positive findings on clinical assessment were high BP of 159/97 and significant lower extremity edema. Urine analysis was significant for mild proteinuria but no hematuria or signs of infection.
Computed Tomography scan of the abdomen and pelvis showed diffusely enlarged renal allograft measuring 15.6 cms x 9.8cms x 9.1cms without any hydronephrosis, calculi or masses. Doppler Ultrasound showed similar findings with perinephric collection, but no renal artery stenosis. Transplant biopsy showed acute cellular rejection of the renal allograft with interstitial infiltration with lymphocytes, plasma cells, and occasional eosinophils classified as Banff IB (Image 1).
There was a small well circumscribed Leiomyoma which was reported as an incidental finding. Whorls of bland spindle cells lacking mitotic figures (Image 2, 3) were noted. Biopsy also showed hypertensive and diabetic nephrosclerosis of the vessels. Upon additional questioning, it was noted that the patient had stopped her immunosuppressive medications five months prior to this presentation with acute renal failure. She had received a living related donor renal transplant, 4 years ago with zero HLA mismatch. The donor and recipient were positive for EBV and Cytomegalovirus (CMV) antibodies. Post-transplant immunosuppression regimen consisted of Tacrolimus (calcineurin inhibitor) and Everolimus (mammalian target of rapamycin inhibitor, mTORi).
4. Differential Diagnoses
Differential diagnoses for Leiomyoma in the graft were Leiomyosarcoma, angiomyolipoma, and renal cell carcinoma [4,5]. These were ruled out based on histologic findings. Leiomyoma in the presented case histologically consisted of whorls of cytologically bland spindle cells with abundant eosinophilic cytoplasm (Image 1). On high resolution microscopy, it revealed absence of cytologic atypia and mitotic figures (Image 2).
The histologic features of a Leiomyosarcoma are abundant mitotic figures, nuclear pleomorphism, and nuclear hyperchromatism that were not seen in our case.
Angiomyolipoma consists of an admixture of adipose tissue, blood vessels with thickened walls and smooth muscles, a characteristic finding called triphasic histology. This was also excluded in the above renal tissue. Renal Cell Carcinomas (RCC) may present histologically with sarcomatous features such as spindle cells. RCCs stain positive for cytokeratin and invade the surrounding tissue which not seen on the above biopsy sample. Immunohistochemical staining with epithelial cell marker and RCC marker also aid in the diagnosis of RCC but were not performed in our case owing to the absence of other histological features if RCC.
5. Treatment
The patient was treated with high dose steroids (0.5 mg/kg daily for three doses) and anti-thymocyte globulin (1.5 mg/kg/day for five doses) for acute allograft rejection. Her renal function slowly improved to a nadir creatinine of 2.7mg/dl and GFR of 19ml/min. The leiomyoma was managed conservatively with periodic surveillance imaging and EBV titers. The immunosuppression regimen was changed to Mycophenolate mofetil, Sirolimus and Prednisone.
6. Follow-up
Patient is seen in the Renal transplant clinic every 2-3 months and close surveillance is done for signs of increase in the size of leiomyoma or occurrence of other solid tumors.
7. Discussion
Literature review though various search engines revealed that there were only two reported cases of leiomyomas arising in the renal allografts [1,2], one in an adult recipient and the other in a pediatric recipient. In the described case of leiomyoma in the pediatric transplant patient, the tissue was positive for Episten Barr Virus (EBV) [2,6,7]. Among the recipients of renal transplants, there were eighteen reported cases of leiomyomas in extra-renal locations such as brain, liver and lung. All these individuals were immunocompromised from anti-rejection medications for their transplanted organs. Extra uterine leiomyomas have also been described in adult and pediatric HIV positive population [8]. Most of the described cases of leiomyomas in immunocompromised patients were noted to be EBV positive.
The origin of leiomyoma in our report was speculative. Possibly, the tumor was present in the donor kidney and was incidentally noted on biopsy. It was also likely that the tumor was initiated de-novo in the transplanted kidney given the positive EBV status of both the donor and recipient. Tissue EBV testing of our patient was not completed due to small tumor size and small amount of leiomyoma tissue obtained on biopsy. Prior to this finding, patient was immunosuppressed and was treated with calcineurin inhibitor. In the light of the new tumor, she was placed on a calcineurin inhibitor free immunosuppressive regimen to reduce the rate of growth of tumor and decrease the chances of new malignancies.
8. Conclusion
Leiomyomas of the transplanted renal allograft are rare. EBV associated leiomyomas are common in immunocompromised patients, however de-novo development is also noted. When present, diagnosis and differentiation from other malignant neoplasms is imperative due to its impact on management, and choice of immunosuppressive agents in such individuals.
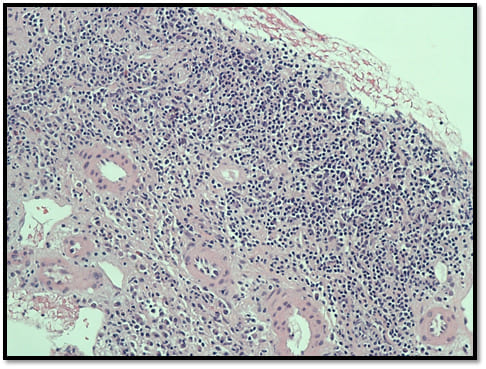
Image 1: Renal Allograft biopsy with lymphocyte, plasma cells and occasional eosinophil infiltration: Acute Rejection.
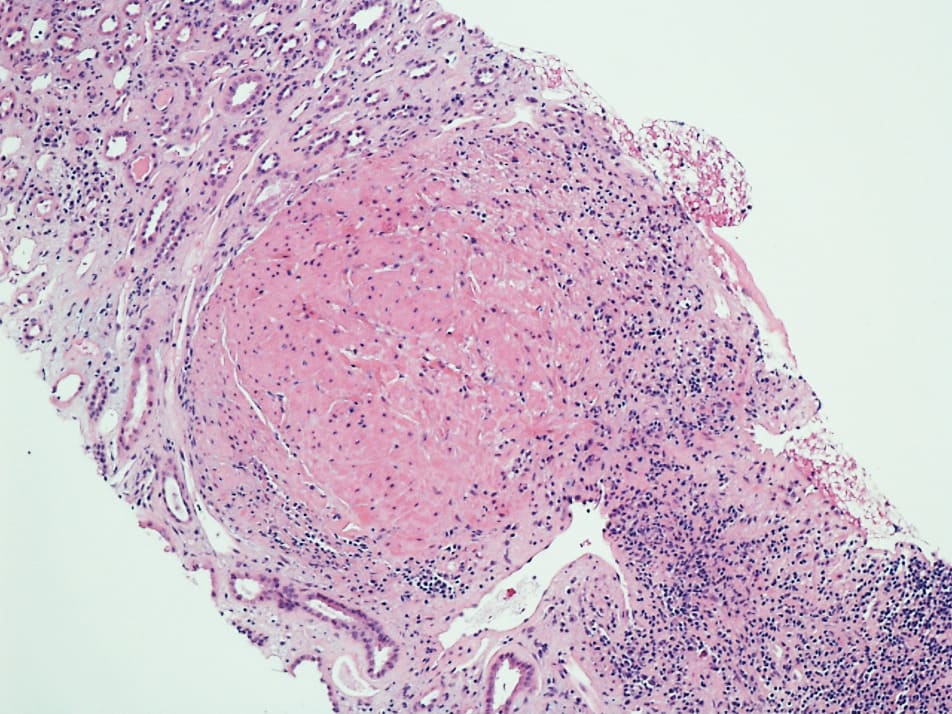
Image 2: Low-power view showing leiomyoma with whorls of cytologically bland spindle cells and prominent eosinophilic cytoplasm.
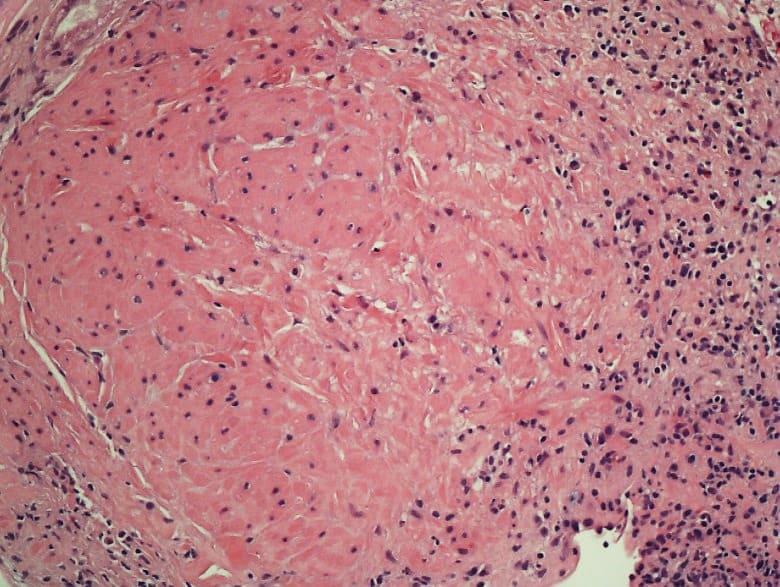
Image 3: High resolution image: leiomyoma characterized by the absence of significant cytologic atypia and mitotic activity.
- Li YJ, Siriwardana AR, Penn Symons JL, O’Neill GF, Qiu MR, et al. (2016) Leiomyoma in a Renal Allograft. Case Reports in Urology 2016: 4.
- Dionne JM, Carter JE, Matsell D, Macneily AE, Morrison KB, et al. (2005) Renal Leiomyoma Associated with Epstein-Barr Virus in a Pediatric Transplant Patient. American Journal of Kidney Diseases 46: 351-355.
- Penn I (2000) Post-transplant malignancy: the role of immunosuppression. Drug Saf 23:101-113.
- Khetrapal S (2014) Renal Leiomyoma: An Uncommon Differential Diagnosis of Renal Masses with a Clinical Relevance. Journal of Clinical and Diagnostic Research.
- Patil P, McKenney J, Trpkov K, Hes O, Montironi R, et al. (2015) Renal leiomyoma. A contemporary multi-institution study of an infrequent and frequently misclassified neoplasm. The American Journal of Surgical Pathology 39: 349-356.
- Larbcharoensub N, Limprasert V, Pangpunyakulchai D, Sanpaphant S, Wiratkapun C, et al. (2017) Leiomyoma: A Case Report and Review of the Literature. Urology Case Reports 13: 3-5.
- Lee ES, Locker J, Nalesnik M, Reyes J, Jaffe R, Alashari M, et al. (1995) The Association of Epstein-Barr Virus with Smooth-Muscle Tumors Occurring after Organ Transplantation. New England Journal of Medicine 332: 19-25.
- Sharif M, Seelall V (2011) Endobronchial Epstein Barr Virus-Associated Leiomyoma: An Unusual Finding in an Adult AIDS Patient. Chest 140: 80.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.