Undescended Testis: Timing of Surgery and Patient Follow-Up
by Christopher Amah, Ijeoma Obianyo*, Nene Agugua-Obianyo
Department. of Paediatric Surgery, University of Nigeria Teaching Hospital, Enugu, Nigeria
*Corresponding author: Ijeoma Obianyo, Department. of Paediatric Surgery, University of Nigeria Teaching Hospital, Enugu, Nigeria
Received Date: 20 July 2025
Accepted Date: 05 August 2025
Published Date: 08 August2025
Citation: Amah C, Obianyo I, Agugua-Obianyo N (2025) Undescended Testis: Timing of Surgery and Patient Follow-Up. Arch Surg 5: 130 https://doi.org/10.29011/3066-2559.000130
Abstract
Background: The current recommended age of orchidopexy in Undescended Testis (UDT) is 6 - 18 months. The main goal of this timing is to allow time for complete descent, to prevent the impairment of spermatogenesis, and to decrease the risk of malignancy in later life.
Objective: To study the timing of surgery and post-operative follow-up in children managed for UDT.
Patients and method: We performed a retrospective review of UDT managed between Jan 2013 and Dec 2022, at the University of Nigeria Teaching Hospital (UNTH), Enugu, Nigeria. Data extracted from ward, operating theater and medical records department were entered into specifically designed pro-forma. The data were collated and analyzed by univariate analysis.
Results: A total of 102 UDT patients were managed during the 10-year period, but only the clinical records of 90 patients with 115 UDT were accessible for review. This comprised 65 (72.2%) unilateral and 25 (27.8%) bilateral cases. Mean age at operation was 6.6 years. Mean length of post-operative follow up was 5.2 months. Short term outcome was satisfactory in all patients. There was no long-term follow-up for infertility and malignancy.
Conclusion: Majority of UDT in this study presented late and thus operated on late. Patients presenting late, should be enlisted into a strict and well-defined protocol of long-term follow-up. We advocate for awareness campaign to reduce the delay in presentation.
Keywords: Follow-up; Timing; Undescended testis
Introduction
Undescended Testis (UDT) is the commonest congenital abnormality of the genito-urinary tract in boys [1-3]. The incidence varies with gestational age at birth, affecting 2-5% of full term and 30% of preterm neonates. Descent of testis continues after birth, but it is now known that beyond 6 months of age spontaneous descent of the testis rarely occurs [1,3,4]. UDT may be situated along its normal route of descent or in an ectopic position.
It may be unilateral or bilateral, clinically palpable or non-palpable, and prone to complications such as trauma, torsion, infertility, and malignancy. The diagnostic tools used to detect UDT include physical examination, radiological technique, hormonal assay, and laparoscopic procedure [2,3,5,6]. Different imaging techniques have been evaluated for the assessment of UDT, but above all ultra-sonography with a high-resolution transducer (>7.5MHz) offers the greatest accuracy in the assessment of 100% of palpable and about 85% of non-palpable UDT [3,6]. When the testis is non palpable, diagnostic laparoscopy through an umbilical port is the procedure of choice [6,7]. Surgery is the treatment of choice, and orchidopexy is successful in up to 95% of UDT with a low rate of complications, about 1% [3]. The optimal time for orchidopexy has remained a subject of debate for decades. Current consensus and guidelines from the scientific community recommend that orchidopexy should be performed as early as 6 - 18 months of age, or at 1st presentation if diagnosed later [3,8]. The main goal of this timing of treatment is to prevent the impairment of spermatogenesis leading to infertility, and to decrease the risk of malignancy in later life. These two factors are outcomes in the management of UDT that require long term follow up.
Study Objective
We studied the two determinant factors - timing of surgery and post operative follow up, in the management of UDT, to determine their pattern.
Patients and Method
This is a 10-year retrospective review of children managed for UDT between Jan 2013 and Dec 2022, at UNTH Enugu, South East Nigeria. Data extracted from wards, operating theater and medical records department of the hospital were entered into proforma designed for the study. Demographic data collected included, age at presentation, whether unilateral or bilateral, palpable or non-palpable, associated anomalies, method of diagnosis, age at operation, type of operation, complications, outcome and length of post-op follow up. The data were analyzed using Statistical Package for Social Sciences (SPSS) version 25.
Results
A total of 102 children were managed for UDT during the 10- year study period, but only the clinical records of 90 children with 115 UDT were accessible for review in this study, comprising 65(72.2%) unilateral and 25(27.8%) bilateral cases. 75(65.2%) out of the 115 UDT were palpable and 40(34.8%) non palpable (Figure 1). Age at first presentation ranged from 4 months to 16 years, with a mean age of 6.4 years, 9(10%) of the patients presented before 1 year of age, 12 (13.3%) at age 1-2years, 15(16.7%) at age 2-5years, and 54 (60%) above 5 years of age (Table 1). Localization of the testis was clinical in 42 (46.7%) cases, by ultrasonography in 47 (52.2%). 1(1.1%) patient had impalpable testis localized by MRI (Table 2). 108 (93.9%) orchidopexies were performed, while 7 patients (6.1%) had unilateral orchidectomy for atrophic testes. No patient had surgery before age 1 year, 16 (17.8%) had at 1-2 years, 20(22.2%) at 2-5 years, and 54 (60%) above 5 years (Table 3). Short term outcome was satisfactory in all patients with no significant complications. Mean length of post-operative followup is 5.2 months. There was no long-term follow-up of patients for infertility and malignancy.
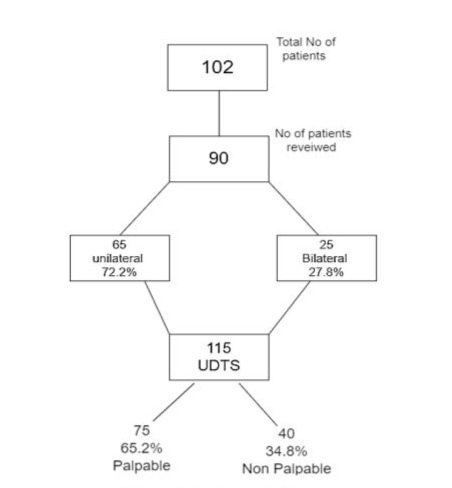
Figure 1: Study population.
|
Age |
No of patients |
Percentage |
|
<1yr |
9 |
10 |
|
1yr - 2 yrs |
12 |
13.3 |
|
>2yrs - 5yrs |
15 |
16.7 |
|
>5yrs |
54 |
60 |
|
Total |
90 |
100 |
Table 1: Age at Presentation.
|
Method |
No of patients |
Percentage |
|
Clinical assessment |
42 |
46.7 |
|
Ultrasonography |
47 |
52.2 |
|
MRI |
1 |
1.1 |
|
Laparoscopy |
0 |
0 |
|
Total |
90 |
100 |
Table 2: Localization of the testis.
|
Age |
No of patients |
Percentage |
|
<1yr |
0 |
0 |
|
1yr - 2 yrs |
16 |
17.8 |
|
>2yrs - 5yrs |
20 |
22.2 |
|
>5yrs |
54 |
60 |
|
Total |
90 |
100 |
Table 3: Age at Operation.
Discussion
This study revealed that 88% patients had orchidopexy by age 2years, and 60% by 5 years. This, with its potential consequences is beyond the current recommended age of 6 - 18 months [3,8]. The testis, for the function of spermatogenesis leaves its original intra-abdominal location for an extra-corporeal abode, in search of a lower ambient temperature (2-4o C lower than core temp), which the scrotum provides by virtue of its unique thermoregulatory anatomical features [3,9]. The fetal/neonatal germ cells of the testis (the gonocytes), subsequently undergo transformation into spermatogonia, the precursor cells for spermatogenesis at puberty. In the meantime, and very importantly, there is clearance of any remaining unused, undifferentiated fetal germ cells by apoptosis, so that by 2 years of age there are none left in the testis. The inhibition of this fetal germ cell transformation in UDT leads to a deficient pool of stem cells for post pubertal spermatogenesis, and infertility. In addition, persisting undifferentiated germ cells may become malignant after puberty [3,10]. Approximately 10% of infertile men have a history of cryptorchidism. Also, about 10% of all cases of Testicular Germ Cell Tumours (TGCT) - seminomas &embryonal carcinomas - develop in men with history of cryptorchidism, with the peak age incidence of 20 - 30 years [3,11]. Unfortunately, the mean post operative patient follow-up in this study was 5.2 months, after which the patients were lost to follow up. This is not much different from the findings in other studies within the sub-region [12-14]. There is no definite protocol for post-op follow up in UDT within the sub-region, despite the fact that majority of the patients are operated upon at very late age [15,16].
Conclusion
The management of UDT in our environment does not include any definite protocols for long term follow up of patients for infertility and neoplasm. There is need to raise awareness of the importance of early presentation and timely treatment of UDT. Patients with UDT presenting late, should be enlisted into a strict and welldefined protocol of long term follow up for infertility and testicular neoplasm.
References
- Hadley M Wood, Jack S. Elder (2009) Cryptorchidism and Testicle cancer: Separating fact from fiction: J of Urol 181: 452-461.
- Mathers MJ, Sperling H, Rübben H, Roth S (2009) The Undescended Testis: Diagnosis, Treatment And Long-Term Consequences. DtschArztebl Int 106: 527-532.
- Jerzy K. Niedzielski, Elżbieta Oszukowska, Jolanta SłowikowskaHilczer (2016) Undescended Testis - Current Trends and Guidelines: A Review of the Literature, Arch Med Sci 3: 667-677.
- David L. Wenzler, David A. Bloom, John M. Park (2004) What is the rate of spontaneous testicular descent in infants with cryptorchidism? J Urol 171: 849-851
- Ekenze SO, Nwankwo EP, Okere PCN (2013) The Utility Of Ultrasonography In The Management Of Undescended Testis In A Developing Country, World Journal of Surgery 37: 1121-1124.
- Iskandar Rahardjo Budianto, Hock Lim Tan, Yoshiaki Kinoshita, Riana Pauline Tamba, Satoshi Leiri, et al. (2014) Role Of Laparoscopy And Ultrasound In The Management Of “Impalpable Testis” In Children, Asian Journal of Surgery 37: 1015-9584.
- Mehendale VG, Shenoy SN, Shah RS, Chaudhari NC, Mehendale AV (2013) Laparoscopic Management Of Impalpable Undescended Testes: 20 Years’ Experience. J Minim Access Surg 9: 149-153.
- Ivana Fratri T, Dragan Šarac, Jelena Anti T, Marina Yermanov, Radoica Joki T (2018) Impalpable Testis: Evaluation Of Diagnostic And Treatment Procedures and Our Treatment Protocol, HindawiBioMed Research International, Article ID 3143412.
- Iskandar Rahardjo Budianto, Hock Lim Tan, Yoshiaki Kinoshita, Riana Pauline Tamba, Satoshi Leiri, et al. (2014) Role of Laparoscopy and Ultrasound In The Management of “Impalpable Testis” in Children, Asian Journal of Surgery 37: 200-204.
- C Kollin, JB Stukenborg, M Nurmio (2012) Boys with undescended testes: Endocrine, volumetric and morphometric studies on testicular function before and after orchidopexy at nine months or three years of age. J Clini Endocrinol Metab 97: 4588-4595.
- Docimo S (1996) Testicular Descent and Ascent in the first year of life. J Urol 48: 458-460.
- Ozgui Pirgon, Bumin Nuri Dunder. Vanishing Testis (2012) A Literature Review. J. Clini Res Pediatr Endocrinol 4: 116-120.
- Williams EV, Appanna T, Foster ME (2001) Management of the impalpable testis: a six-year review together with a national experience, Postgrad Med J 77: 320-322.
- Samuel Chidi Ekpemo, Chukwuemeka Onyearugha (2019) Management Of Undescended Testis In Children In Aba Nigeria. International Journal of Clinical Urology 3: 15-17.
- David, Osifo Osarumwense; Iyekoretin, Evbuomwan (2008) Undescended Testes In A Developing Country-A Study Of The Management Of 71 Patients, African Journal of Paediatric Surgery 5: 11-14.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.