Treatment of Tibial Stress Fracture in Elite College Athlete using Teriparatide (Forteo)
by Patrick Laird*, Matthew Motisi, Drew Slater, James Ross
Broward Health Orthopedics, USA
*Corresponding author: Patrick Laird, Broward Health Orthopedics, 1600 S South Andrews, Ft Lauderdale FL 33316, USA
Received Date: 14 August, 2025
Accepted Date: 25 August, 2025
Published Date: 28 August, 2025
Citation: Laird P, Motisi M, Slater D, Ross J (2025) Treatment of Tibial Stress Fracture in Elite College Athlete using Teriparatide (Forteo). J Orthop Res Ther 10: 1398. https://doi.org/10.29011/2575-8241.001398
Abstract
An elite 21-year-old male college basketball player developed a Fredericson Grade 4A stress fracture to the right tibia. His symptoms did not improve despite rest and he was unable to participate in activity. The patient’s history, physical examination, and imaging, including right tibial radiographs and MRI, were indicative of a stress fracture to the tibial shaft. He was therefore recommended nonoperative management, consisting of a tall boot for two weeks, rest from activity for 4-6 weeks, and daily Teriparatide (Forteo) injections for two months. The athlete was able to return to the court after seven weeks of this non-operative treatment plan without physical limitations or pain, while logging the second highest total minutes played on the entire team following his return. This case report reviews the evaluation and treatment of stress fractures in athletes and the efficacy of using Teriparatide to expedite return to asymptomatic play.
Introduction
Stress fractures in athletes can be a very problematic diagnosis, with regards to treatment and timing of the return to play. Stress fractures can occur in several areas of the body, and often result from no obvious trauma. Patients will often note activity-related pain that consistently persists without alleviation of symptoms for several months. This can be frustrating not only for the athlete, but also the coaching staff, training staff, and the physicians alike. Stress fractures are the result of repetitive mechanical stresses in a particular area of the bone that causes microscopic fractures [1]. The initial diagnostic workup includes radiographs of the affected area and if necessary, an MRI is recommended for definitive diagnosis [2]. The well documented treatment for stress fractures in athletes is activity restriction with a period of protected weight bearing followed by a graduated return back to activities, over a period depending on the patient and physician’s recommendations [3].
Bone normally remodels through a balanced cycle of osteoclastic resorption and osteoblastic bone formation. A sudden increase in training volume of high-intensity, repetitive impact activities can cause an imbalance in bone remodeling if not allowed adequate time for recovery [4]. There has been recent evidence to suggest that parathyroid hormone (PTH) and its synthetic peptide fragment, teriparatide (PTH 1-34) may have a net anabolic effect on bone and may aid in fracture healing, specifically in fractures that are slow to heal [5]. Parathyroid hormone (PTH) is the primary regulator of calcium and phosphate metabolism in both the kidneys as well as bone [6]. Teriparatide (TPTD) is a recombinant form of the bioactive portion of parathyroid hormone (PTH 1, 34) that was initially approved by the FDA in 1987 for the treatment of patients with high risk of fracture including postmenopausal women with osteoporosis, men with primary or hypogonadal osteoporosis, and men and women with osteoporosis secondary to sustained glucocorticoid therapy [1]. The recommended dosage is 20 μg subcutaneously once daily, which has an anabolic effect on the bone, prompting new bone formation on cortical and trabecular bone by stimulating osteoblasts over osteoclasts [7]. In humans, this has demonstrated greater bone mass via the new formation of both cancellous and cortical bone.
The use of Teriparatide has been suggested off label to stimulate bony healing in not only delayed fracture unions and non-unions, but also in stress fractures in young adults [8]. However, there is limited literature that has investigated the effectiveness of Teriparatide for the treatment of stress fractures. Similarly, there is no established timetable in regard to effective return to sport after beginning teriparatide treatment. We present a case of a Division I basketball player that was treated with tetrapeptide and returned to sport pain-free and without limitations 7 weeks after initiating treatment. Additionally, we demonstrate the progressive healing on subsequent MRI studies.
Case Presentation
A 21-year-old collegiate male basketball player presented to the office with 1 month of right shin pain. He noted the pain predominantly while sprinting during basketball practice, which had worsened throughout the week prior to his visit. The athlete localized the pain to the anterior aspect of the right lower extremity, at the mid-tibial shaft. The patient denied any history of new activity, injury, or trauma. He also denied any pain while walking however endorsed pain while running. The patient had a remote history of a right knee hamstring strain. Regular home medications included weekly allergy injections.
Upon physical examination of the patient’s right lower extremity, there was tenderness to palpation over the medial and posterior mid tibial shaft. There was no knee joint line tenderness and the knee range of motion was full from 0 – 140 degrees. The patient’s knee examination was stable, with negative Lachman’s, dial, and posterior and anterior drawer exams, as well as a negative McMurray’s sign. He was neurovascularly intact with a 2+ dorsalis pedis and posterior tibial pulse; strength and muscle bulk were normal.
Anteroposterior (AP) and lateral radiographs were initially obtained which demonstrated cortical thickening of the anterior tibial cortex, without any evidence of a stress fracture line (Figure 1). An MRI of the right lower extremity without contrast thereafter obtained and demonstrated a Fredericson Grade 4A stress fracture of the tibia shaft, with periosteal and interosseous edema. There was also thickening of the tibial cortex, without intra-cortical signal change (Figure 2). After discussion of both nonoperative and operative treatment options with the patient, a collaborative decision was made to proceed with non-operative management. The patient was advised to wear a tall boot for two weeks following his visit, along with avoidance of physical activity. The patient was also started on daily teriparatide injections, with the plan for two months of medical treatment. After three weeks, the patient demonstrated significant improvement in his symptoms, describing no pain with daily activities and minimal tenderness to palpation along the tibia. A repeat MRI was obtained at that time, which demonstrated complete resolution of the periosteal edema, and improvement in the amount of intra-osseous edema (Figure 3). The walking boot was discontinued, and the athlete was allowed to perform exercise on a stationary bike and under-water treadmill. He was also allowed to begin shooting basketballs.
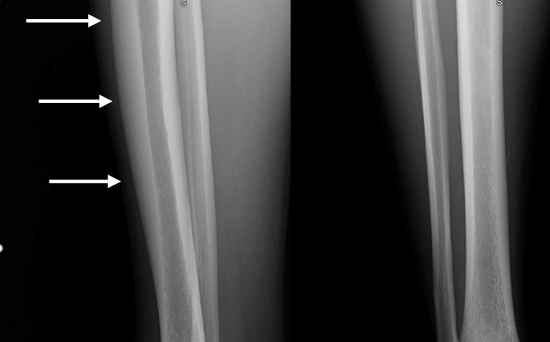
Figure 1: Lateral (A) and anteroposterior (B) radiographs demonstrate thickening of the anterior tibial cortex, without stress fracture line. (arrows)
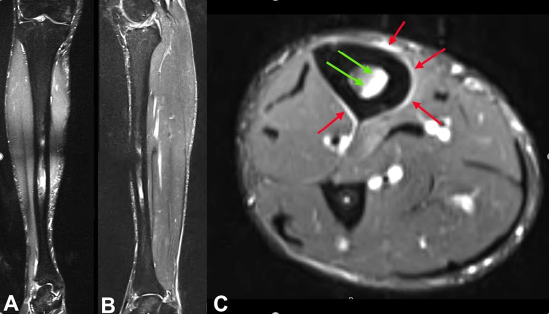
Figure 2: Initial MRI after presentation and prior to treatment. The sagittal (A), coronal (B), and axial (C) reformats demonstrated intra-osseous (green arrow) and periosteal (red arrow) edema, consistent with a Fredericson Grade 4A stress fracture of the tibia shaft.
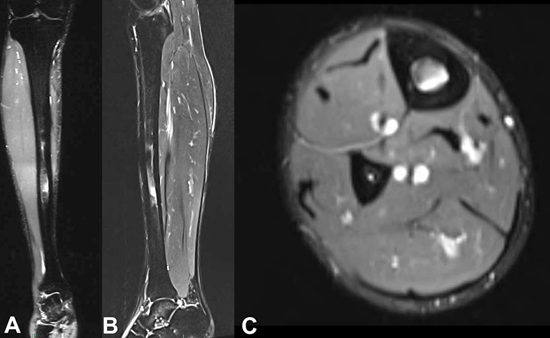
Figure 3: MRI that was obtained, 3 weeks after clinical treatment, demonstrating complete resolution of the periosteal edema and improvement in the intra-osseous edema, now consistent with Fredericson Grade 3 stress fracture.
After seven weeks of teriparatide injections and avoidance of basketball games, the patient noted no pain with activities and upon examination there was no tenderness to palpation along the tibial shaft. Another MRI was performed, which continued to demonstrate improvement in the intra-osseous edema (Figure 4). Given that he was asymptomatic, he was cleared to return to play, however continued with the teriparatide injections for a total of two months. Further serial MRIs were obtained at 10 weeks and 18 weeks from the initiation of treatment, which eventually demonstrated complete resolution of any bony edema (Figure 4). Throughout the season, he was able to play in 34 of the team’s 34 games, with the second most total minutes (1,043 minutes) played on the entire roster; he was able to average 30.7 minutes per game. He did not experience any return of symptoms or pain.
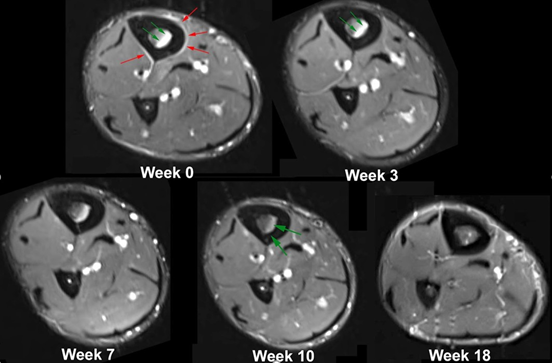
Figure 4: Serial MRI’s (axial) demonstrating progressing healing of the tibial stress fracture.
Discussion
Stress fractures in athletes can cause significant distress to the athlete, both by length of symptoms and time to diagnosis. Tibial stress fractures are relatively common and have been reported to have an incidence of 10% to 20% in runners [9]. Stress fractures tend to initially have subtle pain and can sometimes take weeks before a patient presents for evaluation, due to frustration with pain and limitation from normal activity [10]. These injuries can have a psychosocial effect on an athlete due to the loss of time from competition, and even an economic effect for professional athletes. For athletes and most patients, the time to recovery is a very important part of the decision algorithm [11]. In a systematic review of return to sport (RTS) with tibial stress fractures by Schundler, et al, 12% of athletes undergoing nonoperative management went on to requiring surgical intervention. The rate of failure for nonoperative management falls between 0-25% in this population [12]. These numbers do not necessarily even account for increased time to recovery and RTS without other nonoperative treatment modalities. The average return to play in both the nonoperative management groups and operative managements of the aforementioned systematic review was 3-4 months. This included 341 patients among all the studies reviewed in the article [13]. In a more specific study of a cohort of three Division 1 collegiate running athletes, the mean time to return to unrestricted sport participation was 12-13 weeks for all injury sites reported [14]. There were no significant differences in this time to return based on injury location, i.e., metatarsal versus tibia stress fractures.
Kahanov et al. demonstrated that the return to training of athletes who have sustained lower body stress fractures may take between 61 and 153 days, on average [15]. For these reasons, we believe exploring advantageous treatment options to help the athlete recover predictably and expeditiously is of paramount importance. Almirol, et al. demonstrated anabolic effects of teriparatide in a randomized controlled pilot study of premenopausal women, aged 21 to 45 years, with stress fractures. These anabolic effects were demonstrated by a significantly greater increase in bone biomarkers at eight weeks. Quantitative computed topography (CT) scans also demonstrated a larger cortical area and thickness in the patients treated with teriparatide. Using Fredericson grading of magnetic resonance imaging (MRI) to assess the healing of lower limb fractures, four women (67%) who received teriparatide for eight weeks, compared with three women (43%) in the placebo control group, achieved a two-grade or more improvement in healing or reduction to grade zero [8].
The treatment of a tibial stress fracture with Teriparatide in our athlete was proven to be efficacious in stimulating bony healing, as demonstrated clinically and upon serial MRIs. Secondarily, after daily treatment of teriparatide, in conjunction with the classical nonoperative management, the athlete was able to return to sport seven weeks after developing a Fredericson 4a tibial stress fracture. Therefore, in stress fracture injuries where conservative management does not timely alleviate the problem, other options that are less invasive than surgical management should be considered.
Teriparatide, however, does have side effects that must be considered when using for the treatment of young athletes with stress fractures. Some of the common adverse reactions to teriparatide include pain in limb (reported by ≥ 10% of patients), nausea, headache, and dizziness (each reported by ≥ 1% to < 10% of patients) [16]. Continuous use of TPTD can result in hyperparathyroidism which may cause bone resorption instead of bone formation, and therefore it is important to administer the medication as instructed. Most notably, TPTD has been shown to cause an increased incidence of osteosarcoma in rats treated with TPTD, although this effect has not been observed in humans in prior studies [1, 5]. For patients who begin with Teriparatide treatment, it is recommended to get baseline blood work which includes calcium, magnesium, sodium, potassium, creatinine, urea, and cholesterol. It is also recommended to have a serum calcium measurement at one month of treatment for all patients that begin teriparatide therapy. Follow-up intervals for calcium monitoring should then be decided by the prescribing physician at their discretion. If hypercalcemia is present after beginning therapy, the dose should be reduced. If the lab values do not return to baseline, then treatment should be administered every other day. If the hypercalcemia persists, therapy should be discontinued entirely, and further workup should be pursued to find the cause of the hypercalcemia [12]. A bone mineral density is also recommended for evaluation at one year after their first does. However, these recommendations are cited in the setting of treatment of osteoporosis with long standing TPTD therapy [12].
Conclusions
It is important to continue to evolve our treatment protocols and modalities for injuries, especially those that can have as large of an impact on the patient population, such as stress fractures in athletes can. While treatment with teriparatide has shown to be effective in the right patient, further studies could be considered to further evaluate the relationship of Teriparatide as a beneficial and efficacious adjunct treatment to facilitate recovery from stress fractures.
References
- FORTEO (teriparatide) Label (2020).
- Patel DS, Roth M, Kapil N (2011) Stress fractures: diagnosis, treatment, and prevention. Am Fam Physician 83(1): 39-46.
- Milgrom C, Giladi M, Stein M, Kashtan H, Margulies JY, et al. (1985) Stress fractures in military recruits. A prospective study showing an unusually high incidence. J Bone Joint Surg Br 67(5): 732–5.
- Hetland ML, Haarbo J, Christiansen C (1993) Low bone mass and high bone turnover in male long-distance runners. J Clin Endocrinol Metab 77(3): 770-775.
- Campbell JE, Campbell GM, Hanley DA (2014) The effect of parathyroid hormone and teriparatide on fracture healing. Expert Opin Biol Ther 15(1): 119-129.
- Khan M, Jose A, Sharma S (2022) Physiology, Parathyroid Hormone. Stat Pearls USA.
- Babu S, Sandiford NA, Vrahas M (2015) Use of Teriparatide to improve fracture healing: What is the evidence? World J Orthop 6: 457-461.
- Almirol EA, Chi LY, Khurana B, Hurwitz S, Bluman EM, et al. (2016) Short-term effects of teriparatide versus placebo on bone biomarkers, structure, and fracture healing in women with lower-extremity stress fractures: A pilot study. J Clin Transl Endocrinol 5: 7-14.
- Boden BP, Osbahr DC (2000) High-Risk Stress Fractures: Evaluation and Treatment. J Am Acad Orthop Surg 8(6): 344-353.
- May T, Marappa Ganeshan R. (2023) Stress Fractures. Stat Pearl, USA.
- Feldman JJ, Bowman EN, Phillips BB, Weinlein JC (2016) Tibial Stress Fractures in Athletes. Orthop Clin North Am 47(4): 733-741.
- Vall H, Patel P, Parmar M (2024) Teriparatide. StatPearls, USA.
- Schundler SF, Jackson GR, McCormick JR, Tuthill T, Lee JS, et al. (2023) Non-operative Management of Tibial Stress Fractures Result in Higher Return to Sport Rates Despite Increased Failure Versus Operative Management: A Systematic Review. Arthrosc Sports Med Rehabil 5(3): e881-e889.
- Miller TL, Jamieson M, Everson S, Siegel C (2018) Expected Time to Return to Athletic Participation After Stress Fracture in Division I Collegiate Athletes. Sports Health 10(4): 340-344.
- Kahanov L, Eberman LE, Games KE, Wasik M (2015) Diagnosis, treatment, and rehabilitation of stress fractures in the lower extremity in runners. Open Access J Sports Med 6:87-95.
- European Medicines Agency (2020) Terrosa summary of product characteristics.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.