Treatment of Imperforate Hymen with Diode Laser: A Case Report
by Antonio Maiorana1*, Raffaella Romano2, Martina Maiorana3, Antonella Mercurio1
1Obstetrics and Gynecology Unit, ARNAS Civico Di Cristina-Benfratelli Hospital, Palermo, Italy
2Department of Health Promotion, Mother and Child Care, Internal Medicine and Medical Specialties (PROMISE), University Of Palermo, Palermo, Italy
3Department of Human Pathology of Adult and Childhood “Gaetano Barresi”, Unit Of Pediatric Surgery, University Of Messina, Messina, Italy
*Corresponding author: Antonio Maiorana, Gynecology and Obstetrics Unit, ARNAS Civico Di Cristina-Benfratelli Hospital, Piazza Leotta n.4, Palermo, 90127, Italy
Received Date: 26 July 2025
Accepted Date: 30 July 2025
Published Date: 01 August 2025
Citation: Maiorana A, Romano R, Maiorana M, Mercurio A (2025). Treatment of Imperforate Hymen with Diode Laser: A case Report. Ann Case Report. 10: 2357. DOI:10.29011/2574-7754.102357
Abstract
Background: Imperforate hymen is a congenital anomaly characterized by the absence of an opening in the hymenal membrane, leading to obstructed menstrual flow and complications such as hematocolpos and hematometra. Standard surgical treatment involves hymenotomy with a scalpel or electrocautery, but this approach may be associated with bleeding, postoperative pain, and scarring, potentially impacting future sexual function. The diode laser has emerged as a promising alternative, offering improved precision, reduced bleeding, and better postoperative healing. Case Presentation: A 13-year-old girl presented with abdominal pain and urinary retention. Clinical examination and imaging confirmed an imperforate hymen with hematocolpos and hematometra. The patient underwent a cross-shaped hymenotomy using a diode laser, followed by hematocolpos drainage and vaginoscopy to rule out genital malformations. Postoperative recovery was uneventful, with minimal pain (VAS score: 1), negligible blood loss, and no significant discomfort. Follow-up evaluations at 7 days and 3 months revealed excellent healing, with no hymenal opening narrowing. Discussion: The diode laser provides several advantages over traditional techniques, including: high precision and controlled incision leading to a hymenal opening closely resembling physiological anatomy; minimal intraoperative bleeding due to the laser’s coagulating effect; reduced postoperative pain and lower risk of synechiae formation; improved healing with decreased likelihood of hymenal reclosure. This case represents the first documented use of a diode laser for imperforate hymen treatment in the scientific literature, highlighting its potential as a superior alternative to conventional hymenotomy. Conclusions: Diode laser hymenotomy appears to be a well-tolerated, minimally invasive approach with excellent functional and aesthetic outcomes. Wider adoption of this technique could provide valuable data to refine surgical guidelines and enhance patient care. However, further studies are needed to compare its long-term efficacy with traditional methods.
Keywords: Imperforate Hymen; Hematocolpos; Hymenal Membrane; Labia Majora: Haemostasis.
Introduction
Imperforate hymen is a congenital malformation characterized by the absence of an opening in the hymenal membrane, preventing normal menstrual blood flow. [1] The estimated incidence is about 1 in 2,000 female births. [2]
Symptoms usually appear during adolescence and include primary amenorrhea, cyclic pelvic pain, and, in some cases, urinary retention due to hematocolpos compressing the bladder [3]. The clinical consequence of an imperforate hymen is the development of hematocolpos, followed by hematometra, due to the inability of menstrual blood to flow out of the vagina. [4] The standard treatment for imperforate hymen is hymenotomy using a scalpel or electrocautery, followed by vaginal stent placement to prevent synechiae. Standard surgical treatment of imperforate hymen involves hymenectomy after a cruciate, plus, or X-shaped hymenotomy incision. [5] However, this technique may be associated with bleeding, postoperative pain, and scarring, which could affect future sexual function. [6] The diode laser has emerged as a promising alternative, offering potential advantages such as improved precision, reduced bleeding, and less postoperative discomfort. [7]
Case presentation
A 13-year- old young woman presented to the pediatrician ER because of abdominal pain and urinary retention. The patient denied episodes of vomiting of fever. Her medical history was unremarkable, with no known diseases or gynecological conditions. She reported she has not had menarche yet. During the investigations she performed a gynecological evaluation: abdomen globose, manageable, midly tender on deep palpation; external genitalia of nulliparous woman with normally shaped labia majora. An imperforate hymenal membrane was observed, with a swelling suggestive of hematocolpos (Figure 1)
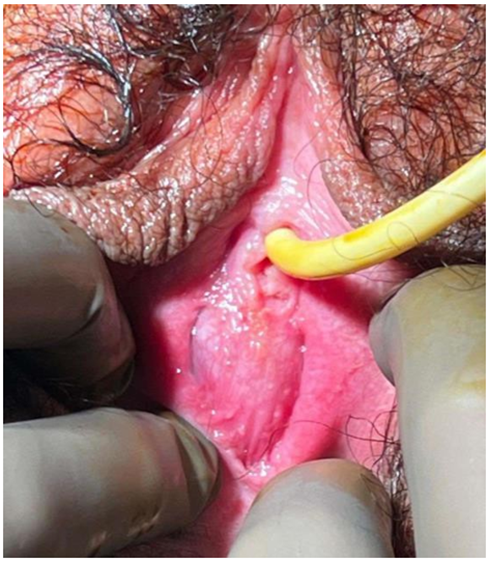
Figure 1
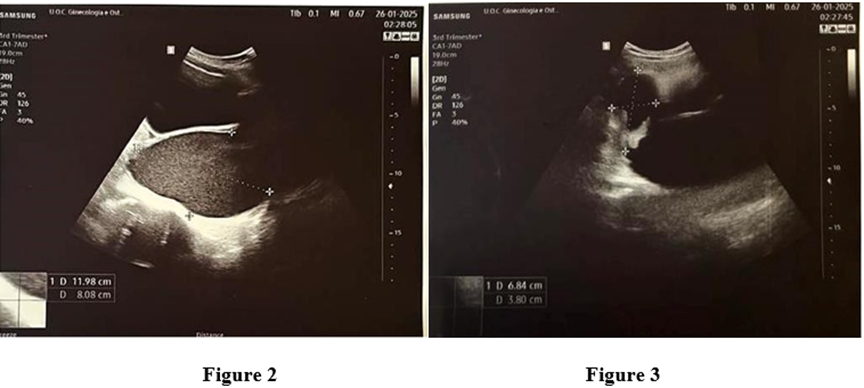
On transabdominal ultrasound examination: the bladder was full and overdistended, consistent with urinary retention. Behind to the bladder, a mass measuring 11x8x9 cm with corpuscolar content was observed, suggestive of hematocolpos (Figure 2). The aforementioned mass appeared contigous with the uterine cavity (68x38 mm), which was also distended by anechoic fluid, suggestive of hematometra (Figure 3). The left adnexa was normal. The right adnexa was not visible. The Douglas pouch was free of fluid. The kidneys were in their normal position and whitin normal limits, with mild pyelectasis.
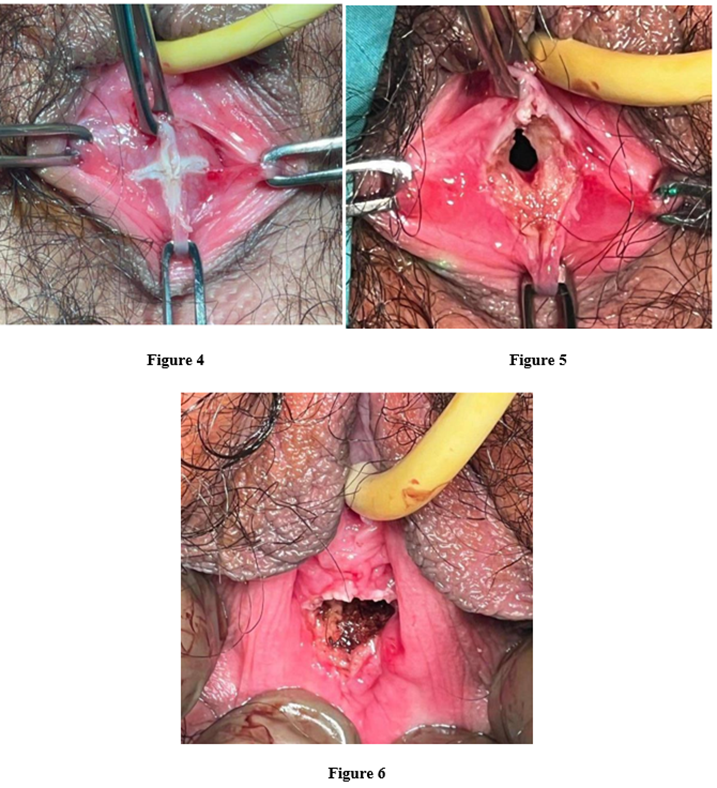
The patient was therefore admitted to the gynecology department, where she underwent the following procedure: cross shaped incision of the hymenal membrane using a diode laser, drainage of the hematocolpos, Subsequent vaginoscopy to rule out possible genital malformations (Figure 4,5,6).
Postoperatively, the patient reported a pain level of 1 on the VAS scale. Blood loss was minimal and postoperative discomfort was negligible. Two days after the procedure, the patient was discharged in good overall clinical condition (Figure 7,8).
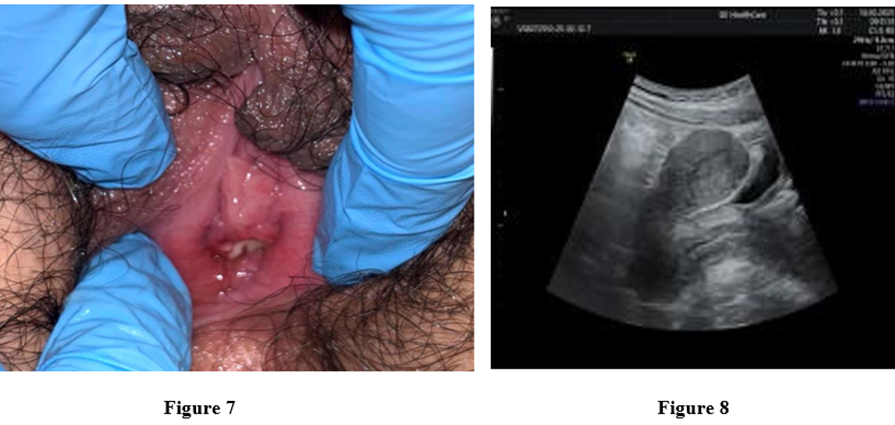
The patient was re-evalueted 7 days after the procedure and after the menstrual flow, where both the clinical and ultrasound findngs were normal. The patient was re-evaluated after three months, revealing an extremely precise incision with no signs of hymenal opening narrowing.
Discussion
The diode laser produces two wavelengths from 980 to 1470nm. These wavelengths cut and vaporize the tissue while simultaneously promoting absorption of haemoglobin and H2O resulting in excellent haemostasis, cutting and vaporization. This enables precise incision with superior hemostatic effects compared to traditional scalpels or electrocautery [8] Furthermore, the thermal penetration depth is significantly lower than with other lasers. This allows safe and more precise laser application in the vicinity of sensitive structures with simultaneous thermal protection of the surrounding tissue. [9]
In treating imperforate hymen, the diode laser is used to create a controlled opening in the hymen while minimizing thermal damage to surrounding tissues. The key aspects of this technique include
- Local anesthesia: In most cases, topical anesthetic cream or local infiltration is sufficient.
- Laser incision: The laser is applied along a predefined area, avoiding excessive tissue trauma.
- Minimal bleeding: Due to the laser is coagulating effect.
- Optimized healing: Reduced risk of postoperative synechiae.
The advantages of Diode Laser over traditional techniques are
- Reduced intraoperative bleeding: the photothermal effect of the diode laser enables immediate coagulation of blood vessels, reducing the risk of excessive bleeding compared to traditional scalpel techniques.
- Less postoperative: laser use reduces postoperative pain due to decreased inflammation and minimal collateral tissue damage.
- Lower risk of synechiae formation: the diode laser promotes more uniform healing of the vaginal mucosa, reducing the risk of adhesions or scarring that could impair future sexual function.
- Precision and controlled incision: unlike traditional scalpels, the laser allows more accurate control over incision depth and extension, leading to improved aesthetic and functional outcomes.
Advantages and Strengths
- High Precision of Laser Fiber: the precision of the laser fiber allows for the recreation of a hymenal opening very close to physiological anatomy, resulting in a hymen that appears compatible with that of a Virgin patient. This aspect is particularly significant from a psychological perspective for both the patient and her parents.
- Improved healing and reduced risk of reclosure: the enhanced healing process achieved with laser
- Treatment minimizes the risk of hymenal opening closure, ensuring a more stable and long-term outcome.
- Unique Case in Scientific Literature: This is the only documented case of an imperforate hymen treated with a diode laser in the scientific literature, highlighting its novelty and potential for future clinical applications.
Limitations and Clinical Considerations
Despite its numerous advantages, diode laser use has some limitations
Higher cost: The need for specialized equipment makes this technique more expensive than traditional hymenotomy.
Learning curve: Proper training is required to avoid complications from excessive tissue heating.
Limited availability: Not all medical centers have access to diode laser technology for this procedure.
Conclusions
The treatment of imperforate hymen with a diode laser is a promising alternative to conventional surgery, offering advantages in terms of precision, reduced bleeding, and improved healing. The laser treatment for hymenoplasty after a diagnosis of an imperforate hymen offers a well-tolerated, minimally invasive surgical approach with satisfactory functional and aesthetic outcomes. As this is the first case described in the literature, broader adoption of the technique is desirable to gather more data that are consistent. However, further studies are needed to establish definitive guidelines and compare this technique with traditional methods. The adoption of the diode laser could enhance surgical outcomes and improve patients’ quality of life, particularly in specialized centers with access to this technology.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed Consent: Written informed consent was obtained from the patient before the operation and the pubblication of this paper
References
- Abdelrahman HM, Jenkins SM, Feloney MP. (2023) Imperforate Hymen. StatPearls.
- Kumar Y, Yadav P, Agarwal A. (2022) Abdominal swelling and obstructive uropathy due to hematometrocolpos secondary to imperforate hymen: a case report. Pan Afr Med J. 41: 18.
- Chebil A, Bouchahda H, Nouiji S, Dahmeni H, Chaouch MA, et al. (2024) Abdominal distension resulting from hematocolpos in children: A case report. Int J Surg Case Rep. 124: 110414.
- Marino G, Alfieri N, Tessitore IV, Barba M, Manodoro S, et al. (2023) Hematocolpos due to imperforate hymen: a case report and literature systematic review. Int Urogynecol J. 34: 357-369.
- Basaran M, Usal D, Aydemir C. (2009) Hymen sparing surgery for imperforate hymen: case reports and review of literature. J Pediatr Adolesc Gynecol. 22: e61-e64.
- Meutia AP, Yonathan K, Hidayah GN, Moegni F. (2022) The Use of Interdigitating Y-Flap Technique for Imperforate Hymen. JPRAS Open. 32: 43-47.
- Vitale SG, Mikuš M, De Angelis MC, Carugno J, Riemma G et al. (2023) Diode laser use in hysteroscopic surgery: current status and future perspectives. Minim Invasive Ther Allied Technol. 32: 275-284.
- Nappi L, Pontis A, Sorrentino F, Greco P, Angioni S. (2016) Hysteroscopic metroplasty for the septate uterus with diode laser: a pilot study. Eur J Obstet Gynecol Reprod Biol. 206: 32-35.
- Spaich S, Berlit S, Berger L, Weiss C, Tuschy B, et al. (2023) First experiences with a diode laser in major gynecological laparoscopic procedures show lack of benefit and impaired feasibility. Lasers Med Sci. 38: 34.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.