Treatment of Chronic Achilles Tendon Injury Using Short Harvest Flexor Hallucis Tendon Transfer
by M Sethi*, M Salim, E Alderton, R Limaye
University Hospital of North Tees, Stockton, United Kingdom
*Corresponding author: Mohit Sethi, University Hospital of North Tees, Stockton, United Kingdom
Received Date: 24 September 2025
Accepted Date: 29 September 2025
Published Date: 01 October 2025
Citation: M Sethi, M Salim, E Alderton, R Limaye (2025) Treatment of Chronic Achilles Tendon Injury using Short Harvest Flexor Hallucis Tendon Transfer. J Surg 10: 11459 https://doi.org/10.29011/2575-9760.011459
Abstract
Background: The transfer of the Flexor Hallucis tendon is a recognized treatment for chronic injuries to the Achilles tendon, known to alleviate pain and enhance strength. This study aimed to evaluate the outcomes of utilizing a short harvest of the flexor hallucis longus tendon fixed with a bio-tenodesis screw in the management of chronic ruptures of the Achilles tendon.
Methods: A retrospective review was conducted involving 32 patients (n=32) who had both preoperative and postoperative American Orthopaedic Foot & Ankle Society (AOFAS) ankle-hindfoot scores, and who underwent treatment with a short harvest of the flexor hallucis longus tendon graft.
Results: An average follow-up duration of 31 months revealed an improvement in AOFAS scores. Statistical analysis was performed using the Wilcoxon Signed Ranked Test, with significant results (p<.001).
Conclusion: The transfer of the Flexor Hallucis longus tendon using a short graft and securing it with a bio-tenodesis screw for chronic Achilles tendon ruptures yields positive outcomes and may serve as a preferred treatment option for this condition.
Keywords: Aofas: American Orthopaedic Foot & Ankle Society Scores. Fdl: Flexor Digitorum Longus, Fhl: Flexor Hallucis Longus, Pb: Peroneus Brevis, Peek: Polyetheretherketone, Ta: Tendo Achilles.
Introduction
The Tendo-Achilles (TA) tendon is the largest, strongest, and thickest tendon in the human body [1]. Factors that increase the risk of its rupture include being middle-aged and male, engaging in sports (often referred to as “weekend warriors”), obesity, and the use of steroid injections and fluoroquinolone antibiotics [1]. Ruptures typically occur 2-6 cm above the TA insertion at the musculotendinous junction, a relatively avascular region [2].
Achilles tendon ruptures are the most frequently occurring tendon ruptures in the lower extremity [3]. Between 10-25 percent of acute ruptures go undiagnosed [4,5], leading to what is known as a neglected TA rupture. Contributing factors to this condition may include misdiagnosis or delays in diagnosis and treatment, as well as late patient presentation [6]. While there is no definitive timeline for when an acute rupture becomes a chronic or neglected rupture, a window of four to six weeks from injury to treatment is commonly accepted [3,7,8]. The management of neglected TA ruptures presents significant challenges for orthopedic surgeons [9-11]. While there is extensive literature regarding treatment for acute TA injuries, there is limited data on managing neglected ruptures. Although various treatment options have been proposed, a clear “gold standard” procedure remains undefined [3,7]. Some conservative approaches, such as using a molded ankle-foot orthosis, may be suitable for elderly, sedentary patients unfit for surgery [1,3]. Surgical reconstruction typically yields the best functional outcomes [3]. Defects in the TA that are less than 2 cm can often be repaired with an end-to-end technique, but chronic ruptures usually present with larger gaps upon clinical evaluation [12].
In 1931, Christensen first described using fascial turn-down flaps for the repair of neglected TA ruptures with gaps ranging from 2 to 10 cm [7,13]. While various modifications to this technique have been made, it has been noted that this method may result in a strength deficit of approximately twenty-three percent [3]. Later, in 1975, Abraham and Pankovich introduced the V-Y advancement flap as a treatment for neglected TA ruptures [14]. However, it has been suggested that this technique is more appropriate for younger patients. Inherently, the vascular supply of soleus helps the tendon heal faster in younger patients [7].
Material and Methods
A retrospective review was carried out on routinely collected data for chronic Achilles tendon rupture cases treated in the Department of Orthopaedics at North Tees and Hartlepool NHS Trust between January 2013 and January 2020. The inclusion and exclusion criteria are outlined in Table 1.
|
Inclusion Criteria |
Exclusion Criteria |
|
All patients had a documented history of Achilles tendon injury, with the time between rupture and surgical intervention exceeding six weeks. Clinically, they exhibited signs consistent with chronic rupture, such as a positive Thompson test or inability to perform a single heel rise. The diagnosis was confirmed through radiological imaging. Preoperative AOFAS scores were recorded, and all cases had a tendon gap greater than 5 cm. |
Open Achilles tendon rupture; The history of local infection near the Achilles tendon rupture. Concomitant diseases with fracture, blood vessels rupture, or nerve rupture. The patients who could not accept regular follow up or had no AOFAS score |
A total of 32 cases (n=32) met the inclusion criteria for this audit. All patients underwent pre-operative AOFAS scoring and were offered, and consented to, treatment involving Achilles Tendon (TA) reconstruction using a Flexor Hallucis Longus (FHL) tendon transfer. All surgeries were performed by the same senior surgeon using a standardized technique.Under general anaesthesia (Figure.1). patients were positioned prone with a tourniquet applied to the thigh. Following standard aseptic procedures, a posteromedial approach to the Achilles tendon was used. This method provides good access to the FHL tendon while avoiding injury to the sural nerve [5]. The paratenon was incised and fibrotic tissue debrided, revealing an average tendon gap of 5–8 cm. This gap was used to access the FHL muscle belly anteriorly.
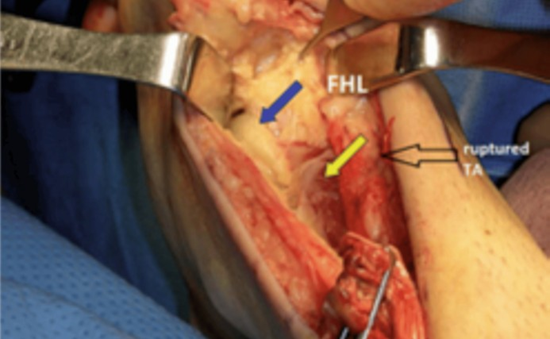
Figure 1: Exposure of Tendoachilles and Flexor Hallucis Longus
The FHL muscle was identified, and its tendon was traced distally. A 3 cm tendon segment was harvested using a short harvest technique from its insertion behind the ankle. Krackow stitches were applied to facilitate handling of the tendon, and preparation was done using the Arthrex FHL repair kit. The tendon’s width was measured, and a matching drill was used to create a tunnel in the calcaneus—just anterior to the original TA insertion—while avoiding the calcaneal tuberosity. The FHL tendon was inserted into the tunnel and secured using a PEEK interference screw, with the ankle positioned at approximately 60 degrees of plantar flexion.Proximally, a myoplasty was performed to attach the FHL muscle to the gastrocnemius. Closure involved suturing the deep fascia over the defect, followed by interrupted absorbable sutures for the subcutaneous tissue and interrupted nylon mattress sutures for the skin. Postoperatively, the affected limb was immobilized in a below-knee slab, and the patient was instructed to remain nonweight bearing for six weeks. At two weeks following surgery, a trained nurse performed a wound inspection and removed the sutures. Subsequent care involved applying serial casts, with a gradual decrease in plantarflexion of 20 degrees every two weeks. Physiotherapy was initiated at the six-week mark, along with full weight-bearing mobilization using an air cast boot. The boot was gradually discontinued over the next six weeks, during which more advanced physiotherapy exercises were introduced. For statistical evaluation, all patients were encouraged to participate in regular follow-up visits, which included physical examinations and MRI scans when necessary. Assessment of Achilles tendon function focused on tendon integrity, pain, ankle strength, and range of motion. Postoperative complications such as wound healing issues were also monitored. At the most recent follow-up, subjective outcomes were reassessed using the American Orthopaedic Foot & Ankle Society (AOFAS) ankle-hindfoot score (Appendix 1).
Results
A total of 32 patients (n = 32) were included in the study. Among them, 25 had experienced neglected acute Achilles tendon ruptures that were not treated promptly following the initial injury. The remaining 7 patients had sustained Achilles tendon ruptures despite receiving appropriate initial diagnosis and conservative management. The cohort comprised 23 males and 9 females, with a mean age of 50.3 years (range: 31–80 years) at the time of surgery. Thirteen patients had ruptures on the left side, while 19 had rightsided injuries. The mean duration between the rupture and surgical intervention was 14.87 weeks (range: 7–21 weeks). All patients completed follow-up. One patient developed a superficial wound infection that resolved with regular dressing changes and oral antibiotics. Another patient experienced reduced mobility due to a complication following total hip replacement. A third patient, who underwent cauda equina decompression, reported paresthesia in the leg, likely attributable to the spinal surgery. All other patients were able to perform a single-limb heel rise (Figure 2) and had returned to their pre-injury level of activity. Radiological assessments at the latest follow-up were satisfactory. The mean follow-up duration was 31 months (range: 13-68 months).
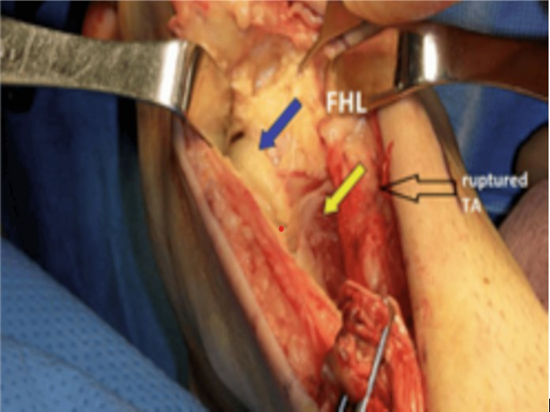
Figure 2: Dissection of FHL up to tunnel leading to Sustentaculum Tali.
Comparative analysis of preoperative and postoperative AOFAS (American Orthopaedic Foot & Ankle Society) ankle-hindfoot scores was conducted using paired-sample statistical testing via a commercial software package (IBM SPSS, version 26; Chicago, IL, USA). Due to non-normal data distribution, the non-parametric Wilcoxon signed-rank test was applied. Statistical significance was defined as p < 0.05. The median AOFAS score significantly improved from 49 preoperatively to 90 postoperatively (Table 2). The Wilcoxon signed-rank test confirmed this improvement was statistically significant (T = 528, Z = 4.94, p < .001) (Tables 3 and 4) (Figures 3-5).
|
N |
Mean |
STD Deviation |
Minimum |
Maximum |
|
|
AOFAS Pre-op |
32 |
48.91 |
8.283 |
34 |
68 |
|
AOFAS Pre-op |
32 |
89.28 |
9.169 |
63 |
100 |
Table 2: Descriptive Statistics.
|
N |
Mean Rank |
Sum of Ranks |
|
|
Negative Ranks |
0a |
0 |
0 |
|
Positive Ranks |
32b |
16.5 |
528 |
|
Ties |
0c |
||
|
Total |
32 |
Table 3: Wilcoxn Signed Ranked Test (AOFAS Post op- AOFAS Preop); a. AOFAS Postop < AOFAS Preop b. AOFAS Postop > AOFAS Preop; c. AOFAS Postop = AOFAS Preop.
|
Z |
-4.939b |
|
Asymp.Sig.(2 tailed) |
0 |
Table 4: Test Statistics (AOFAS Postop- AOFAS Preop); Test Statisticsa; a. Wilcoxon Signrd Ranked Test; b. Based on Negative Rank.
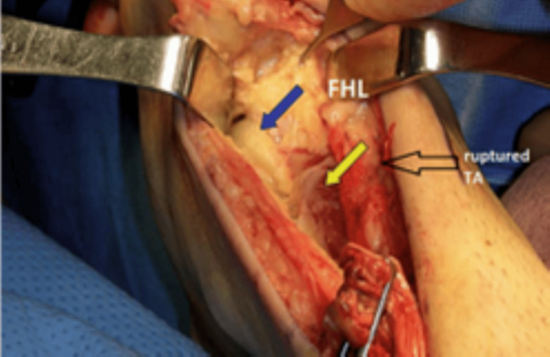
Figure 3: Preparation of Drill hole tunnel in calcaneum.

Figure 4: Insertion of FHL into the tunnel and bio composite screw.

Figure 5: Showing patient performing a single heel rise on the affected side at 12 months post op.
Discussion
Flexor Hallucis Longus (FHL) tendon transfer was first introduced approximately two decades ago as a surgical option for managing chronic Achilles tendon ruptures [16]. The FHL muscle generates sufficient power to elevate the heel and functionally compensate for the Achilles tendon. This tendon transfer technique offers several advantages in reconstruction of chronic Achilles ruptures: (1) anatomical proximity to the Achilles tendon, (2) similar function to the triceps surae, (3) adequate muscular strength, and (4) alignment with the Achilles tendon’s axis of motion [16]. Due to these favourable anatomical and biomechanical characteristics, FHL transfer has gained popularity among orthopedic surgeons, with numerous reports documenting successful outcomes [17]. The typical procedure involves harvesting the FHL tendon and anchoring it into a bone tunnel within the posterior calcaneus. Two harvesting approaches exist: a longer harvest from the midfoot at the knot of Henry, and a shorter harvest just posterior to the ankle. In our study, all patients underwent the short harvest technique. Yeoman et al. (2012) treated 11 patients with chronic Achilles ruptures using the short FHL harvest and interference screw fixation, achieving consistent outcomes and low complication rates. Our study, which included a larger cohort (n = 32), employed a similar harvesting technique combined with fixation using a biocompatible screw. Our results were comparable, demonstrating low complication rates and favorable functional outcomes. In all cases, FHL fixation was achieved using a PEEK Bio-Tenodesis screw system (Arthrex). This technique facilitates tendon fixation without the need for transosseous tunnel drilling or tensioning, streamlining the procedure. The effectiveness of this approach is supported by Benca et al. (2018), who showed in a cadaveric study of 24 paired lower legs that tenodesis screw fixation provided similar biomechanical properties and initial fixation strength compared to traditional transosseous suture techniques. Oksanen et al. (2014) reported that FHL muscle hypertrophy, averaging 52%, was observed via MRI following transfer. A similar observation was noted in one of our patients, where significant hypertrophy necessitated partial shaving of the muscle (Figure 1), further suggesting the FHL’s robust adaptive capacity. Previous work by Coull et al. (2003) indicated that while interphalangeal joint motion may be compromised post-transfer, functional tasks such as walking, running, and stair climbing remain unaffected. Nevertheless, the technique may lead to some loss of great toe function, which should be considered when treating younger, more active patients. In our series, the mean patient age was 50.3 years, placing them in the middle-aged category. Except for two patients—one with limited mobility due to a total hip replacement and another with residual symptoms related to spine surgery— all others returned to their pre-injury activity levels without difficulty in ambulation. MRI proved to be a valuable diagnostic modality in our study. It allowed accurate assessment of tendon stump integrity and healing status. No patient in our cohort was misdiagnosed using MRI, underscoring its reliability in evaluating chronic Achilles tendon injuries. This study has several limitations. It is retrospective in design, conducted at a single center, and performed by a single surgeon. Additionally, objective functional measures such as isokinetic strength testing or gait analysis were not included. There was also no comparative group using alternate surgical techniques. Future multicenter, randomized controlled trials with larger sample sizes and longer follow-up periods would help strengthen the evidence base.
Conclusion
FHL tendon transfer to the calcaneus, fixed using a bio-tenodesis screw, offers precise tensioning and secure fixation in the treatment of chronic Achilles tendon ruptures. The procedure demonstrated low morbidity and favorable functional outcomes. Most patients successfully resumed daily work and activity with minimal limitations, supporting its role as a preferred treatment strategy for this condition.
References
- V-Y Advancement and FHL Transfer for the Chronic or Neglected Achilles Tendon Rupture - Raikin.OrthopaedicsOne Articles. In: OrthopaedicsOne - The Orthopaedic Knowledge Network. Created May 16, 2011 05: 57. Last modified Jul 25. 201204, 19:11.
- Schweitzer. M E, Karasick D (2000) “MR: Imaging of Disorders of the Achilles Tendon.”American Journal of Roentgenology, 175: 613-625.
- Jake L, John MS (2012) “Surgical Treatment of the Neglected Achilles Tendon Rupture.”Achilles Tendon.
- Wegrzyn J, Luciani FJ, Philippot R, Brunet-Guedj E, Moyen B, et.al (2009) Chronic Achilles Tendon Rupture Reconstruction Using a Modified Flexor Hallucis Longus Transfer. International Orthopaedics,1187-1192.
- Bevilacqua, Nicholas J (2012) Treatment of the Neglected Achilles Tendon Rupture. Clinics in Podiatric Medicine and Surgery, 29: 291- 299
- Taylor, Robert: Neglected Achilles Tendon Ruptures: Surgical Considerations.
- Lin, Liu and Yin (2016) “Surgical Strategy for the Chronic Achilles Tendon Rupture.” BioMed Research International, 2016 : 1-8.
- Yong-Serk P, Sung KS (2012) Surgical Reconstruction of Chronic Achilles Tendon Ruptures Using Various Methods. Orthopedics.35: e2013-2018
- Cetti R, MD, Christensen SE, Jorgensen (1993) “Operative versus Nonoperative Treatment of Achilles Tendon Rupture.”The American Journal of Sports Medicine, 21: 791-799.
- Mcclelland D, Maffulli N (2004) Neglected Rupture of the Achilles Tendon: Reconstruction with Peroneus Brevis Tendon Transfer.. The Surgeon, 2: 209-213.
- Kursat DT: “The Effect of Phospholipids (Surfactant) on Adhesion and Biomechanical Properties of Tendon: A Rat Achilles Tendon Repair Model.” BioMed Research International, vol. 2015, 2015:1-6.
- Myerson MS: Disorders of the Achilles Tendon.. Reconstructive Foot and Ankle Surgery. 2010:341-357.10.1016/b978-1-4377-0923- 0.10027
- Christensen I (1953) Rupture of the Achilles Tendon; Analysis of 57 Cases.. Acta Chirurgica Scandinavica, 106: 50-60.
- Abraham E, AM Pankovich (1975) “Neglected Rupture of the Achilles Tendon. Treatment by V- Y Tendinous Flap.” The. Journal of Bone & Joint Surgery, 57: 253-255.
- Lepow GM, Green JB (2006) “Reconstruction of a Neglected Achilles The. The. Journal of Foot and Ankle Surgery, 45: 351-355.
- Shino K (1998) Maturation of Allograft Tendons Transplanted into the Knee: an Arthroscopic and Histological Study.. Journal of Bone and Joint Surgery, 70: 556-560.
- Arnoczky S P (1986) “Replacement of the Anterior Cruciate Ligament Tendon Rupture With an Achilles Tendon Allograft: A Case Report.” Using a Patellar Tendon Allograft. An Experimental Study.” Journal of Bone & Joint Surgery, 68: 376-385.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.