Translating Clinical Practice Guidelines into Stepped Care Treatment Recommendations for Osteoarthritis in the Assessment of Burden of Chronic Conditions (ABCC-) tool: A Mixed Qualitative Method Study
by VHJ Debie1; AHM Gidding-Slok1, LCM van Loon1, SAH Hendrix1, OCP van Schayck1, TAEJ Boymans2, RPG Ottenheijm1
1Department of Family Medicine, Maastricht University, The Netherlands.
2Department of Orthopedic Surgery, Maastricht University Medical Center, The Netherlands.
*Corresponding author: Valerie Debie, Department of Family Medicine, Care and Public Health Research Institute (CAPHRI), Maastricht University, P.O Box 616, 6200 MD, Maastricht, The Netherlands
Received Date: 26 August, 2025
Accepted Date: 04 September, 2025
Published Date: 07 September, 2025
Citation: Debie VHJ, Gidding-Slok AHM, van Loon LCM, Hendrix SAH, van Schayck OCP (2025) Translating Clinical Practice Guidelines into Stepped Care Treatment Recommendations for Osteoarthritis in the Assessment of Burden of Chronic Conditions (ABCC-) tool: A Mixed Qualitative Method Study. J Orthop Res Ther 10: 1400. https://doi.org/10.29011/2575-8241.001400
Abstract
Background: Many evidence-based clinical practices guidelines are available for osteoarthritis (OA). However, to be effectively implemented in clinical practice, these guidelines should be translated into concrete personalized, stepped care treatment recommendations. This study aims to develop treatment recommendations for OA using the Assessment of Burden of Chronic Conditions (ABCC-) tool, which quantifies and visualizes the burden of OA across physical, emotional, and social domains. The ABCC-tool includes personalized treatment recommendations to aid self-management, shared decision-making, and personalized care plans. The OA module, developed with input from healthcare professionals and patients, addresses pain, activity avoidance, and joint stiffness. Methods: A mixed qualitative methods study was conducted. First, a literature review was performed to identify current evidence-based treatment recommendations of the hip, knee, hand and wrist, and foot and ankle OA across the settings of general practice, physical therapy, orthopedic surgery, and rheumatology. Next, a consensus meeting was held with general practitioners specialized in musculoskeletal disorders to formulate stepped care evidence-based treatment recommendations for integration in the ABCC-tool. Results: Treatment recommendations for pain and joint stiffness were similar, focusing on lifestyle modifications and patient education, pain medication, corticosteroid injections and referrals to specialists. For activity avoidance, treatment recommendations emphasized patient education and specialist referrals. Conclusion: These treatment recommendations, integrated into the ABCC-tool, provide a stepped care, patient-centered framework for OA management, ensuring that guidelines can be applied to the individual needs of the patient. Future research should focus on pilot testing and implementing the ABCC-tool in clinical practice.
Keywords: ABCC-tool, Osteoarthritis, Clinical practice guidelines, Treatment recommendations, Stepped care, Personalized-care
List of Abbreviations: ABCC-tool: Assessment of Burden of Chronic Conditions Tool; COPD: Chronic Obstructive Pulmonary Disease; EULAR: European Alliance of Associations for Rheumatology; GP: General Practitioner; IA: Intra-Articular; MSK: Musculoskeletal; NICE: National Institute for Health and Care Excellence
NSAID: Non-Steroidal Anti-Inflammatory Drugs; OA: Osteoarthritis; OARSI: Osteoarthritis Research Society International; PROM: Patient Reported Outcome Measures; PRP: Platelet Rich Plasma; RCT: Randomized Controlled Trial; SNRI’s: Serotonin and Norepinephrine Reuptake Inhibitors
Introduction
A wide range of evidence-based clinical practice guidelines exist for osteoarthritis (OA), developed independently by various OA-related disciplines. These guidelines may be joint-specific or address OA more generally and most are developed separately across different countries [1-3]. Evidence-based guidelines are valuable tools for providing effective and efficient care, however they are often difficult to translate into treatment recommendations for routine clinical practice [4]. Typically, these guidelines are based on a standard patient profile, but many patients present with comorbidities. These patients often require more complex care than is provided in the original evidence used for the guidelines [4]. A more individualized approach is preferred, and guidelines should not be applied as ‘cookbook medicine [5]. Other challenges arise during the implementation phase, as patient preferences are often insufficiently considered in the guideline development process [4]. Furthermore, guidelines are mostly focused on biomedical symptoms, leaving out psychosocial burden [6]. Effective OA care should be tailored to the individual, ideally following a stepped care approach that adjusts treatment intensity based on the patient's needs and response to earlier steps.
To facilitate this personalized stepped care approach, the Assessment of Burden of Chronic Conditions (ABCC-) tool is expanded and validated for OA [7,8]. The ABCC-tool quantifies and visualizes the full scope of experienced burden of one or more chronic conditions, which can initiate the conversation between the patient and healthcare professional and includes practical treatment recommendations. Furthermore, this tool facilitates self-management, shared decision making, and personalized care plans, that include the chosen treatment [9]. Other chronic conditions in the ABCC-tool are asthma, chronic obstructive pulmonary disease (COPD), diabetes mellitus type 2, chronic heart failure, and post-COVID, and can be used together in any combination [9-14]. The ABCC-tool is explained in detail in Box 1.
The ABCC-tool consists of a five-step cycle. First, patients complete a self-administered questionnaire on physical, emotional and social burden. This questionnaire features a modular structure, consisting of a core set of generic questions applicable to all chronic conditions, with condition-specific modules added as needed. This enables a personalized patient reported outcome measure (PROM) tailored to individual patients. Second, results are visualized in a balloon diagram, where red (low) to green (high) balloons indicate the level of disease burden. Third, this balloon diagram can be used to select relevant topics for the patient to discuss the preferences of the patient, based on the colors and height of the balloon. Fourth, healthcare professionals can click on balloons and tailored treatment recommendations pop up, forming the basis to create personalized goals and a personalized care plan (see Figure 1). Finally, during follow-up, previous results (grey) and current results (colored) allow progress monitoring [10].
Box 1: ABCC-tool.
The OA module in the ABCC-tool consists of three domains: pain, activity avoidance and joint stiffness, and is aimed at hip, knee, hand, wrist, foot and ankle OA. The next step before implementation is to develop corresponding treatment recommendations for each domain, to be discussed during step 4 in the abovementioned cycle. Therefore, this study aims to translate evidence-based clinical practice guidelines into stepped care practical treatment recommendations to be integrated in the ABCC-tool.
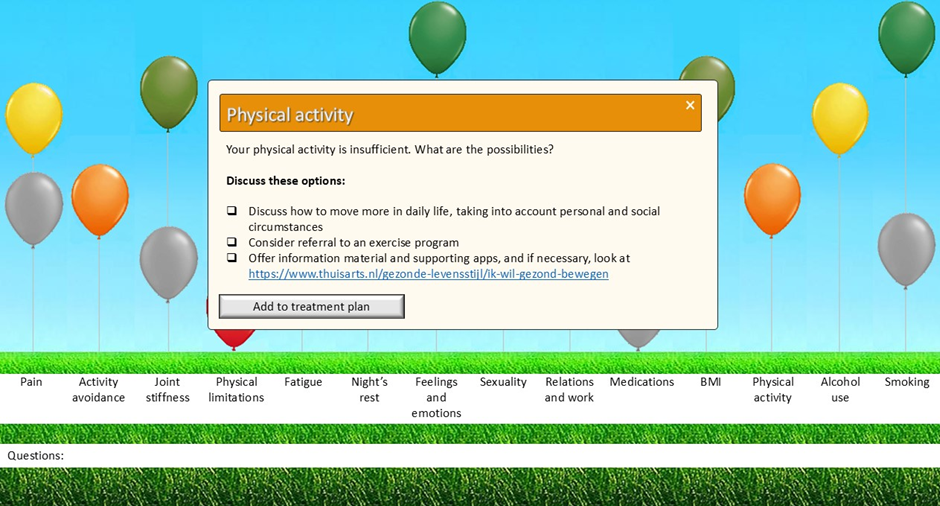
Figure 1: The balloon diagram in the ABCC tool for OA, showing the treatment recommendation for the "Physical Activity" domain, based on the height of the balloon. This domain is part of the lifestyle module, for which treatment recommendations were developed in a previous study (7). The recommendation appears when the healthcare professional clicks on the corresponding balloon.
Methods
A mixed qualitative study design was carried out, combining a literature review and a consensus meeting to identify evidence-based conversative treatment recommendations for hip, knee, hand, wrist, foot and ankle OA across the three domains of ABCC-tool’s OA module: pain, activity avoidance and joint stiffness. These recommendations were derived from clinical guidelines across the settings of general practice, physical therapy, orthopedic surgery and rheumatology, chosen because they represent the core settings involved in managing OA.
Literature Review
We followed a stepwise process to extract OA treatment recommendations for the ABCC-tool. First, we reviewed joint specific, evidence-based guidelines from Australia, Canada, the Netherlands, the United Kingdom, the United States, and other internationally recognized leading guidelines, across general practice, physical therapy, orthopedic surgery, and rheumatology. These were all developed from international literature and endorsed by scientific associations.
When no guidelines could be included, we searched PubMed and Embase for systematic reviews published after the year 2000 that offered joint specific treatment recommendations for at least one domain in the ABCC-tool. Only English and Dutch reviews were included. The full search strings are presented in Appendix 1. Additionally, an expert in musculoskeletal (MSK) disorders (RO) was consulted to ensure comprehensive coverage of the literature and to identify any additional treatment recommendations that may not have emerged from the systematic review.
Consensus Meeting
Based the literature review, the research team formulated a stepped care treatment concept for all included joints, aligned with the color-code balloons of the ABCC-tool. The cut-off points for the balloon colors in the ABCC-tool are determined based on the severity of the burden. Each question within the tool is scored on a scale from 0 (no burden) to 6 (severe burden). For all OA domains, scores of 0 correspond to a green balloon, 1–2 to orange, 3 to yellow, and 4–6 to red.
Through the Dutch College of General Practitioners expert group of general practitioners (GPs) specialized in MSK disorders, all their specialized GPs (n=70) were invited to participate in a questionnaire study and consensus meeting to establish consensus on the treatment recommendations for OA. The aim was to include at least six to twelve specialized GPs in the consensus meeting [15].
Ahead of the meeting, a draft set of recommendations was sent via an online questionnaire. GPs rated each on a 10-point Likert scale (0 = complete disagreement, 10 = complete agreement) and could provide feedback. Mean scores were calculated, and feedback was incorporated.
Before the consensus meeting, all mean scores were calculated, and additional feedback was processed. During the online meeting, only recommendations with a mean score below 7.5 were discussed [16]. The chair proposed revisions, which were re-rated by the GPs. This process was repeated until consensus was reached on all recommendations.
Results
Literature Review
The literature review and consensus meeting addressing the domains pain and activity avoidance were conducted between September and November 2022, while those focusing on the domain joint stiffness were held between October 2024 and January 2025, due to the addition of this OA domain following the validation process [8]. Because of this extended time between the two reviews, an additional literature review was conducted in May 2025 on pain and avoiding activities to ensure the latest versions of all guidelines were reviewed. A total of 26 guidelines were included in this study, see Table 1.
|
General practice |
Physical therapy |
Orthopedic surgery |
Rheumatology |
|
|
Australia |
Royal Australian college of General Practitioners [2] |
Australian Physiotherapy Association [17] |
Australian orthopedic association [18] |
Australian Rheumatology Association [19] |
|
Canada |
The College of Family Physicians of Canada [20] |
Arthroscopy Association of Canada [21] |
||
|
The Netherlands |
Dutch College of General Practitioners [22-24] |
Royal Dutch Society for Physical Therapy [23,25] |
Dutch Orthopedic Association [23,26-28] |
Dutch Association for Rheumatology [29] |
|
United Kingdom |
British Orthopedic Association [30] |
|||
|
United States |
American Physical Therapy Association [31,32] |
American Academy of Orthopedic Surgeons [3,33-36] |
American College of Rheumatology [37,38] |
|
|
International guidelines |
Osteoarthritis research society international [39] |
European Alliance of Associations for Rheumatology [40] |
Table 1: Included guidelines per country and discipline.
Domain Pain
For the domain pain, a total of 12 guidelines on hip OA were included [2,17,19,20,26,28,31,33,34,37,39,41], 16 for knee OA [2,17-23,25,26,30,32,35,37,39,41], eight for hand and wrist OA [20,24,29,36-40], and one for foot and ankle OA [3]. Treatment recommendations were mainly based on activation of self-management skills. Furthermore, it was advised to focus on education and lifestyle; physical-, occupational- and hand therapy; using braces, orthosis, and splints; prescribing non-steroidal anti-inflammatory drugs (NSAIDs) and weak opioids (e.g. tramadol); providing intra-articular corticosteroid injections; and refer to a specialist. See Table 2 for the recommendations per guideline used, with the specific joints specified.
|
|
General practice |
Orthopedic surgery |
Rheumatology |
||||||||||||||
|
Royal Australian college of General Practitioners [2] |
The College of Family Physicians of Canada [20] |
Dutch College of General Practitioners [22-24] |
Australian Physical therapy Association [17] |
American Physical Therapy Association [31,32] |
Royal Dutch Society for Physical Therapy [23,25] |
Australian orthopedic association [18] |
Arthroscopy Association of Canada [21] |
Dutch Orthopedic Association [23,26,28] |
British Orthopedic Association [30] |
American Academy of Orthopedic Surgeons [3,33-36] |
Osteoarthritis research society international [39] |
Australian Rheumatology Association [19] |
American College of Rheumatology [37,38] |
Dutch Association for Rheumatology [29] |
European Alliance of Associations for Rheumatology [40,41] |
||
|
Self-management and education |
2 |
1,2,3 |
2,3 |
1,2 |
1,2 |
1,2 |
2 |
2 |
1,2 |
1,2,3 |
3 |
||||||
|
Lifestyle |
1 |
1,2 |
2 |
1,2 |
1 |
2 |
1 |
2 |
1,2,4 |
1,2 |
1,2 |
||||||
|
Brace, orthosis, splint |
1,2,3 |
2,3 |
2 |
2 |
2 |
2 |
3,4 |
1,2 |
1,2 |
3 |
3 |
||||||
|
Walking aid |
1,2 |
1,2 |
1,2 |
1 |
1,2 |
||||||||||||
|
Thermal therapy |
1,2,3 |
1,2 |
1,2 |
2 |
2 |
3 |
2 |
||||||||||
|
Exercise program |
1,2 |
3 |
2 |
1,2 |
1,2 |
2 |
1,2 |
2 |
2 |
2 |
1,2 |
1,2,3 |
3 |
1,2,3 |
|||
|
Physical therapy |
1,2 |
1,2 |
2 |
1,2 |
1,2 |
1,2 |
2 |
1,2 |
2 |
1,2,4 |
|||||||
|
Occupational therapy |
1,2 |
||||||||||||||||
|
Hand therapy |
3 |
3 |
|||||||||||||||
|
Paracetamol |
2 |
2,3 |
1,2 |
1,2 |
2 |
1,2 |
|||||||||||
|
NSAID (oral) |
2 |
1,2,3 |
2 |
1,2 |
2 |
2 |
1,2 |
2 |
1,2,3,4 |
2 |
1,2,3 |
3 |
3 |
||||
|
NSAID (topical) |
2 |
2,3 |
2,3 |
1,2 |
1,2 |
1,2 |
2 |
2 |
2 |
2, 3 |
3 |
3 |
|||||
|
Weak opioid |
2 |
1,2,3 |
2 |
1,2 |
1,2 |
1,2 |
3 |
||||||||||
|
IA corticosteroid injections |
1,2 |
1,2 |
2,3 |
1,2 |
2 |
2 |
1,2 |
2 |
1,2,3,4 |
2 |
1,2,3 |
3 |
3 |
||||
|
Referral to (another) specialist |
2 |
2,3 |
1,2 |
1,2 |
2 |
1,2 |
2 |
1,2,3,4 |
1,2 |
3 |
3 |
||||||
|
1= hip OA; 2= knee OA; 3= hand and wrist OA; 4= foot and ankle OA |
|||||||||||||||||
|
NSAID= non-steroidal anti-inflammatory drugs; IA= intra-articular |
|||||||||||||||||
Table 2: Treatment recommendations from national and international guidelines for pain in hip, knee, hand, wrist, foot and ankle OA.
For all joints, at least one guideline emerged, and therefore, no literature review was done. In addition, the expert recommended two randomized controlled trials (RCT’s) on intramuscular corticosteroid injections for hip and knee OA [42,43].
Domain Activity avoidance
Two guidelines were found for activity avoidance for patients with hip and knee OA [25,26], which is presented in Table 3.
|
Physical therapy |
Orthopedic surgery |
|
|
Royal Dutch Society for Physical Therapy [25] |
Dutch Orthopedic Association [26] |
|
|
Self-management and education |
1,2 |
|
|
Training of pain coping skills |
1,2 |
|
|
Exercise program |
1,2 |
1,2 |
|
Physical therapy |
1,2 |
|
|
Referral to therapist |
1,2 |
|
|
1= hip OA; 2= knee OA |
Table 3: Treatment recommendations from a Dutch guideline for activity avoidance in hip and knee OA.
A search in PubMed and Embase was conducted because no guidelines were available for hand, wrist, foot and ankle OA on activity avoidance. This resulted in 18 unique articles. However, no articles were eligible for this study after reading the full text (see Figure 1 in Appendix 2). The consulted expert suggested as treatment recommendations that patients can be referred to a physical therapist and mental health practice nurse. Additionally, the expert also recommended a Dutch article that described the avoidance model on patients with OA in general, which focused on education and a referral to a physical therapist and psychologist [44].
Domain Joint stiffness
For the domain addressing joint stiffness of the hip, three guidelines were included [25,26,31], four for knee stiffness [22,25,26,35], two for hand and wrist stiffness [24,30], and none for stiffness in the foot or ankle. These guidelines recommend the support of self-management, education and lifestyle. Furthermore, braces and splints; an exercise program and physical therapy; NSAIDs; intra-articular corticosteroid-, and PRP-injections; and referring the patient to a specialist as well. Recommendations per guideline with the specific joints specified are presented in table 4.
|
General practice |
Physical therapy |
Orthopedic surgery |
||||
|
Dutch College of General Practitioners [22,24] |
Royal Dutch Society for Physical Therapy [25] |
American Physical Therapy Association [31] |
Dutch Orthopedic Association [26] |
British Orthopedic Association [30] |
American Academy of Orthopedic Surgeons [35] |
|
|
Self-management and education |
3 |
2 |
||||
|
Lifestyle |
1 |
2 |
||||
|
Brace, orthosis |
3 |
|||||
|
Exercise program |
2 |
1,2 |
1 |
1,2 |
3 |
2 |
|
Physical therapy |
2 |
1 |
2 |
|||
|
NSAID (unspecified) |
1,2 |
2 |
||||
|
IA corticosteroid injections |
2 |
|||||
|
Referral to (another) specialist |
2 |
|||||
|
1= hip OA; 2= knee OA; 3= hand and wrist OA |
||||||
|
NSAID= non-steroidal anti-inflammatory drugs; IA= intra-articular |
||||||
Table 4: Treatment recommendations from national and international guidelines for stiffness in hip, knee, hand and wrist OA
No specific guidelines addressing foot and ankle stiffness emerged during the search, so a literature review was conducted (see Figure 2 in Appendix 2). One systematic review was retrieved focusing on intra-articular injections to reduce joint stiffness [45].
Consensus Meeting
For the domains pain and activity avoidance, 17 treatment recommendations were formulated and sent to 70 specialized GPs in an online questionnaire. A total of 15 GPs completed the questionnaire. For 12 recommendations, consensus was reached (range mean consensus 7.5 to 9.0), while for the other five recommendations no consensus was reached (range mean consensus 5.1 to 7.2). Twelve out of 15 GPs participated in the consensus meeting. The five recommendations that initially lacked consensus were discussed after which the recommendations were revised to reach consensus on all recommendations.
For the domain joint stiffness, five GPs participated in the consensus meeting. Considering the significant overlap between the treatment recommendations for pain and joint stiffness, it was deemed unnecessary to conduct a separate scoring process for these recommendations. Instead, the beforementioned GPs were consulted to assess whether they agreed to adopt the same treatment recommendations established for pain in the context of joint stiffness, which they did.
See Appendix 3 for all treatment recommendations and adjustments with scores before and after the consensus meeting, and Appendix 4 for the final treatment recommendations included in the ABCC-tool for the domains pain, activity avoidance and joint stiffness.
Discussion
After a literature review, a questionnaire study and a consensus meeting, evidence-based stepped care conservative treatment recommendations for hip, knee, hand, wrist, foot and ankle OA were formulated, and linked to the severity of the experienced disease burden as measured with the ABCC-tool. Treatment recommendations for pain and joint stiffness consisted of four different steps (i.e. education and lifestyle recommendations, pain medication, corticosteroid injections, and referring to other specialists), while recommendations for activity avoidance were based on education and referrals. These formulated recommendations require clinical judgement of the healthcare professional, in collaboration with the patient, to tailor them into an individualized care plan.
During the review process it was noticed that all OA guidelines predominantly focus on pain management, while less attention was paid to joint stiffness or activity avoidance. This might be because from a healthcare professional’s perspective, joint stiffness is mainly considered a symptom in the diagnostic process and usually resolves on its own within 30 minutes. It appears that this is being overlooked in the treatment process and has therefore not been included in guidelines, despite patients indicating during the development process of the OA module of the ABCC-tool that joint stiffness was a significant burden [7].
For activity avoidance, only two guidelines were retrieved, for hip and knee OA [25,26]. OA guidelines mostly focus on the physical burden of OA, while avoiding activities due to OA is more of a mental burden. Mental burden guidelines or studies are mostly limited to depression and anxiety in general [46]. To gain further insight into recommendations for activity avoidance, we conducted an additional literature review. Unfortunately, no relevant reviews were found. However, the purpose of the ABCC-tool is to focus on the physical, emotional and social burden of OA. Therefore, to create recommendations we consulted an expert in MSK disorders and discussed this topic extensively during the consensus meeting.
Although we intended to only include systematic reviews in this study, we included two RCTs as well [42,43]. These studies included a new insight into intra-muscular injections as a treatment for pain, which is a relatively new recommendation not yet included in guidelines.
As far as we know, this is the first study that attempts to translate clinical guidelines into practical recommendations for patients with OA. As mentioned earlier, the goal is not to facilitate ‘cookbook medicine’ but rather facilitating the process of making a personalized care plan, where the interaction between healthcare professional and patient is still essential. By providing a more step by step approach, patients can be involved and can become active partners in their own care process.
Strengths and limitations
This study has several strengths. First, we reviewed guidelines from five countries and two international organizations (OsteoArthritis Research Society International (OARSI) and European Alliance of Associations for Rheumatology (EULAR)) [39,40]. When no guidelines were available, international databases were searched to ensure all relevant evidence was included. Second, guidelines for various joints were considered, allowing us to create general OA treatment recommendations with joint-specific options where relevant, important since many patients have OA in multiple joints. Third, the literature review was conducted by two researchers, to ensure all relevant literature was included and to reduce selection bias and improving reliability [47-49]. Fourth, all treatment recommendations are based on consensus by a group of specialized GPs.
In addition, there are some limitations in this study. First, only English and Dutch guidelines were included due to language constraints. Still, as these are based on international evidence, we believe no key information was missed [50,51]. Within these guidelines, most physical therapy and orthopedic surgery guidelines focused on hip and knee OA, with hand, wrist, foot, and ankle guidelines only available from the American Academy of Orthopedic Surgeons [3,36]. General practice and rheumatology guidelines mainly covered hip, knee, hand, and wrist OA. Furthermore, guidelines focusing on OA in general, so not joint specific, for example the National Institute for Health and Care Excellence (NICE) guidelines, were not included [52]. However, a subsequent review of these NICE guidelines revealed no additional relevant information that would have impacted on our treatment recommendations. Second, the consensus process involved only specialized GPs, lacking input from other disciplines like physical therapy or orthopaedics. However, we included multidisciplinary guidelines to capture diverse perspectives.
Third, the domain of joint stiffness was added to the ABCC-tool later due to co-creations processes used in the development and validation phase [7]. Therefore, recommendations for this domain were developed subsequently, using the same methodology. Additionally, a search of the guidelines was performed to check for new or updated guidelines for the domains pain and activity avoidance. Fourth, we did not conduct an independent risk of bias assessment for the included reviews, as our analysis focused on existing clinical guidelines. However, these guidelines are generally developed through rigorous processes, with guideline committees typically assessing the quality of the underlying evidence using standardized methods such as the GRADE approach.
Implications for future research
The aim of the ABCC-tool is to help patients address their experienced physical, emotional and social burden of disease and create personalized goals with their healthcare professional. By incorporating evidence-based treatment recommendations for OA into this tool, these personalized goals can be translated into a personalized care plan, characterized by a stepped care approach. Previous research showed an increase in perceived quality of care and patient activation after using the ABCC-tool for patients with COPD, asthma, diabetes mellitus type 2 and heart failure [53]. As with this final element of the OA module the development for OA is now completed and could be implemented and pilot tested in clinical practice.
Conclusion
By translating evidence-based clinical practice guidelines and additional evidence from current studies into practical treatment recommendations following a stepped care approach, care for people with OA can now be delivered in a more structured, evidence-based and personalized way. With this step completed, the development process of the ABCC-tool for OA is finished. The next step of the ABCC-tool for OA is the implementation phase.
Acknowledgements
We would like to thank the members of the Dutch College of General Practitioners expert group of GPs specialized in MSK disorders (NHG-expertgroep Het Beweegkader) for their attendance and participation in this study.
Conflict of interest statement
There are no conflicts of interest.
Financial and Material support
This study was funded by Reuma Nederland (NSP22-1-303). The funding party had no role in study design, interpretation or manuscript writing.
References
- Belo JN, Bierma-Zeinstra SMA, Kuijpers T, Opstelten W, Van den Donk M, et al. (2016) Non-traumatic knee complaints.
- Royal Australian College of General Practitioners (2018) Guideline for the management of knee and hip osteoarthritis.
- American Academy of Orthopeadic Surgeons (2024) Arthritis of the Foot and Ankle.
- Grol R, Cluzeau FA, Burgers JS (2003) Clinical practice guidelines: towards better quality guidelines and increased international collaboration. Br J Cancer 89 Suppl 1(Suppl 1): S4-8.
- Wollersheim H, Burgers J, Grol R (2005) Clinical guidelines to improve patient care. Neth J Med 63(6): 188-192.
- Burgers JS, Hamming JF, Smulders YM (2022) Are guidelines still supportive in clinical practice? Ned Tijdschr Geneeskd 166: D6953.
- Debie VHJ, Boymans TAEJ, Ottenheijm RPG, van Schayck OCP, Gidding-Slok AHM (2024) Expanding the ABCC-tool for Osteoarthritis: Development and Content Validation. Osteoarthritis and Cartilage Open 6(3): 100488.
- Debie VHJ, Boymans TAEJ, Gidding-Slok AHM, van Schayck OCP, Ottenheijm RPG, et al. (2025) The Assessment of Burden of Chronic Conditions (ABCC-) Tool: A Valid and Reliable Tool for Hip, Knee, Hand, Wrist, Foot and Ankle Osteoarthritis. Osteoarthritis and Cartilage Open 7(3):100623.
- Claessens D, Boudewijns EA, Keijsers LC, Gidding Slok AHM, Winkens B, et al. (2023) Validity and Reliability of the Assessment of Burden of Chronic Conditions Scale in the Netherlands. The Annals of Family Medicine 21(2): 103-111.
- Boudewijns EA, Claessens D, van Schayck OC, Keijsers LCEM; Salome PL, et al. (2020) ABC-tool reinvented: development of a disease-specific ‘Assessment of Burden of Chronic Conditions (ABCC)-tool’for multiple chronic conditions. BMC family practice 21(1): 1-7.
- Slok AHM, Bemelmans TCH, Kotz D, Molen Tvd, Kerstjens HAM, et al. (2016) The Assessment of Burden of COPD (ABC) scale: a reliable and valid questionnaire. COPD: Journal of Chronic Obstructive Pulmonary Disease 13(4): 431-438.
- Slok AHM, Chavannes NH, van der Molen T, Molen TVD, Molken PHM, et al. (2014) Development of the Assessment of Burden of COPD tool: an integrated tool to measure the burden of COPD. NPJ Primary Care Respiratory Medicine 24(1): 14021.
- Keijsers LCEM, Peters LHL, van Schayck OCP, et al. Development and psychometric properties of the ‘Assessment of Burden of Chronic Conditions (ABCC-)tool’ for people with chronic heart failure (CHF) – a mixed methods approach. Submitted.
- Debie VHJ, Peters LHL, van Schayck OCP, et al. Patient perspectives on the usability and content validity of the Assessment of Burden of Chronic Conditions (ABCC-) tool for post-COVID: a qualitative study. Submitted.
- James D, Warren-Forward H (2015) Research methods for formal consensus development. Nurse researcher 22(3): 35-40.
- Griffin DR, Dickenson EJ, O'Donnell J, Agricola R, Awan T, et al. (2016) The Warwick Agreement on femoroacetabular impingement syndrome (FAI syndrome): an international consensus statement. Br J Sports Med 50(19): 1169-1176.
- Australian Physiotherapy Asscociation (2019) RACGP Guidelines for the Management of Hip & Knee OA.
- Australian Orthopeadic Association (2020) The management of knee osteoarthritis.
- Arthritis information sheet (2018) Tips for OA of the hip or knee 2018. Arthritis Autralia, Australian Rheumatology Association.
- The collge of Family Physicians of Canada, Centre for Effective Practice, Arthritis Alliance of Canada (2017) Osteoarthritis Tool.
- Kopka M, Sheehan B, Degen R (2020) Arthroscopy Association of Canada (AAC) Position Statement on Intra-Articular Injections for Knee Osteoarthritis.
- Belo JN, Bierma-Zeinstra SMA, Kuijpers T, Opstelten W, Van den Donk M, et al. (2016) Non-traumatic knee complaints.
- Nederlandse Huisartsen Genootschap, Nederlandse Orthopedische Vereniging, Koninklijk Nederlands Genootschap voor Fysiotherapie, et al. (2020) Treatment for osteoarthritis in the knee.
- Greving J K-PA, Kuijpers T, Krastman P, Peters-Veluthamaningal C, de Vries A, Wolters R (2021) Hand- and wrist complains.
- Koninklijk Nederlands Genootschap voor Fysiotherapie (2018) Royal Dutch Society for Physical Therapy- guidelines osteoarthritis hip and knee.
- Federatie Medisch Specialisten (2019) Conservative treatment of osteoarthritis in the hip or knee.
- Nederlandse Orthopedische Vereniging (2021) Isolated medial and lateral osteoarthritis of the knee.
- Federatie Medisch Specialisten, nederlandse Orthopedische Vereniging (2021) Choice card Osteoarthritis in the hip.
- Nederlandse Vereniging voor Reumatologie (2022) Treatment of hand osteoarthritis.
- British Orthopaedic Assocoation (2017) Commission Guide: Painful Osteoarthritis of the knee.
- Avruskin A (2023) Physical Therapy Guide to Hip Osteoarthritis.
- Stanley L (2022) Physical Therapy Guide to Knee Osteoarthritis.
- American Academy of Orthopedic Surgeons (2023) Management of Osteoarthritis of the Hip: Evidence-Based Clinical Practice Guideline.
- American Academy of Orthopeadic Surgeons (2025) Osteoarthritis of the hip.
- American Academy of Orthopeadic Surgeons (2019) Knee Osteoarthritis.
- American Academy of Orthopeadic Surgeons (2023) Arthritis of the Hand.
- American College of Rheumatology (2019) American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the Hand, Hip, and Knee.
- Fuggle N, Bere N, Bruyère O, Rosa Mm, Yerro MCP, et al. (2022) Management of hand osteoarthritis: from an US evidence-based medicine guideline to a European patient-centric approach. Aging Clin Exp Res 34(9): 1985-1995.
- Bannuru RR, Osani MC, Vaysbrot EE, Arden NK, Bennell K, et al. (2019) OARSI guidelines for the non-surgical management of knee, hip, and polyarticular osteoarthritis. Osteoarthritis and Cartilage 27(11): 1578-1589.
- Kloppenburg M, Kroon FP, Blanco FJ, Doherty M, Dziedzic KS, et al. (2019) 2018 update of the EULAR recommendations for the management of hand osteoarthritis. Annals of the Rheumatic Diseases 78(1): 16-24.
- Rausch Osthoff A-K, Niedermann K, Braun J, Adams J, Brodin N, et al. (2018) 2018 EULAR recommendations for physical activity in people with inflammatory arthritis and osteoarthritis. Annals of the Rheumatic Diseases 77(9): 1251-1260.
- Dorleijn DMJ, Luijsterburg PAJ, Reijman M, Kloppenburg M, Verhaar JAN, Bindels PJE, et al. (2018) Intramuscular glucocorticoid injection versus placebo injection in hip osteoarthritis: a 12-week blinded randomised controlled trial. Ann Rheum Dis 77(6): 875-882.
- Wang Q, Mol MF, Bos PK, Dorleijn DMJ, Vis M, et al. (2022) Effect of Intramuscular vs Intra-articular Glucocorticoid Injection on Pain Among Adults with Knee Osteoarthritis: The KIS Randomized Clinical Trial. JAMA Netw Open 5(4): e224852.
- Steultjens M (2003) Pain and functional disability in patients with osteoarthritis: the avoidance model.
- Vannabouathong C, Del Fabbro G, Sales B, Smith C, Silvia LC, et al. (2018) Intra-articular Injections in the Treatment of Symptoms from Ankle Arthritis: A Systematic Review. Foot & Ankle International 39(10): 1141-1150.
- Zhou Y, Dai X, Ni Y, Zeng Q, Cheng Y, et al. (2023) Interventions and management on multimorbidity: An overview of systematic reviews. Ageing Research Reviews 87: 101901.
- Delgado-Rodríguez M, Sillero-Arenas M (2018) Systematic review and meta-analysis. Med Intensiva (Engl Ed) 42(7): 444-453.
- Mokkink LB, Prinsen CA, Patrick DL, Alonso J, Bouter LM, et al. (2017) COSMIN methodology for systematic reviews of Patient‐Reported Outcome Measures (PROMs).
- Prinsen CAC, Mokkink LB, Bouter LM, J Alonso, D L Patrick, et al. (2018) COSMIN guideline for systematic reviews of patient-reported outcome measures. Qual Life Res 27(5):1147-1157.
- Zhang Y, Akl EA, Schünemann HJ (2019) Using systematic reviews in guideline development: the GRADE approach. Res Synth Methods 10(3).
- Platz T (2021) Methods for the Development of Healthcare Practice Recommendations Using Systematic Reviews and Meta-Analyses. Front Neurol 12: 699968.
- National Institute for Health and Care Excellence (2022) Osteoarthritis in over 16s: diagnosis and management.
- Boudewijns EA, Claessens D, van Schayck OC, Twellaar M, Winkens B, et al. (2024) Effectiveness of the Assessment of Burden of Chronic Conditions (ABCC)-tool in patients with asthma, COPD, type 2 diabetes mellitus, and heart failure: A pragmatic clustered quasi-experimental study in the Netherlands. European Journal of General Practice 30(1): 2343364.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.