Threatened Miscarriage in a Bicornuate Uterus: With the Baby in the Right Cornua and Subchorionic Hematoma in The Left Cornua
by Maryam M Y Mohammad*
Department of Obstetrics and Gynecology, Maternity Hospital, Kuwait
*Corresponding author: Maryam M Y Mohammad, Kuwait Institute for Medical Specialization (KIMS) -Ministry of Health in Kuwait
Received Date: 23 June 2024
Accepted Date: 29 June 2024
Published Date: 02July 2024
Citation: Maryam Mohammad (2024) Threatened Miscarriage in a Bicornuate Uterus: With the Baby in The Right Cornua and Subchorionic Hematoma in The Left Cornua. Gynecol Obstet Open Acc 8: 204. https://doi.org/10.29011/2577-2236.100204
Abstract
A bicornuate uterus has a fundus that is indented >1 cm with normal vagina and cervix. Bicornuate uterus accounts for around 25% of overall Mullerian anomalies. In this case report, we report a case of a 30-year-old female P1+1+0+2 14+2 weeks of gestation previous one cesarean section case of bicornuate uterus presented to the emergency department with lower abdominal pain and bleeding per vagina. She was admitted for observation as a case of threatened miscarriage. Ultrasound done showing bicornuate uterus with single living fetus matching date in the right cornu and a sub chorionic hematoma (SCH) in the left cornu. Patient was kept in the hospital under observation then she was discharged on progesterone tablets and suppositories. She underwent elective cesarean section at 38 weeks of gestation with good outcome.
Introduction
A bicornuate uterus has a fundus that is indented >1 cm with normal vagina and cervix. It results from partial rather than complete fusion of the Mullerian ducts. Depending on the extent of fusion, separation of the uterine horns will be complete, partial, or minimal [1]. The diagnosis is based on ultrasound findings of two usually moderately separated or divergent endometrial cavities and three-dimensional ultrasound is preferred over twodimensional ultrasound as it gives clear margins of the serosal and endometrial surface of the bicornuate uterus [1]. The incidence of congenital uterine anomalies is approximately 6.7% in the general population [2]. A bicornuate uterus accounts for 10-25% of all congenital uterine anomalies [3]. Bicornuate uterus is often asymptomatic and diagnosed incidentally [1]. It is associated with other anomalies affecting the abdominal wall, renal system and skeletal system [4]. It can affect both the obstetric and gynecological populations. In the gynecological population it can lead to pelvic pain, abnormal uterine bleeding and genital tract infections [4]. As for the obstetrical population it has been associated with recurrent pregnancy loss, preterm labor with its associated complications on the preterm born fetus and postpartum hemorrhage (PPH) [4].
Case Presentation
30-year-old female G3P1+1+0+2 14+2 weeks of gestation previous one cesarean section due to failure to progress and a known case of bicornuate uterus presented to the emergency department with lower abdominal pain and bleeding per vagina. She was admitted for observation as a case of threatened miscarriage. Ultrasound done showing bicornuate uterus with single living fetus matching date in the right cornua and a sub chorionic hematoma (SCH) measuring 55x32x29 mm in the left cornua (as shown in figure 1).
The patient was admitted to the hospital for observation as this was the first episode, she experienced in all of her pregnancies. She was kept on oral progesterone tablets and progesterone suppositories per vagina. During her hospital stay she reported similar episodes of vaginal bleeding however, much milder in severity. A Repeat ultrasound was done after 6 days from her admission which revealed bicornuate uterus with single living fetus matching date in the right cornua and a sub chorionic hematoma (SCH) measuring 48x20x14 mm in the left cornua decreasing in size in comparison to previous ultrasound scan.
The patient was discharged from the hospital and advised to come to the emergency department in case of any abdominal pain, leaking or per vaginal bleeding. She was given an outpatient appointment after one week from hospital discharge for follow up in which she denied any of the previous mentioned symptoms. She was managed in the antenatal clinic as per hospital protocol. When she reached 18 weeks of gestation anomaly scan done which was normal. By 24 weeks she took the oral glucose tolerance test (OGTT) in which results where normal. The remainder of her antenatal follow up was unremarkable. She never had any bleeding episode after her hospital admission. She was given the choice of vaginal birth after cesarean section or an elective repeat cesarean section with all risks and benefits explained. The patient opted for elective repeat cesarean section which was done when she reached 38 weeks of gestation. She delivered alive baby boy 2.9 kg APGAR score 8 and 9. She was discharged on post-operative day three post cesarean section as per hospital protocol. She was given an outpatient clinic appointment after her discharge. Patient was seen in the clinic after her discharge she was doing well with no complaint and asked for contraception. As she was breast feeding options of progesterone only contraception offered for her in which she chose to go with the progesterone only pill (POP).

Figure 1: Bicornuate uterus with fetus in right cornua and SCH in left cornua
Discussion
A bicornuate uterus has a fundus that is indented >1 cm with normal vagina and cervix. It results from partial rather than complete fusion of the Mullerian ducts. Depending on the extent of fusion bicornuate uterus can be classified accordingly [1] (as shown in figure 2 [4]). The diagnosis is made by the presence of two usually moderately separated or divergent endometrial cavities and an indented fundal contour. 3D ultrasonography can reliably differentiate between septate and bicornuate uteri as it can simultaneously visualize both the external or serosal surface and internal or uterine cavity contours of the uterine fundus. MRI is seldom needed to make a definitive diagnosis and should be reserved for times when there is no available or experienced ultra-sonographer [1]. The incidence of congenital uterine anomalies is approximately 6.7% in the general population, 7.3% in the infertile population, and 16.7% in the recurrent pregnancy loss population [2]. A bicornuate uterus accounts for 10-25% of all congenital uterine anomalies [3].
Patients with congenital uterine anomalies are also considered at increased risk of having renal, skeletal, or abdominal wall abnormalities and vice versa [1]. Most patients with bicornuate uterus are asymptomatic and the anomaly is diagnosed incidentally on imaging studies, as a result of imaging studies [1]. As for symptomatic patients they may present with cyclic or noncyclic pain, abnormal vaginal bleeding, and/or infection. In nonpregnant patients, bicornuate uterus can lead to hematometra, hematocolpos, retrograde menstruation, pelvic pain, abnormal uterine bleeding, or genital tract infection [1]. Bicornuate uterus is linked to many adverse obstetrical complications including: spontaneous abortion in 36 percent, preterm birth in around 23 percent, and fetal survival in 50 to 60 percent of patients with a bicornuate uterus. In addition, there is an increased incidence of fetal malpresentation and fetal growth restriction in patients with bicornuate uterus [1]. Finally, the incidence of preterm labor is increased in patients with uterine anomalies including a bicornuate uterus and this is linked due to the decreased gestational capacity of a bicornuate uterus [5]. Complications affecting the fetus or child related to preterm delivery includes the following: higher rates of admission to neonatal intensive care unit (NICU), respiratory distress syndrome (RDS), retinopathy of prematurity, neonatal jaundice, neurodevelopmental and growth impairment on the long term [6].
In patients with poor pregnancy outcomes attributed to the uterine anomaly, uterine reunification can be performed via laparotomy as one study showed increasing birth rate in patients who underwent corrective surgery [3]. However, it is important to point that the probability of giving birth to a live-born infant after corrective surgery in the first and second pregnancy was 71 and 86 percent, respectively with an increasing likelihood of success with increasing number of pregnancies [5]. Surgical correction of a congenital uterine anomaly is not indicated in asymptomatic patients or those with primary infertility [1]. Surgical indications for corrective surgery include the following: recurrent pregnancy loss after exclusion of other contributing causes and dysmenorrhea if medical therapy is not effective [2]. Strassman procedure or metroplasty is the procedure of choice for uterine reunification via laparotomy in patients with bicornuate uterus (as shown in figure 3 [7]) [5]. The Strassman metroplasty joins the narrow uterine cornua of a bicornate uterus into one thus restoring the normal anatomical structure [8]. Surgical intervention with Strassman metroplasty might improve reproductive outcomes but was fund to be associated with increased chance of placenta previa, morbidly adherent placenta, and severe postpartum hemorrhage [9].
Finally, due to an association between bicornuate uterus and cervical insufficiency, the cervical length should be assessed during pregnancy before 24 weeks prior to cervical cerclage placement if indicated [1]. A review of 251 cervical cerclage procedures done over a period of seven years comparing McDonald Vs Shirodkar cervical cerclage (as shown in figure 4 [10]). This study concluded that overall Shirodkar cervical cerclage was associated with higher fetal survival rate if done either in the elective setting or an emergency setting [11]. On the other hand, McDonald cervical cerclage had fewer blood loss intraoperatively. However, the difference between the two procedures was not statistically significant as p value was >0.5 [11]. Finally, cervical laceration post cervical cerclage procedure was higher in patient who underwent Shirodkar procedure occurring in about 25% of patients in comparison with McDonald procedure as it was found in 16% of patients which in turn increased the rate of cesarean section [11]. Both McDonald and Shirodkar procedures are performed vaginally and in comparison, with transabdominal cerclage (as shown in figure 5) which is the treatment of choice for women with failed vaginal cerclage or in women with history of cervical trauma or trachelectomy [12].
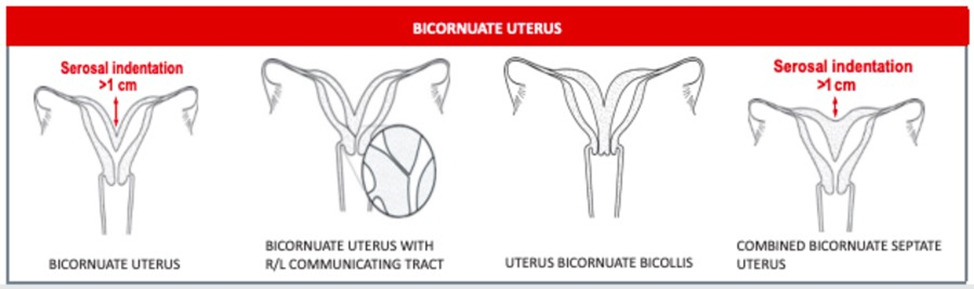
Figure 2: Classification systems for Mullerian anomalies [Photo Credits: American Society of Reproductive Medicine (ASRM)] [4]
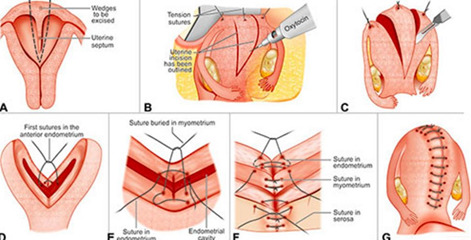
Figure 3: Strassman metro plasty (Photo Credits: Tips & Tricks in Operative Obstetrics & Gynecology Book [8])
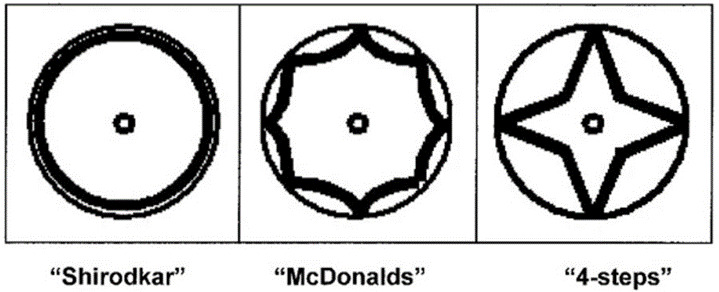
Figure 4: McDonald Vs Shirodkar Cervical Cerclage (Photo Credits: Clinical aspects of cervical insufficiency [11])
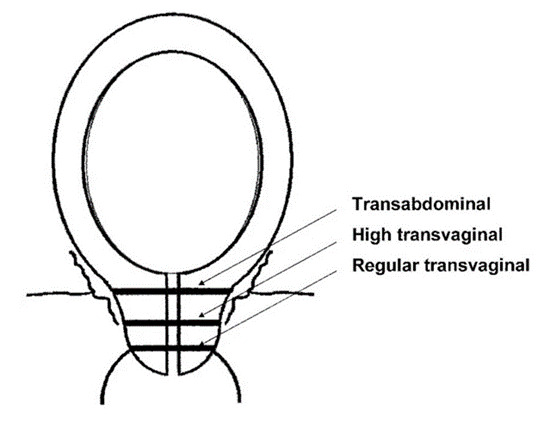
Figure 5: Placement of cervical cerclage (Photo Credits: Clinical aspects of cervical insufficiency [11])
Conclusions
In conclusion, the exact prevalence of a bicornuate uterus is unknown. It is important for the treating physician to be aware of the different uterine anomalies and their obstetrical and gynecological implications. Although a bicornuate uterus does not always lead to complications and can carry a pregnancy to term by normal vaginal delivery with no complications. In this case report we reported a case of bicornuate uterus with a fetus in the right cornua and placental tissue in the left cornua and this pregnancy completed to term which is a surprising yet interesting finding. This proves that increasing number of pregnancies is associated with increase success rate of reaching term it also necessitates the importance of proper patient selection prior commencing any surgical intervention.
Declarations
· Ethics approval and consent to participate
-Consent was taken from the patient and she was informed that data will be displayed in a manner insuring her confidentiality
· Consent for publication
-Consent was taken from the patient and she was informed that data will be displayed in a manner insuring her confidentiality
· Availability of data and materials
-All data and materials are available upon request
· Competing interests
-None
· Funding
-None
· Authors' contributions in this paper
- Conceived and designed the analysis
- Collected the data
- Contributed data or analysis tools
- Performed the analysis
- Wrote the paper
· Acknowledgements
-None
· Authors' affiliation
- Kuwait Institute for Medical Specialization (KIMS), Ministry of Health in Kuwait (MOH)
· Authors' information
- Dr. Maryam Mefarreh Yousef Mohammad
- Royal College of Surgeons in Ireland – Medical University of Bahrain (RCSI-MUB) 2019 Alumni
- Bachelor of Medicine, Bachelor of Surgery degree and Bachelor of the Art of Obstetrics (MB, BCh, BAO)
- Currently a Resident in Kuwait Board of Obstetrics and Gynecology (KBOG)
- Currently working in Maternity Hospital in Kuwait
- Email Address: Dr.maryam.mohammad@gmail.com
- Phone Number: 00965-98758300
References
- R Laufer M. Resident, Fellow, or Student Hospital or Institution Group Practice Congenital uterine anomalies: Clinical manifestations and diagnosis [Internet]. L Barbieri R, H DeCherney A, editors. UpToDate. UpToDate; [cited 2024 Jul 2]. Available from: https://www.uptodate. com/contents/congenital-uterine-anomalies-clinical-manifestationsand-diagnosis
- Saravelos SH, Cocksedge KA, Li TC (2008) Prevalence and diagnosis of congenital uterine anomalies in women with reproductive failure: a critical appraisal. Hum Reprod Update 14: 415-29.
- Troiano RN, McCarthy SM (2004) Mullerian duct anomalies: imaging and clinical issues. Radiology 233: 19- 34.
- Samantha M. Pfeifer, Marjan Attaran, Jessica Goldstein (2021) ASRM mullerian anomalies classification 2021. Fertility and Sterility 116: 1238-1252.
- Maneschi F, Marana R, Muzii L, Mancuso S (1993) Reproductive performance in women with bicornuate uterus . Acta Europaea Fertilitatis 24: 117-20.
- T Mandy G. Overview of the long-term complications of preterm birth [Internet]. Martin R, editor. UpToDate. UpToDate; [cited 2024 Jul 2]. Available from: https://www.uptodate.com/contents/overview-of-thelong-term-complications-of-preterm-birth
- Richa Saxena (2011) Tips & tricks in operative obstetrics and gynecology .Jaypee Digital ebook reader.
- Zhang C, Wang X, Jiang H (2021) Placenta percreta after Strassman metroplasty of the complete bicornuate uterus: a case report. BMC Pregnancy and Childbirth. 2021, 29: 21.
- Gagnier J, Kienle G, Altman DG (2014) The CARE guidelines: consensus-based clinical case report guideline development. J Clin Epidemiol 67: 46-51.
- Lotgering FK(2007) Clinical aspects of cervical insufficiency. BMC Pregnancy and Childbirth 7: 17.
- Harger JH (1980) Comparison of Success and Morbidity in Cervical Cerclage Procedures. Obstetrics & Gynecology 56:543.
- Shennan A, Chandiramani M, Bennett P (2019) A Multicentre Randomised Controlled Trial of Transabdominal Versus Transvaginal Cervical Cerclage. American Journal of Obstetrics and Gynecology 222: 261.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.