Thermal Camera Application in Gynecological Oncology: Feasibility Study of a Novel Technology
by Sayasneh A1,2*, Abdelbar A1,3*, Ramajayan T1, Lim J1, Al-karawi D4, Al Zaidi S4, Alazzam M5, Mehra G1, Muallem MZ6
1Department of Gynecological Oncology, Surgical Oncology Directorate, Guy’s and St Thomas’ NHS Foundation Trust, London, SE1 7EH, UK
2School of Life Course Sciences, Faculty of Life Sciences and Medicine, King’s College London, Westminster Bridge Road, London SE1 7EH, UK
3Department of Obstetrics and Gynaecology, Cairo University, Cairo, Egypt
4Medical Analytica Ltd, 26a Castle Park Industrial Park, Flint, Flintshire, United Kingdom, CH6 5XA
5 Department of Gynecological Oncology, Oxford University Hospitals, Headington, OX3 7LN, UK
6Department of Gynecology with Center for Oncological Surgery, Charité - Universitätsmedizin Berlin, Corporate Member of Freie Universität Berlin, Humboldt-Universität zu Berlin and Berlin Institute of Health, Virchow Campus Clinic, Charité Medical University, 13353 Berlin, Germany
*Both authors contributed equally as first author.
*Corresponding author: Sayasneh A, Department of Gynecological Oncology, Surgical Oncology Directorate, Guy’s and St Thomas’ NHS Foundation Trust, London, SE1 7EH, UK
Received Date: 04 March, 2024
Accepted Date: 11 March, 2024
Published Date: 14 March, 2024
Citation: Sayasneh A, Abdelbar A, Ramajayan T, Lim J, Al-karawi D, et al. (2024) Thermal Camera Application in Gynaecological Oncology: Feasibility Study of a Novel Technology. J Oncol Res Ther 9: 10203. https://doi.org/10.29011/2574-710X.10203.
Abstract
Background: Although thermal imaging has been tried in medical practice before, its use in gynaecological oncology is not established in practice yet. Objectives: To assesses the feasibility of thermal imaging (infrared technology) for tumour detection during gynaecological oncological surgeries, and to explore the feasibility of enhancing surgical outcomes by using thermal camera. Methods: This prospective feasibility study was conducted at a London tertiary cancer centre in the period between September 2022 and September 2023. Preoperative and intraoperative thermal images were captured using a Flir One Pro smartphone thermal camera. Subsequent images analysis was performed to correlate temperature and colour variations to tumour presence. Results: Thermal images were captured for 26 patients. Thermal imaging was able to identify malignant tumours close to abdominal wall in 73.6% of the cases, with a sensitivity of 93.3% and a positive predictive value of 77.8%. Among these, seven patients were excluded due to suboptimal imaging quality. The technique was able to map tumour locations relatively accurately. (4) Conclusion: Thermal imaging presents a promising non-invasive approach for tumour localization in gynaecological oncology. It offers significant potential to improve surgical precision and possibly patient outcomes. Thermal could serve as a valuable adjunct to conventional diagnostics in gynaecological oncology patients. Further validation by larger studies using more advanced thermal imaging is still required before we can generalize these findings in clinical practice.
Keywords: Gynecological Oncology; Thermal Imaging; Tumor Detection; Preoperative Planning; Real-Time Imaging
Introduction
The United Kingdom recorded an annual incidence of 182,000 new cases of cancer among women in the period between 2016 and 2018. Breast cancer came first accounting for approximately one-third of the total number of cases. Uterine and ovarian cancers were the fourth and sixth common, respectively, among female cancers [1]. A wide range of imaging modalities have been implemented in clinical practice for the assessment of various gynecological cancers [2]. This includes computed tomography (CT) scans, magnetic resonance imaging (MRI), and positron emission tomography (PET CT) [2].
Thermography or near-infrared imaging (NIR) is a technique that uses infrared cameras to measure tissue temperatures. It is based on the understanding that malignant tumours show increased metabolic activity which can cause higher blood flow and a subsequent rise in temperature of the surrounding tissues. There are studies applied this technique to identify breast cancers by mapping the changes in surface temperature [3]. However, breast thermography remains adjunctive and not diagnostic due to the lack of evidence and the variability in tumour depth [4]. Nevertheless, the benefit of thermography is the fact it is a cost-effective non-invasive technique [4].
The literature data is limited when it comes to the use of thermography in gynaecological oncology including ovarian and endometrial cancers. This opens the door for more exploratory studies to assess the benefit, if any, of utilizing thermography in gynaecological oncology. Further research is certainly required to assess the potential of thermography in improving either early detection, monitoring, or intraoperative visualization of gynecological cancers. Ultimately, more future research is required to assess if thermography has any role in improving patient outcomes- in women’s cancer treatment. g. The main objective of this study is to evaluate the feasibility and applicability of infrared thermal imaging during gynecologyoncological surgeries.
Materials and Methods
This prospective cohort study was conducted at a tertiary cancer center in London between September 2022 and September 2023. The study was registered and approved by the Trust Clinical Governance board as a quality improvement project. Rigorous protocols in patient selection, training, and image acquisition were followed.
Patient Selection and Informed Consent:
Patients meeting the inclusion criteria, who were undergoing gynecological oncology surgery by the primary author (AS), provided written informed consent including permission for acquiring anonymized photography and infrared thermal images during surgical procedures. Criteria for inclusion were patients with primary or recurrent tumors, including those with large uterine or ovarian masses extending into the abdominal cavity, even if at early FIGO stages. Exclusion criteria involved FIGO stage 1 endometrial cancers in a normal-sized uterus without pelvic or abdominal masses, body mass index BMI =50, age <18 years, and recent use (within 2 hours before surgery) of abdominal creams, patches, or dressings.
Imaging Equipment and Setup:
Thermal images were captured using a Flir One Pro smartphone thermal camera (Flir One Pro Systems, Sweden). This portable device operates within the electromagnetic spectrum, detecting heat signatures in the range of 7.5 to 14 micrometers.
Training and Certification:
To ensure proficiency, the first author (AS) underwent online training provided by the Infrared Training Centre (ITC) [5] consisting of introductory videos and articles. AS further obtained thermography certification by attending a comprehensive three-day online course and passing an assessment test (certificate is attached in Supplementary Figure 1) from Teletherm Infrared Systems / Research, Tampa, FL, USA [6].
Trust board approval:
Approval for the use of the Flir One Pro (Flir One Pro Systems, Sweden) smartphone thermal camera was obtained from the Trust Department of Medical Physics. Further approvals from the Medical Photography Department and Clinical Governance at the Trust were obtained. The study was approved as a service evaluation project and was allocated an ID number by the trust.
Tumor Staging and Grading:
Tumor staging followed FIGO classification [7] and tumor grading adhered to the WHO classification [8].
Imaging Protocol:
In general, our thermal imaging methodology followed the International Academy of Clinical Thermology Guidelines [9]. Thermal images were captured in an appropriately sized operating theatre with the patient in the Lloyd Davis position post-anaesthesia. The Flir One Pro camera, used by author AS, was oriented with the top of the image facing towards the cephalic end of the patient.
Prior to capturing images, a waiting period of at least 10 minutes was observed to allow for equilibration with the room temperature, which was maintained between 18-23 degrees Celsius. This waiting period aimed to minimize any potential temperature variations due to the patient's entry into the operating theatre. The images were captured before the application of any skin preparation or bear huggers.
The camera attached to NHS approved IPad was positioned at a standardized distance of 30-40 cm from the patient's abdomen to ensure optimal focus and resolution. For each patient, 3 images were systematically captured. Images were acquired in normal intensity light, with all surgical lights turned off to eliminate external light interference.
Image Analysis:
The Flir One Pro camera utilized a colour spectrum to represent thermal variations, allowing for real-time temperature mapping. Three standardized images of the abdominal wall were captured before skin incision. The imaging process involved stabilizing the NHS registered IPad camera for five seconds to minimise artifacts. The camera, set at 1x zoom, was maintained parallel to the abdominal wall, capturing the entire area from the xiphisternum to the pubic bone. All data were stored into the Trust computer drive strictly following the hospital policy.
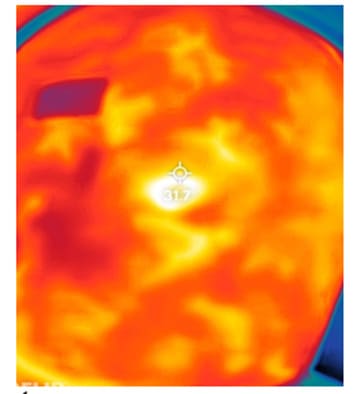
Colour variations and elevated temperatures were identified and correlated with one of the nine quadrants of the abdomen. The camera software automatically identified the hottest spot on the picture, and thermal values were measured in reference to the umbilicus (Figure 1).
The Camera Settings:
We have set emissivity of the Flir One Pro as 0.95 (matte). We used Celsius degrees for temperature units. Same colour scale was used in all images (Lava) were hottest is white, followed by yellow grades, red grades, green grades, blue grades and then coolest is black (Figure 1). If the hot spot is automatically identified by the software, it will look as a red cursor.
Data Collection and Analysis:
Intra-operative findings including bowel adhesions, abdominal wall deposits, hernial sacs, and the anatomical site of pelvic or abdominal tumors, were meticulously documented. Surgically excised tissues underwent histopathological examination, allowing for comprehensive analyses correlating intra-operative and histological findings with thermal images. The study adhered strictly to routine standard practices in patient management with no deviations from established clinical protocols and routine clinical practice.
Statistical Analysis
MedCalc® Statistical Software version 22.018 (MedCalc Software Ltd, Ostend, Belgium; https://www.medcalc.org; 2024) was used to allow statistical analysis. 95% confidence intervals CI were calculated for means and medians. Final histology as benign or malignant was considered as the reference test when calculating true and false positive and negative results. 2x2 contingency table was created to calculate diagnostic performance with 95% CI. To assess the statistical significance of thermal values, the chi-squared test was conducted, and p values below the conventional threshold of 0.05 were considered statistically significant.
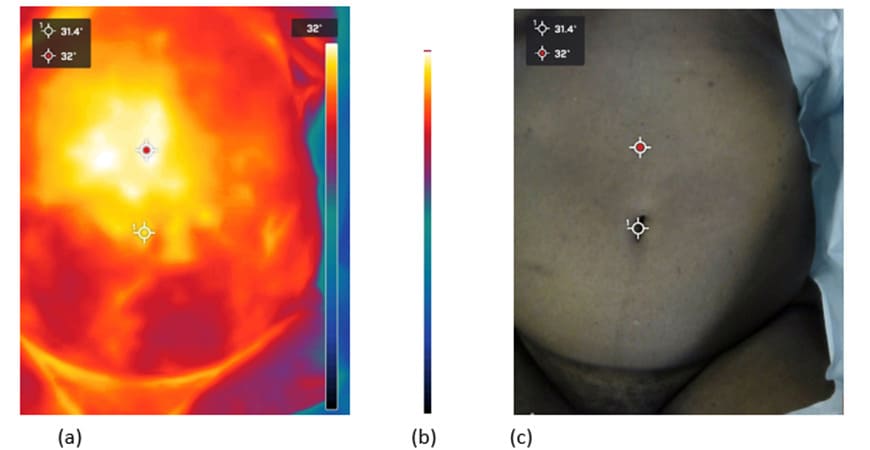
Figure 1: Capturing the hottest spots on the abdominal area in reference to the umbilicus. (a): Lava colour scale is used, as in the right side of the image. Red cursors are the automatically identified hottest spots, white cursor is made by the operator. (b): The Lava colour scale used through all images. (c): Same image in (a) with matching cursors on its conventional non-thermal photograph.
Results
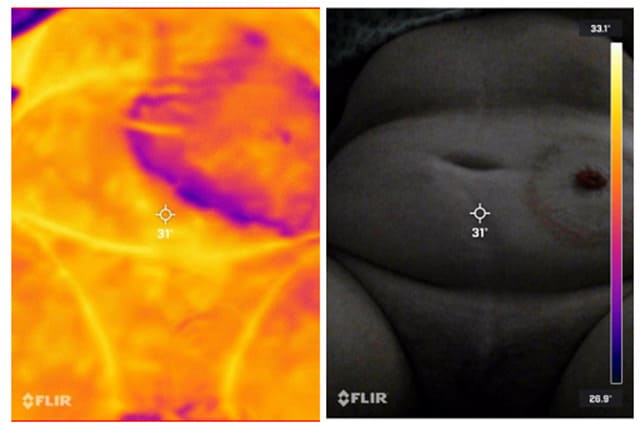
In this study, thermal imaging was used in 26 patients just before their scheduled surgeries. Of these, 7 patients were subsequently excluded from the analysis for following reasons: two patients were had their disease being in the early stage and confined to the pelvis(rendering thermal imaging ineffective because of bone shielding); two patients had antiseptics applied; two patients had stoma bags removed in the operating theatre (as this can affect skin temperature readings); and one patient was excluded due to a small drain dressing was removed in theatre (potentially interfered with the thermal imaging) (Figure 2).
A
B
C
D
Figure 2: Examples of the cases excluded from the study. (A) shows the cooling effect on the skin where a colostomy bag was removed, highlighting the impact of recent bag removal on thermal imaging. (B) shows the effect of anti-septic application on skin temperature, demonstrating how pre-operative preparations can influence thermal readings. (C) and (D) illustrate the thermal imaging appearances of dressings on a stoma site and a previous drainage site, respectively, underscoring the need for clear skin exposure to obtain accurate thermal images.
The study evaluated 19 patients after exclusions, with a mean age of participants of 50.9 years (95% CI: 44–59.2) and a mean BMI of 29.1 kg/m2 (95% CI: 25.1–33.1). Amongst these, ovarian cancer was diagnosed in 14 cases (73.7%). The final histopathology revealed FIGO stage III and IV cancers in 11 of the 19 cases (57.9%). Grade 3 cancers were predominant, representing 73.7% of the cases. Detailed demographics, cancer types, stages, and grades are summarized in Table 1.
|
Demographic parameters |
|||||||||
|
N |
Minimum |
Maximum |
Mean |
95% CI |
Median |
95% CI |
|||
|
Age |
19 |
24 |
70 |
50.9 |
44.7 to 57 |
54 |
44 to 59.2 |
||
|
BMI |
19 |
18 |
49 |
29.1 |
25.1 to 33.1 |
28.5 |
22.8 to 33.4 |
||
|
Other Demographic parameter |
N |
% |
|||||||
|
Ethnicity |
|||||||||
|
Asian |
2 |
10.50% |
|||||||
|
Black African |
6 |
31.60% |
|||||||
|
White other |
1 |
5.30% |
|||||||
|
White Caucasian |
10 |
52.60% |
|||||||
|
Comorbidities |
|||||||||
|
Acute Kidney Injury AKI3 |
1 |
5.30% |
|||||||
|
Hiatus hernia and hypothyroidism |
1 |
5.30% |
|||||||
|
Hypertension |
3 |
15.80% |
|||||||
|
No other comorbidity identified |
13 |
68.40% |
|||||||
|
Previous surgery |
|||||||||
|
Midline laparotomy |
3 |
15.80% |
|||||||
|
Transverse laparotomy |
1 |
5.30% |
|||||||
|
Laparoscopy |
2 |
10.50% |
|||||||
|
Chemotherapy before surgery |
|||||||||
|
No preoperative chemotherapy was given |
14 |
73.70% |
|||||||
|
Patient on chemotherapy between 3 to 6 weeks before surgery |
5 |
26.30% |
|||||||
|
Surgery performed |
|||||||||
|
Fertility preserving surgery (salpingoopherectomy with removal of the tumour) |
3 |
5.30% |
|||||||
|
Salvage palliative surgery (salpingoopherectomy) |
1 |
5.30% |
|||||||
|
Delayed or interval debulking surgery after neoadjuvant chemotherapy |
4 |
21.10% |
|||||||
|
Primary debulking surgery |
8 |
42.10% |
|||||||
|
Secondary debulking surgery |
3 |
15.80% |
|||||||
|
Final Histology |
|||||||||
|
Benign |
1 |
5.30% |
|||||||
|
Malignant |
18 |
94.70% |
|||||||
|
Primary origin of tumour |
|||||||||
|
Ovarian or Fallopian Tube |
17 |
89.40% |
|||||||
|
Endometrial |
1 |
5.30% |
|||||||
|
Unknown |
1 |
5.30% |
|||||||
|
Stage of disease |
|||||||||
|
FIGO I |
4 |
21,1% |
|||||||
|
FIGO II |
0 |
0 |
|||||||
|
FIGO III |
4 |
21.10% |
|||||||
|
FIGO IV |
7 |
36.80% |
|||||||
|
Cancer recurrence |
3 |
15.80% |
|||||||
|
Benign (no staging available) |
1 |
5.30% |
|||||||
|
Grade of disease |
|||||||||
|
1 |
2 |
10.50% |
|||||||
|
2 |
2 |
10.50% |
|||||||
|
3 |
14 |
73.70% |
|||||||
|
Benign |
1 |
5.30% |
|||||||
Table 1: Demographic Parameters.
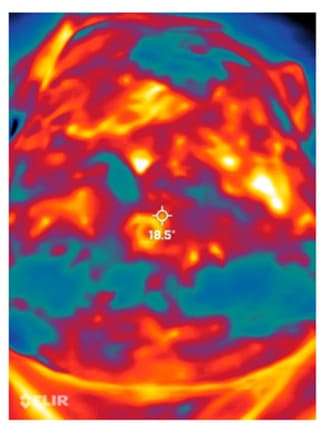
Thermal imaging successfully identified the cancer site with true positive results in 14 of the 19 cases (73.7%), as shown in Figure 3. There was one false negative instance, where the thermal camera identified a cool mass that was later confirmed as a malignant high-grade germ cell tumor (immature teratoma) in final histology (Figure 4). Additionally, there were four cases (21.1%) of false positives as shown in Figure 5.
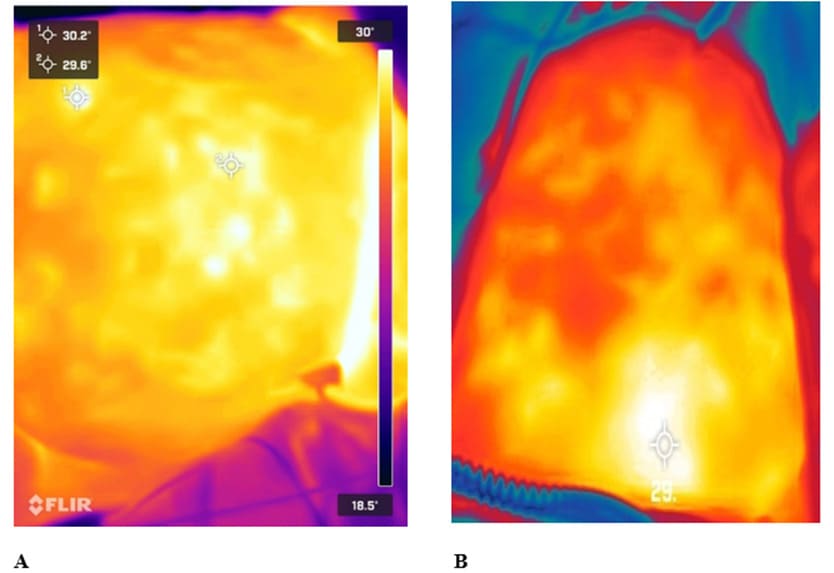
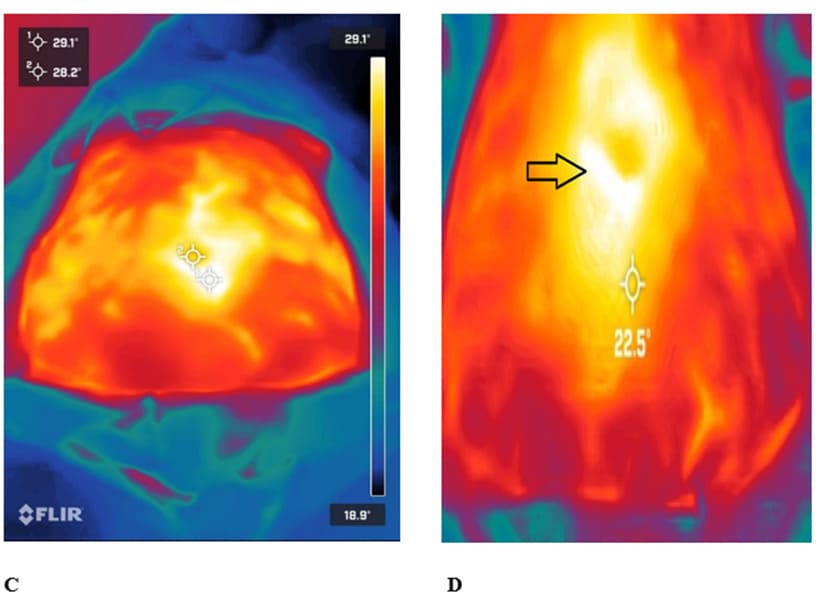
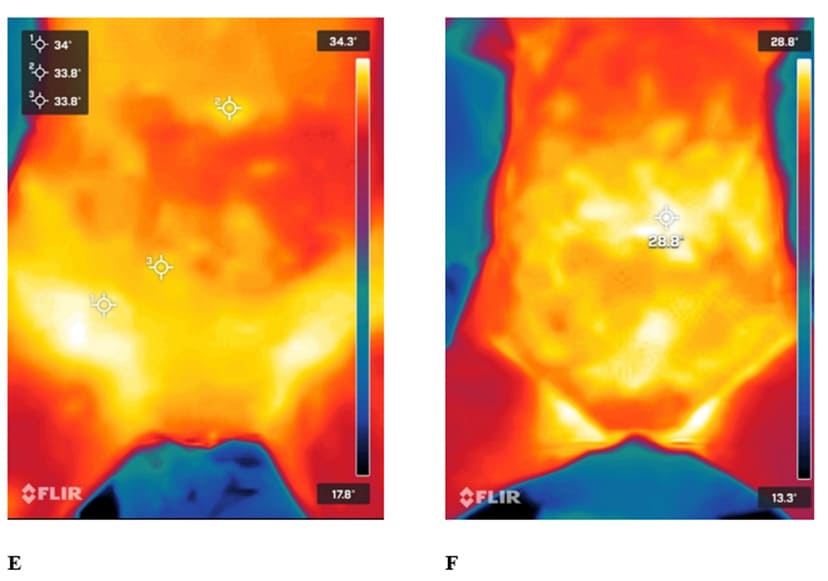
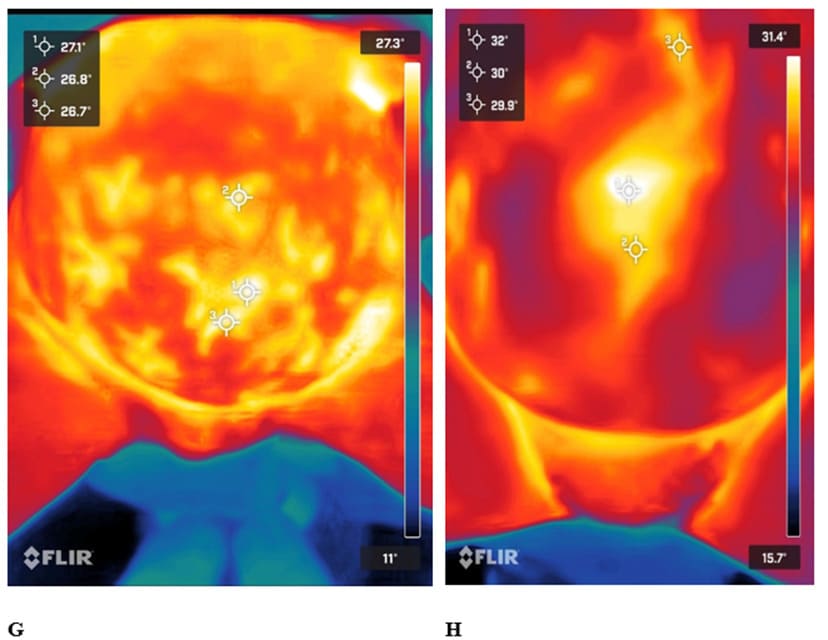
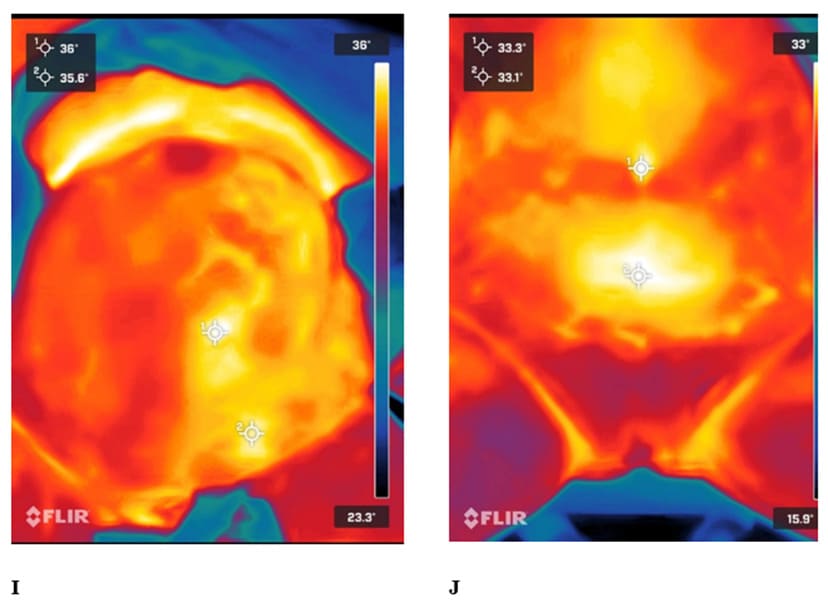
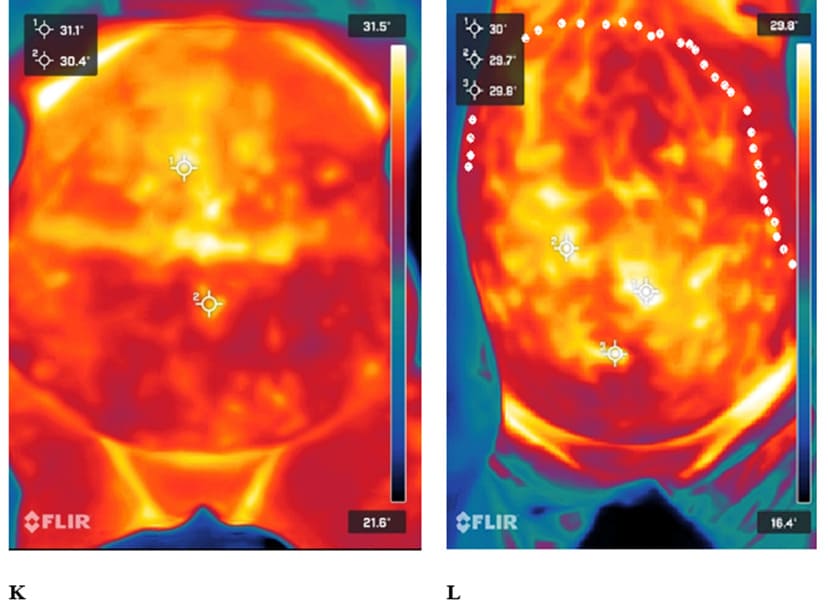
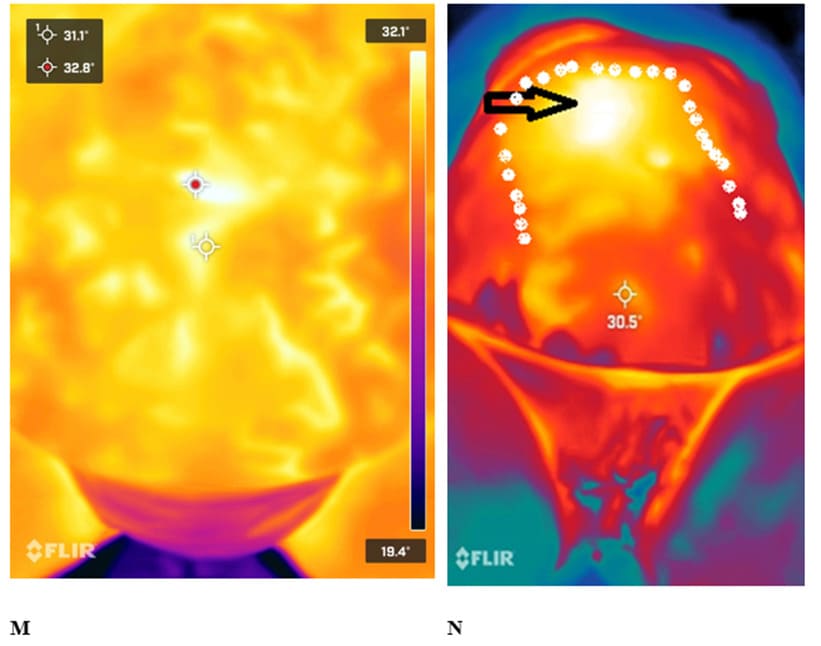
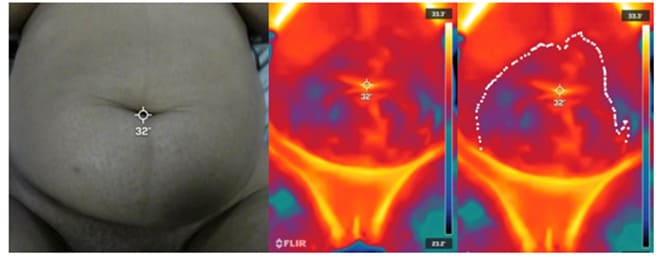
Figure 3: True positive cases. (A): Omental metastasis of high grade serous tubo-ovarian carcinoma adhered to abdominal wall (at cursor sites). (B): Peritoneal nodule of high grade serous tubo-ovarian adenocarcinoma (at cursor site). (C): Mucinous tubo-ovarian adenocarcinoma involving abdominal wall (at the lower cursor site). The other cursor is at the umbilicus. (D): High grade serous tubo-ovarian carcinoma (arrow) involving abdominal peritoneum. (E): High grade leiomyosarcoma extending to right groin (lower cursor). (F): High grade serous tubo-ovarian cancer with peritoneal deposits (cursor). (G): Widely disseminated peritoneal deposits, high grade mucinous adenocarcinoma of unknown primary. (H): Low grade serous adenocarcinoma of tubo-ovarian origin. (I): High grade serous tubo ovarian adenocarcinoma with bowel obstruction and dilated loops of small bowels (cool red right side of patient’s abdomen) and ileocaecal mass with small bowel serosal disease and peritoneal disease (cursor sites). (J): Recurrent high grade serous tubo-ovarian adenocarcinoma presenting as an ileocaecal mesenteric mass (low cursor). (K): High grade serous tubo-ovarian adenocarcinoma with omental cake adherent to anterior abdominal wall (upper cursor). (L): Large ovarian mass, FIGO IA endometrioid adenocarcinoma of the ovary(hottest points at curors and upper border of the mass is delineated). (M): Recurrent high grade serous tubo-ovarian carcinoma deposits in a para umbilical incisional hernia sac (red cursor) and the white cursor is the umbilicus. (N): Endometrioid adenocarcinoma mass (delineated)with hot activity (arrow).
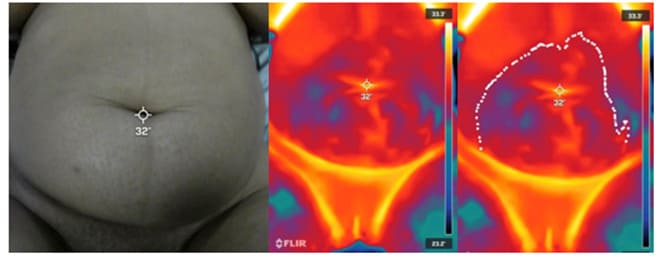
Figure 4: The false negative case. Although the subcutaneous tumour was delineated, it was not hot and therefore was considered as benign. Final histology was a germ cell immature teratoma.
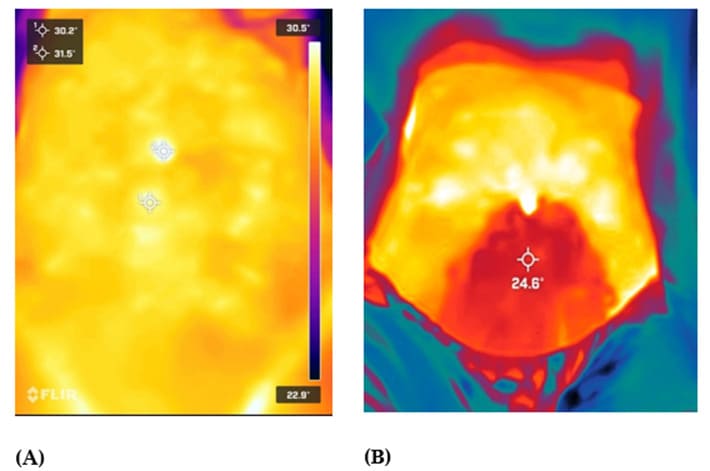
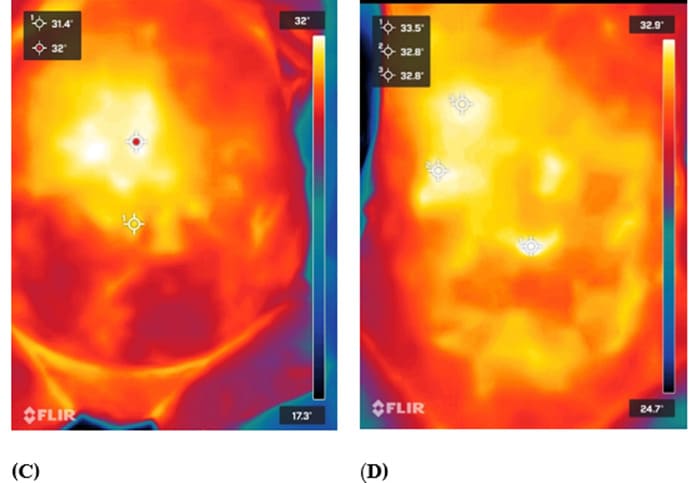
Figure 5: False positive cases. (A): This is a high grade serous tubo-ovarian adenocarcinoma where there is no disease in the hot spots (cursors) above the umbilicus and omentum was clear of disease. (B): 17-week pregnant uterus (note cool activity in pregnant uterus due to amniotic fluid) (cursor) with benign serous cystadenoma of the ovary. Hot spots above the umbilicus were not correlated to any malignancy. (C): Endomerial adenocarcinoma and the hottes spot (red cursor) was relating to a benign degenerating fibroid. (D): FIGO stage 1C tubo-ovarian endometrioid adenocarcinoma. Hot spots (cursors) did not correlate to cancer.
The thermal camera demonstrated a sensitivity of 93.3% (95% CI: 68.1-99.8%) in identifying abdominal surface malignancies and an accuracy of 73.7% (95% CI: 48.8-90.8%). Specificity calculation was not feasible due to the absence of true negative instances. The PPV was calculated at 77.8% (95% CI: 75.4-80%). Statistical analysis indicated no significant relationship between the hottest spot's value or the temperature differential between the hottest spots and the umbilicus for cancer prediction, with p-values of 0.3 and 0.1, respectively.
Other observed findings:
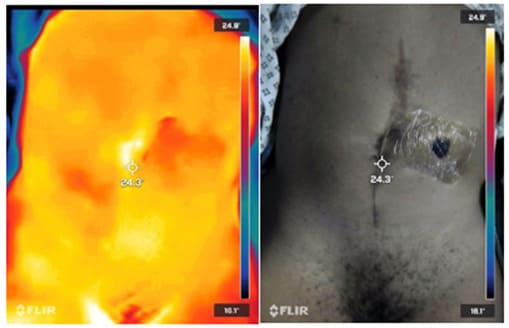
In our study, we obserced that thermal camera was capable of accurately localizing disease sites when affirmed as true positives and situated close to the abdominal wall, as demonstrated in Figures 6, 7, and 8. This precision in mapping highlights the potential of thermal imaging in identifying specific areas of pathology close to abdominal surface anatomy and may offer a non-invasive tool to pinpoint disease locations at the time of surgery. Conversely, areas showing as cooler regions on thermal imaging were frequently associated with fluid accumulations, such as amniotic fluid during pregnancy (illustrated in Figure 5, b) or dilated bowel loops indicative of bowel obstruction (Figure 5, i). This distinction between warmer and cooler areas may be valuable in differentiating solid masses from fluid collections. Furthermore, thermal imaging was able to show smaller cancer depsits, such as small <1 cm thickenning of para-umbilical hernia sac (Figure 9). This suggests that thermal imaging may contribute to the diagnostic process in cases where disease is adjacent to the abdominal wall.
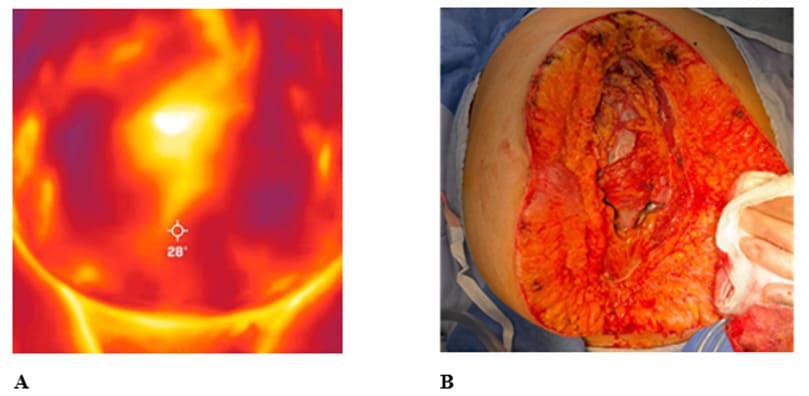
Figure 6: A case of metastatic high grade serous ovarian adenocarcinoma with omental cake on thermal imaging. (A): Pre-operative thermal image showing a hot color in the umbilical, suprapubic and epigastric regions. (B): Intra-operative image showing omental cake extending in the same anatomical area of bright color on thermal imaging.
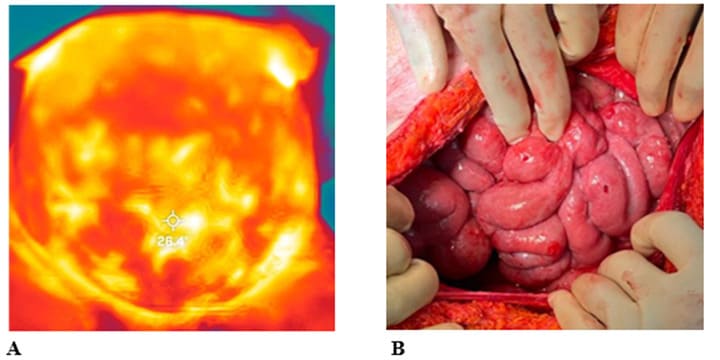
Figure 7: A case of mucinous adenocarcinoma (unknown primary) with metastatic upper intestinal serosal disease attached to anterior abdominal wall. (A): Pre-operative thermal image showing hot bright yellow areas corresponding to diseased bowel lying against anterior abdominal wall and darker areas where there are less disease and mor filmy fibrous adhesions leaving somedistance between bowels and anterior abdominal wall. (B):Intra-operative visualization after bowel adhesiolysis from the anterior abdominal wall reveals a confluence of bowel serosal disease.
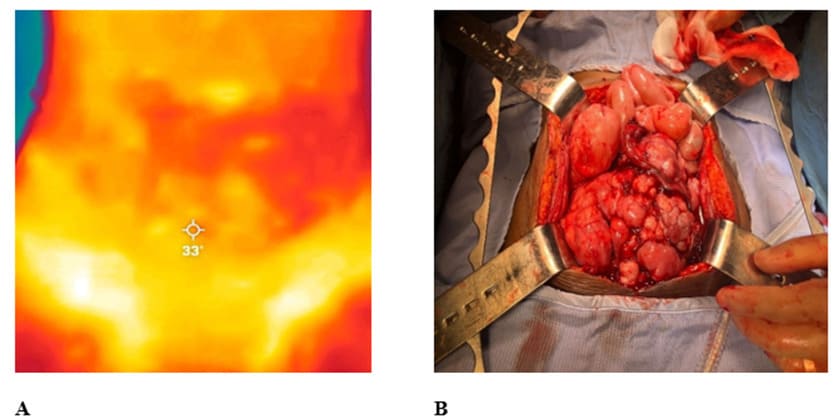
Figure 8: A case of leiomyosarcoma of the right broad ligament reaching above the umbilicus, with rectosigmoid adhesions on the left side of the mass. (A): Pre-operative Thermal image showing hot bright yellow areas in the umbilical and right iliac fossa corresponding to the right broad ligament leiomyosarcoma. The low temperature red colour corresponds to the sigmoid colon adhered to the left side of the mass. (B):Right sided broad ligament leiomyosarcoma with irregular surface after freeing the rectosigmoid from the left and superior aspect of the mass.
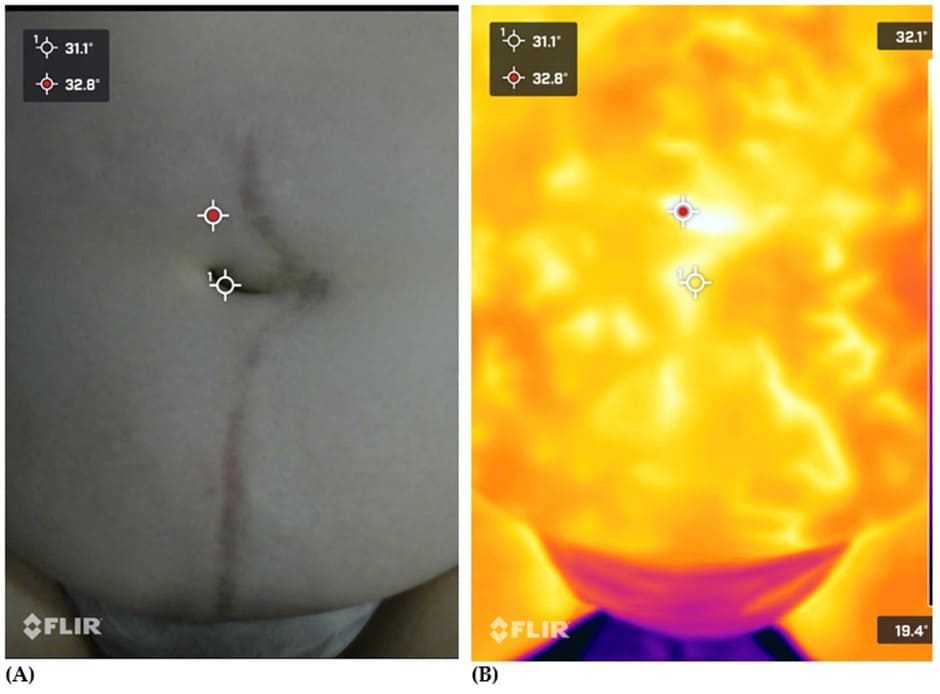
Figure 9: Example of small volume cancer disease in previous scar and paraumbiklical hernia sac. (A): Standard image with no thermal effect, cursors matching with thermal image. (B):Thermal image with hottest spot (red cursor) correlating to disease in hernia sac.
Discussion
As far as we are aware, our study is the first one aimed to assess the feasibility of utilizing thermal imaging to identify gynaecological tumors near the abdominal surface. With a 74% success rate in identifying malignancy deposits sites, our findings highlights the potential of thermal imaging to significantly enhance surgical outcome in gynaecological oncology. This may offer a promising technique for non-invasive pre-operative and intra-operative tumour mapping. This is particularly relevant when considering that thermology provides real-time data, which is less commonly achieved with traditional imaging modalities. In addition, the use of temperature differences rather than colour heterogeneity alone, introduces a novel aspect to thermal imaging analysis.
Similar to other studies in breast cancer, we faced the challenges of the impact of tumor depth and the thermal conductivity of surrounding tissues on temperature distribution [10]. However, the thermal imaging preoperative findings in our study were very sensitive to the detection of the tumour location when it was close to abdominal wall. This could be very helpful in planning of the surgical incision and avoiding cutting into the tumour on peritoneal incision. On a few occasions, a colour pattern has been identified and was correlated to bowel adhesions or obstruction to the anterior abdominal wall. This finding can be of great value to help reduce the risk of bowel injury in cancer surgeries, which can enhance patient safety. From the above, we think that the implications of our findings for clinical practice can be significant, as thermal imaging could serve as a valuable tool in the surgical planning process. This technology could thus contribute to more precise surgical margins, potentially reducing operative times and improving overall patient outcomes.
The lack of data about the thermal imaging technique for gynaecological malignancies posed a significant challenge before we can generate any clinical recommendations. The autor AS had to go through constructed training to be certified as thermalogist to be able to read the images. The limitations of this pilot study include its small sample size and the use of a single model of thermal imaging equipment, which may not fully represent the capabilities of more advanced technologies. The Flir One Pro smartphone thermal camera may lack the resolution and sensitivity of higher-end devices, potentially affecting the study's accuracy. These limitations emphasise the need for cautious interpretation of our findings.
To build on results of our pilot study, future research should focus on larger, randomized controlled trials that utilize more advanced thermal imaging technologies. Such studies could provide more definitive evidence of thermal imaging's effectiveness and its potential applications in gynecological oncology. Additionally, exploring how thermal imaging can be integrated with other diagnostic modalities may offer a more comprehensive approach to tumour characterization and surgical planning.
Conclusions
Our pilot study provides initial evidence that thermal imaging could play a role in enhancing surgical practice in gynecological oncology. Thermal cameras can be used for the surface mapping of various gynaecological tumours prior to surgical interventions. However, randomized controlled studies are needed to validate our findings.
Author Contributions:
Ahmad Sayasneh was instrumental in conceptualization, methodology, overseeing and leading the investigation, original draft preparation, and review and editing. Ahmed Abdelbar focused on data collection and contributed to writing and formal analysis, similar roles were held by Thushanee Ramajayan. Ahmad Sayasneh, Dhurgham Al-karawi and Shakir Al Zaidi contributed to the physical and technical background review of the thermology concept of the study. Moiad Alazzamacted as a national external reviewer of the study. Zelal Muallem acted as an international reviewer of the study. Validation efforts were jointly handled by the team. Visualization, supervision, project administration, and securing funding were led by Ahmad Sayasneh. All authors have reviewed and consented to the manuscript's final version.
Funding: This research received the Thermal camera as a loan from Medical Analytica Company (Medical Analytica Ltd, 52 Carlines Avenue, Ewloe, Flintshire, United Kingdom, CH5 3RQ).
Institutional Review Board Statement: This study was approved by the Clinical Governance Trust Board as a service evaluation project and was allocated an audit number 14592.
Informed Consent Statement: Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement: Data is available as Excel document attached as a supplementary file.
Acknowledgments: NA
Conflicts of Interest: The authors declare no conflict of interest
References
- Cancer Research UK (2023) Cancer Statistics for the UK.
- Rockall AG, Avril N, Lam R, Iannotti F, Vitola JV, et al. (2021) The role of CT, PET-CT, and MRI in ovarian cancer. Br J Radiol 94: 20210117.
- Ng EYK, Sudharsan NM (2001) An improved three-dimensional direct numerical modelling and thermal analysis of a female breast with tumour. Proc. Inst. Mech. Eng 215: 25-37.
- Tavakoli A, Ng EYK (2021) Early detection of breast cancer using infrared technology: A comprehensive review. Thermal Science and Engineering Progress 23: 101142.
- Infrared Training Centre (ITC).
- Teletherm Infrared Systems / Research.
- Berek JS, Renz M, Kehoe S, Kumar L, Friedlander M (2021) Cancer of the ovary, fallopian tube, and peritoneum: 2021 update. Int J Gynecol Obstet 155: 61-85.
- Höhn AK, Brambs CE, Hiller GGR, May D, Schmoeckel E, et al. (2021) 2020 WHO Classification of Female Genital Tumors. Geburtshilfe Frauenheilkd 81: 1145-1153.
- International Academy of Clinical Thermology. Thermography Guidelines.
- Hakim A, Awale RN (2020) Thermal Imaging - An Emerging Modality for Breast Cancer Detection: A Comprehensive Review. J. Med. Syst 44: 136.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.