There Is Still Place of Surgery in Metastatic Complete Response with Associated Immunotherapy in Renal Cell Carcinoma with Sarcomatoid Differentiation: A Case Report
by Dhihia Leghima1, Jihane Lehyanti2, Philippe De Sousa3, Michele Lamuraglia2,4*
1CHU Amiens Picardie, Oncology Unit, 1 Rue du Professor Christian Cabrol 80000 Amiens, France
2CHU Amiens Picardie, Internal Medecine Unit, 1 Rue du Professor Christian Cabrol 80000 Amiens, France
3CHU Amiens Picardie, Urology Unit, 1 Rue du Professor Christian Cabrol 80000 Amiens, France
4Sorbonne Université, CNRS, INSERM, Laboratoire d’Imagerie Biomédicale (LIB), 75006, Paris, France
*Corresponding author: Michele Lamuraglia, Laboratoire d’Imagerie Biomédicale (LIB), UMR 7371, UMR S 1146, Université Pierre et Marie Curie (PARIS VI), 15, rue de l’école de medecine (escalier A - 3° etage) – Paris, France
Received Date: 28 January 2025
Accepted Date: 31 January 2025
Published Date: 04 February 2025
Citation: Leghima D, Lehyanti J, De Sousa P, Lamuraglia M (2025). There Is Still Place of Surgery in Metastatic Complete Response with Associated Immunotherapy in Renal Cell Carcinoma with Sarcomatoid Differentiation: A Case Report. Ann Case Report. 10: 2180. https://doi.org/10.29011/2574-7754.102180
Introduction
Renal cell carcinoma (RCC) with sarcomatoid differentiation is one of the most aggressive forms of RCC, mainly due to its propensity for primary metastasis, relative resistance to systemic targeted therapies and poor prognosis with a median survival of 5-12 months [1]. The median age at diagnosis is 60 years. Most patients (90%) are symptomatic at diagnosis, predominantly with abdominal pain and hematuria, and often locally advanced or metastatic (45-77%). The treatment is based on a combination of maximal possible surgical resection combined with systemic therapy for metastatic disease [2]. Programmed death-ligand 1 (PD-L1) expression is increased in sarcomatoid dedifferentiated renal tumors, suggesting that patients with sarcomatoid RCC (sRCC) may benefit from Programmed Death 1 (PD1) and/or PDL1 immune checkpoint blockade therapy [3].
Keywords: Clear cell renal cell carcinoma (RCC); Sarcomatoid differentiation; Immunotherapy.
Case Presentation
In October 2019, a 27-year-old female patient, an unexpected and acute pain in the right hip bone. Radiographic imaging showed a lytic lesion of the right iliac wing. Blood test showed elevated CRP (C-reactive protein), LDH (Lactate dehydrogenase) and fibrinogen, thrombocytosis and inflammatory anemia. She works as a laboratory technician in the food industry, where she has been exposed to solvents but observed the necessary precautions. The clinical exam did not reveal neither ascites, nor hepatomegaly, or neurological signs. Computed tomography (CT) showed a large mass in the left kidney, secondary bone lesions (left clavicle, T12 and T5 vertebrae without a direct risk of compression and in the right iliac wing), an adjacent left adrenal lesion and at least six pulmonary nodules. (Figure 1A-C). Biopsy of the iliac lesion found a sarcomatoid carcinoma with a renal origin (Positive PAX 8 compatible with a clear cell renal cell carcinoma with a sarcomatoid differentiation (IMDC 4)). No TFE3 expression or loss of BAP1 expression, with loss of SDHB expression were reported (Figure 2).
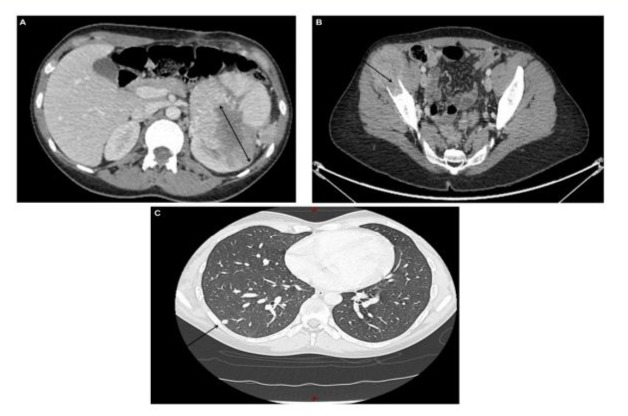
Figure 1: A CT total body base line revealed a primary renal lesion measuring 10 cm (A), a lytic lesion of the right iliac wing (B) and multiple pulmonary nodules (C).
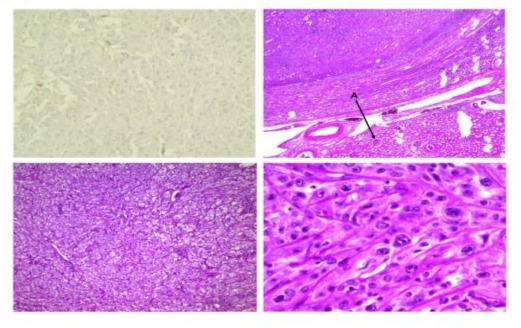
Figure 2: Histopathology of sRCC. No expression of the anti-SDHB antibody by tumor cells. Tumoral proliferation with diffuse architecture, eosinophilic cytoplasm, with atypical nuclei.
Seven months later, the patient received a first line of treatment with NIVOLUMAB/IPILILUMAB and had a favorable clinical and biological response. CT showed a stable disease according to RECIST 1.1 guideline (-24%) after 4 cycles of immunotherapy (Figure 3A-C). Treatment protocol was followed by NIVOLUMAB (480 mg every 4 weeks) as a maintenance therapy.
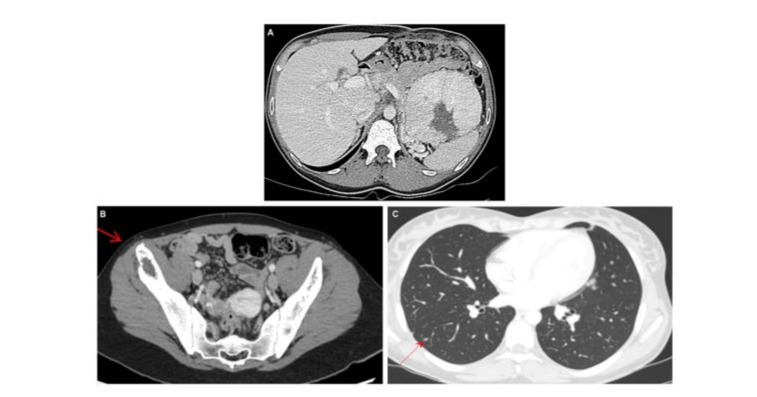
Figure 3: Evaluation after 4 cycles of treatment by NIVOLUMAB/IPILILUMAB. CT evidence shows a partial responding disease using the RECIST 1.1 guidelines (-24%), with stability of primary renal lesion measuring 10 cm (A), but reduction of lytic lesion of the right iliac wing (B) and reduction of since and numbers of multiple pulmonary nodules (C).
A clinical evaluation performed in December 2020, after 6 cycles of maintenance by NIVOLUMAB, found a completed clinical response. CT showed a completed regression of all metastatic lesions, but a discrete increase of the renal mass (from 87 mm to 97 mm). The patient was in excellent general conditions (ECOG=0), and was asymptomatic. Two months later, the patient underwent a large complete left nephrectomy (Figure 4). Histology analysis confirmed the sarcomatoid differentiation of the RCC measuring 11 cm with hilar vascular invasions. In September 2022, after 1 years ET 9 months before nephrectomy and after 21 cycles of postoperative maintenance therapy with NIVOLUMAB (a total dose of 10080 mg), no clinical and biological progression was detected. Furthermore, the patient still had a complete response (RECIST criteria), indicating an excellent quality of life. In January 2023, the patient presented back pain. Unfortunately, CT confirmed progression with the emergence of multiple liver and bone lesions. A second line with CABOZANTINIB was started without much benefit, before radiotherapy of bone metastases.

Figure 4: Large left nephrectomy, 11cm renal mass with hilar vascular invasions.
Discussion
Sarcomatoid differentiation is a rare transformation that can occurs in most RCC histological subtypes. Patients with this subtype have a worse survival at any stage of the disease. When diagnosed at an early stage, surgical intervention remains the treatment of reference, although recurrence is frequent [3].
RCC is a tumor characterized by an increased angiogenesis (due to loss of VHL tumor suppressor). Clinical benefits in patients with advanced RCC have been observed in multiple trials with protocols involving different combinations of immune and/or angiogenesis inhibitors in patients with untreated intermediate- and low-risk advanced RCC [4].
The phase III trial CHECKMATE-9ER demonstrated significant benefits in progression-free survival (PFS) and overall survival (OS) with Nivolumab/Cabozantinib compared to Sunitinib (4). In addition, the Phase III KEYNOTE-426 trial found significantly higher OS and PFS with Pembrolizumab/Axitinib compared to sunitinib in treatment-naïve advanced RCC (5). The CHECKMATE-214 trial highlighted a significant increase in OS with the combination of Nivolumab and Ipilimulab compared to Sunitinib (6). This double immunotherapy continues to demonstrate sustained efficacy benefits and manageable safety at 4-year of follow-up (7).
In this case report we observed that immunotherapies treatments can drastically improve objective response rate in a high-risk patient with a poor prognosis. El Mouallem et al, in a similar case report of 67-year-old patient with sarcomatoid cRCC, achieved a complete response after 6 months of Nivolumab in second line (Sunitinib in the first line). Nivolumab was continued for a total of 2 years without evidence of recurrence, before being stopped [5].
Moreover, our case reported that cytoreductive nephrectomy should also be considered in patients with disease with unfavorable prognostic parameters to increase the likelihood of successful immunotherapy (9).
In conclusion, due to the paucity of prospective data, defining the role of cytoreductive nephrectomy in the era of immunotherapy remains controversial.
References
- Othmane Y, Mounir L, Tarik K, Khalid E, Abdellatif K, et al. (2015). Chromophobe renal cell carcinoma: report of four cases and review of the literature. Pan Afr Med J. 22: 123.
- Arnoux V, Lechevallier E, Pamela A, Long JA, Rambeaud JJ. (2013). Carcinomes rénaux à contingent sarcomatoïde. Progrès en Urologie. 23: 430-437.
- Blum KA, Gupta S, Tickoo SK, Chan TA, Russo P, et al. (2020). Sarcomatoid Renal Cell Carcinoma: Biology, Natural History and Management. Nat Rev Urol. 17: 659-678.
- Choueiri TK, Powles T, Burotto M, Escudier B, Bourlon MT, et al. (2021). Nivolumab plus Cabozantinib versus Sunitinib for Advanced Renal-Cell Carcinoma. N Engl J Med. 384: 829-841.
- El Mouallem N, Smith SC, Paul AK. (2018). Complete Response of a Patient with Metastatic Sarcomatoid Renal Cell Carcinoma to a Programmed Death-1 Checkpoint Inhibitor. JOP. 14: 511-513.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.