The Utilization of Human Placental Mesenchymal Stem Cell Derived Exosomes in Aging Skin: An Investigational Pilot Study
Greg Chernoff* BSc, MD, FRCSC
Greg Chernoff, Department of Surgery, Ascension Saint Vincent Hospital, Private Practice, 9002 N Meridian Street, Suite 205, Indianapolis, Indiana, 46260, USA
*Corresponding author: Greg Chernoff, BSc, MD, FRCSC; Department of Surgery, Ascension Saint Vincent Hospital, Private Practice, 9002 N Meridian Street, Suite 205, Indianapolis, Indiana, 46260, USA
Received Date: 05 April, 2021; Accepted Date: 12 April, 2021; Published Date: 15 April, 2021,
Citation: Chernoff G (2021) The Utilization of Human Placental Mesenchymal Stem Cell Derived Exosomes in Aging Skin: An Investigational Pilot Study. J Surg 6: 1388. DOI: 10.29011/2575-9760.001388
Abstract
Introduction: The fields of cellular medicine, regenerative and stem cell therapy continue to grow, yielding many novel therapies in aesthetic and reconstructive surgery. Human placental mesenchymal stem cell - derived extracellular vesicles, or exosomes have been utilized in many degenerative, inflammatory, and autoimmune conditions involving the musculoskeletal system. Exosomes are 50-15- nm particles, rich in cytokines, messenger RNA, microRNA, and transmembrane proteins from their parent cells. They are produced by cells as a means of intercellular communication, and via a natural paracrine signaling system participate in normal bodily function. With proper homing, exosomes can illicit regenerative, ant-inflammatory, immunomodulatory, and anti-prostaglandin events. This study examines the safety and potential benefits of topically applied exosomes on aging skin.
Materials and Methods: Forty patients were enrolled in a randomized, double-blinded, placebo (saline) controlled study. There were 20 patients in the treatment group and 20 patients in the saline control group. Each group underwent facial micro needling with immediate topical application of either 5 billion exosomes suspended in saline, or saline alone. Treatments were repeated at 30, 60, and 90 days, with final analysis at 120 days. Standardized photography was coupled with 3-dimentional analysis utilizing the Quantificare Imaging System (Quantificare, USA). Linear analog tests were also administered to objectify patient satisfaction.
Results: There were no adverse reactions, allergic, or hypersensitivity reactions reported. The Exosome Treatment Group showed improved tone, quality, and clarity of their skin compared to the Control Group (p < .0001), with a reduction in wrinkles, pores, pigment, oiliness, and improvement in evenness of skin and vascularity. There was a constant progression of satisfaction with results in the Treatment Group from 30 to 120 days, compared with a high degree of dissatisfaction with results in the Control Group.
Conclusion: Human placental mesenchymal stem cell-derived exosomes can be safely applied topically to patients with aging skin. Exosomes are a viable addition to the armamentarium of the physician treating aging skin and associated dermatopathological conditions.
Introduction
The fields of cellular medicine, regenerative and stem cell therapies continue to grow exponentially, particularly as it relates to therapeutics and diagnostics [1]. Early cutaneous applications of cellular medicine saw success with human dermal-derived, tissue cultured, autologous injectable fibroblasts [2]. The next advancement in autologous regenerative therapy surrounded Stromal Vascular Fraction (SVF) procured from adipose tissue lipoaspirate via a near closed specialized sterile surgical processing system [3]. In this study, Berman and Lander performed a prospective, multi-center safety study on 1698 SVF deployment procedures on 1524 patients with various degenerative, inflammatory, and autoimmune conditions involving the musculoskeletal system. Their study showed both safety and efficacy with a low number of reported adverse events, and a high rate of pain mitigation and improvements in a variety of degenerative conditions. This study opened the door to a promising new era in autologous personalized cell therapy [4]. Further study was then carried out examining the efficacy of SVF in treating aging skin, acne, wound healing and other autoimmune, inflammatory and degenerative conditions involving the skin [5].
The mechanism of action of mesenchymal stem cells in regeneration remains under study [6]. Early hypotheses speculated engraftment and trans-differentiation with creation of new cells to effect repair. In 2006, Caplan described MSC’s as “medicinal signaling cells” capable of releasing paracrine effectors which influence the body via immunomodulatory and trophic mechanisms [7]. These bioactive messengers can upregulate resident stem cells, which reside throughout all tissues of our bodies, and affect the phenotypic and physiologic expression of our immune system. MSC’s are in constant communication through biologic signaling with surrounding cells and contain a feedback loop involving their own cell membranes. This complex signaling system allows stem cells to induce healing of damaged target cells within proximity without engraftment. This cellular communication is affected by messengers termed exosomes and microvesicles, collectively known as Extracellular Vesicles (EV’s).
Exosomes measure 50 -150 nm and are lipid membrane packets formed by a two-step budding process. First formed by inward budding of membranous vesicles in a multivesicular body, they fuse with the plasma membrane to release exosomes. Microvesicles are larger packets formed by direct budding of the plasma membrane. Both contain transmembrane proteins from their parent cells which aid in regulating uptake by other cells [8]. Exosomes contain messenger RNA (mRNA), microRNA (miRNA), and a multitude of proteins consisting of growth factors (Table 1) and immune factors (Table 2). When properly stimulated, they illicit homing, regenerative, anti-inflammatory, immunomodulatory and anti-prostaglandin mechanisms. Extracellular vesicles travel systemically without the risk of clumping. They do not demonstrate a first-pass effect into the lungs when administered intravenously as is commonly seen with MSC’s. EV’s can cross the blood-brain barrier without using mannitol [8]. Exosomes are able to evade the immune response as they contain no DNA, yielding no risk for malignant transformation.
An increasing number of younger and older patients are presenting for consultation in aesthetic offices. Within this patient population exists a desire for minimally invasive, non-surgical procedures seeking preventative aesthetic solutions to prolong the necessity for future corrective aesthetic therapies. This trend has fueled the current explosion in the expanding knowledge and study of placental mesenchymal stem cell-derived vesicles or exosomes [1]. Mesenchymal Stem Cell Exosomes, (MSC exosomes) are produced by stem cells of connective tissue lineage which is the origin of skin, hair, bone, muscle and cartilage. MSC exosomes are different from adult bone marrow exosomes which has a preponderance of hematopoietic stem cell exosomes. Another source of exosomes is derived from amniotic fluid. These are composed of primarily maternal epithelial cell exosomes. It is hypothesized that the ability of MSC exosomes to induce the synthesis of connective tissue is the basis for remarkable clinical benefits resulting from stem cell therapy [7]. The advantage of perinatal MSC exosomes over exosomes from aged autologous or allogenic progenitor cells resides in the fact that with age, the number and function of MSC’s in our tissue declines. Aged autologous progenitor cells also produce less than 40% of the cytokines and differing miRNA’s than perinatal MSC’s. This secretome advantage of younger exosomes is therefore significant. This study examines the potential benefit of human c-section donated, cultured fetal stem cell-derived exosomes in the treatment of aging skin.
Methods
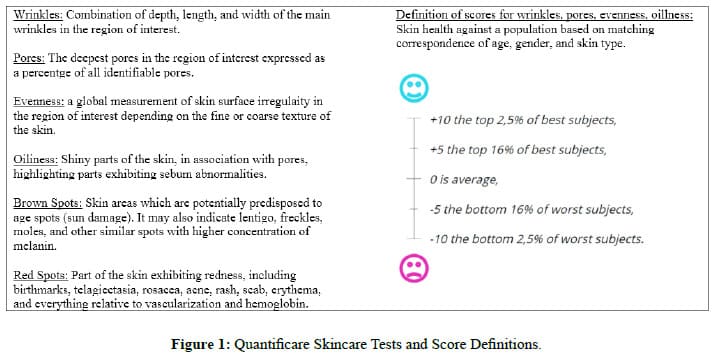
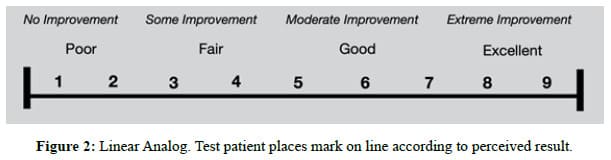
To determine the safety and efficacy of topically applied Mesenchymal Stem Cell Derived Exosomes on aging skin, 40 patients were enrolled. There were 30 females and 10 males. Ages ranged from 32 years to 76 years. There were 22 Caucasian, 6 Hispanic, 4 Asian, 4 African American, 3 Mediterranean, and 1 Indian patient. The patients were enrolled in a randomized, doubleblind, placebo (saline) controlled regimen. There were 20 patients in the Treatment Group and 20 patients in the Control Group. Each group underwent a combination of microdermabrasion (Rejuvapen, USA) followed by immediate topical application of either 5.0 ml (5 billion) Exosomes (Kimera Labs, USA) or 5.0 ml of 0.9% sterile saline (Placebo). Treatments were repeated at 30, 60 and 90 days with final analysis at 120 days. Pre-treatment and post-treatment standard photography was coupled with 3-dimentional analysis utilizing the Quantificare Imaging System (Quantificare, USA), (Figure 1). Linear analog scales (Figure 2), were administered to each patient to objectify patient satisfaction with the treatment. The Exosomes utilized (Kimera Labs, USA) were a suspension of isolated and purified, c-section donated, placental, mesenchymal stem cell-derived extracellular vesicles suspended in a saline solution. The product is manufactured in two concentrations: standard and a 3X concentrate. Both products have been available for many years and have been proven to be safe, consistent, effective, and reproducible from Lot to Lot.
To ensure the safety of the finished vial product (FVP), donor eligibility is first established through review of medical records, social behavior, physical examination, and serological blood tests to verify the absence of relevant communicable diseases. Table 3 lists the Donor Safety Testing procedures. Once donor eligibility is deemed acceptable and released, the isolated Mesenchymal Stem Cells (MSC) are characterized to ensure identity and safety. Once the Master Cell Bank (MCB) has been fully characterized, and safety confirmed, then manufacturing of the FVP proceeds. Both manufacturing and all analytical testing of these Exosomes are performed under strict cGMP guidelines and regulations as per 21 CRF210, 211, as well as GLP HCT/P Regulations and Guidance as per 21 CFR 1271. There are numerous controls throughout the process. The manufacturing suites are qualified to ISO 7 compliant airflow standards, and the LFGI’s used for the manufacturing downstream process are ISO 5 certified units. Routine environmental monitoring, as well as aseptic monitoring are performed in the room, as well as in all LFGI units before, during, and after the manufacturing process takes place. This strict monitoring ensures that no contamination is introduced to the product. Once the FVP is completed, additional testing is performed to ensure the quality, purity, identity, safety, biological activity, and strength of the product. Table 4 lists the testing performed on either the Finished Bulk Product (FBP) or the FVP.
Results
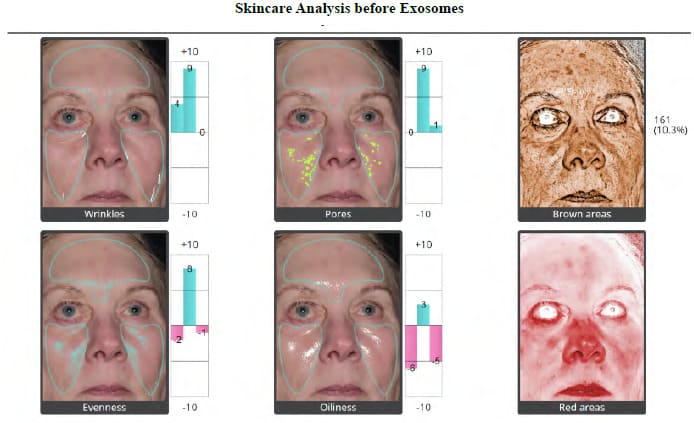
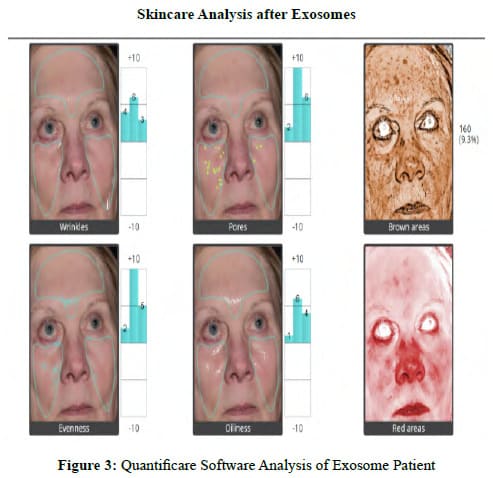
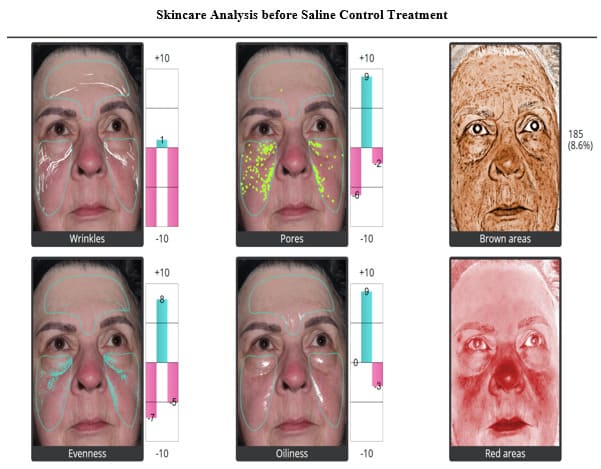
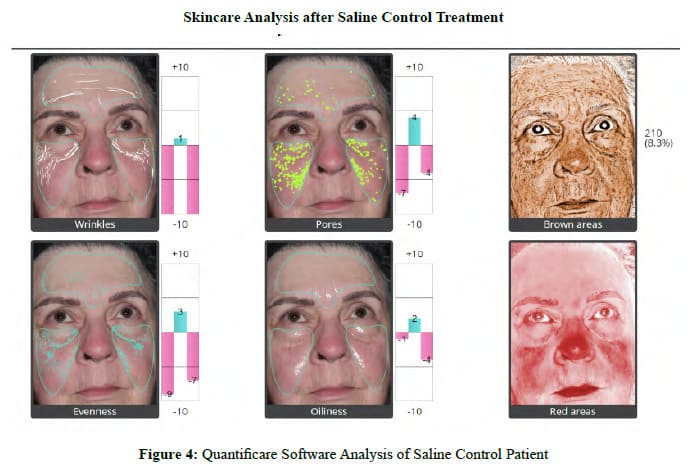
There were no allergic reactions, hypersensitivity reactions, or adverse events in either the Treatment Group or the Control Group. No patients were lost to follow-up in either Group. Patient satisfaction with cosmetic results is an important measure of procedure efficacy. Each patient completed a linear analog scale at 30, 60, 90, and 120 days (Figure 2). Placing a mark on a 10 cm line provides an objective, numerical endpoint of a subjective impression of results which can then be subjected to statistical analysis. Table 5 summarizes the Patient Satisfaction Linear Analog results for the Exosome Group. Table 6 summarizes the Patient Satisfaction Linear Analog results for the Saline Control Group. No patient reported being unhappy with the Exosome results from Day 30 through Day 120, whereas 35% of the Control Group were unhappy with the results at 30 days, 45% at 60 days, 55 % at 90 days and 40 % were unhappy by 120 days. There was a constant progression of satisfaction with results in the Exosome Group from 30 to 120 days with 75% of the population being “Extremely Happy” with the end result and 25% of the population being “Very Satisfied” with the results at 120 days. In the Control Group, no patient was “Extremely Satisfied” at 120 days (p< .0001). Figure 3 shows the 3-dimentional Quantificare analysis of an Exosome Patient before treatment and at 120 days. Uniformly, the Exosome patients exhibited improved tone, quality and clarity of their skin with a reduction in fine lines, pores, pigment, oiliness, and an improvement in texture and vascularity. Figure 4 shows the 3-dimentional Quantificare analysis of a Control patient before treatment and at 120 days. Uniformly the Control Group showed little improvement in tone, quality, texture and clarity of their skin.
Discussion
Much has been written on the role of endogenous exosomes in cutaneous biology and dermatologic disease [9-36]. Studies have demonstrated the key function that keratinocytes play in secreting exosomes that orchestrate many of the protective and regenerative capabilities of the epidermis and dermis [9-12]. Few studies have examined the therapeutic benefits of MSC EV’s in treating aging skin and the many problems associated with aging such as loss of elasticity, reduced collagen synthesis and function, pigmentary changes and dysplasia leading to cutaneous carcinomas. MSC exosomes have several therapeutic effects on the skin. They are able to stimulate fibroblast proliferation and migration [21], increase collagen extracellular matrix production and deposition [13], promote angiogenesis in acute and chronic wounds [23,27,28], modulate inflammation and the immune response [16], and regulate tissue remodeling to reduce adverse scarring [25]. MSC exosomes are also able to increase the number of hair follicles in the anagen or growth phase and regenerate the dermal papilla cells within the hair follicle [17]. The exosome’s trophic or regenerative and immunomodulatory capabilities are central in understanding their benefit when treating aging skin. Creating an “Inflammatory Homing Milleu” (IHM) by performing microdermabrasion, micro-needling, needle-radiofrequency, fractionated or exfoliative carbon dioxide (CO2) laser treatments prior to topical exosome application, creates the inflammatory trigger for the exosomes to initiate the “healing” or rejuvenating response. The added benefit of applying topical exosomes is their anti-inflammatory and antiprostaglandin properties which reduce post-procedure erythema and any associated discomfort. The exosomes are also acting on the cutaneous resident stem cells which are partially undifferentiated and once activated can proliferate and migrate to sites of injury where they acquire a mature phenotype to facilitate repair and remodeling. This accounts for the neo-collagenesis visible in the Grenz Zone when examining rejuvenated cutaneous tissue.
The immunomodulatory effects of exosomes relate to their ability to influence the expression of specific cells. M1 macrophages are pro-inflammatory and secrete inflammatory cytokines. M2 macrophages are considered anti-inflammatory. MSC exosomes influence the conversion of M1 macrophages into M2 macrophages [36-39]. Additionally, MSC exosomes convert T Helper1 cells (inflammatory) to T Helper2 cells (aniinflammatory) and increase T Regulatory cells. These phenotypic changes and the production of anti-inflammatory cytokines like IL-10, TGF-beta3, TIMP, TNFalphaRA, and IL-IRA further provide for the anti-inflammatory and immunomodulatory effects seen after MSC exosome administration. The ant-fibrotic benefits of MSC exosomes revolve around the production of TGF-beta3, which regulates cell adhesion and extracellular matrix formation. Exosomes also regulate the ratio of collagen Type III to Type I facilitating normal healing. They also promote scarless cutaneous repair by regulating extracellular matrix remodeling via inhibiting granulation tissue. This results in more organized fine reticular collagen [40]. Subsequent to injury, cells lose ATP/ADH and experience oxidative stress, and produce reactive oxygen and nitrogen molecules resulting in death. MSC exosomes contain the 5 enzymes involved in the ATP-generating stage of glycolysis, namely, GAPDH, PGK, PGM, ENO, and PKM2 [41]. This antiapoptotic effect on mitochondria underscores the exosome’s ability to ameliorate the damaging effects of inflammation and ischemia on living cells. With the hallmark of aging surrounding the decline of regenerative properties yielding impaired function of progenitor cells, further studies examining the role of MSC exosomes in treating aging skin pathology are warranted.
Conclusion
Human placental mesenchymal stem cell-derived exosomes are a valuable addition to the armamentarium of the physician treating aging skin and associated dermatopathology.
|
BMP5 |
Stimulates Bone Growth |
|
GDF15 |
Regulates inflammation, apoptosis, cell repair, and growth |
|
OPG |
Stimulates Bone Growth/Blocks Osteoclast Precursor Formation |
|
G-CSF |
Stimulates Bone Marrow to Procedure Granulocytes and Stem Cells |
|
SCF |
Responsible for Stem Cell and Melanocyte Growth |
|
TGFß3 |
Most Important Anti-Inflammatory Protein. Converts Inflammatory T Cells into Anti-Inflammatory Regulatory T Cells. |
|
VEGF |
Stimulates Formation of Blood Vessels |
|
ICAM-1 |
Binds Inflammatory Ligands on White Cells |
|
IL-1RA |
Binds and Sequesters the Inflammatory Cytokine IL-1 |
|
IL-6 |
Responsible for Macrophage Activation |
|
IL-10 |
Anti-Inflammatory Cytokine responsible for Immunomodulation and Regulatory T Cell Conversion |
|
MCP-1 |
Recruits Mononuclear Cells to Treatment Area |
|
MIP-1 |
Also known as CC1-4, Recruits Mononuclear Cells to the Treatment Area |
|
PDGF-BB |
Growth Factor Used to Stimulate Healing in Soft and Hard Tissues |
|
TIMP1 & TIMP2 |
Blocks Cartilage and Extracellular Matrix Degradation, Important for Cartilage Repair |
|
HGF |
Involved in Organ Regeneration and Wound Healing |
|
GDNF |
Promotes Survival of Neurons |
|
BDNF |
Supports Survival of Neurons and Encourage Growth |
|
FGF |
Potent Growth Factors Affecting Many Cells |
|
TNFR1 |
Binds and Inactivates the Inflammatory cytokine TNF-a |
|
IL-1RA TIMP1 & TIMP2 TNFR1 and TNFR2 Numerous Histone Deacetylase mRNAs GDF11 - Potent anti-aging agent GDF15 - Regulates inflammation IGFBP2 - One of six IGF binding proteins that bind IGF-1 and IGF-2 IGFBP3 IGFBP4 - Reportedly anti-tumorigenic effects against prostate cancer, colon cancer, and glioblastoma IGFBP6 OPG SCFR TGF-ß1 & TGF-ß3 VEGF VEGFR-2 BMP4 - Involved in bone and cartilage development, fracture repair, and muscle development BMP7 - Important in bone homeostasis PTEN - A potent tumor suppressor gene Numerous Key miRNA |
|
CMV IgM (EIA) Biorad |
Hepatitis B Surface Ab |
Syphilis Screening Nontreponemal |
WNV |
|
CMV IgG (EIA) Biorad |
Hepatitis C Virus Ab |
Ultrio Elite HBV |
ZIKA Virus |
|
CMV Total Ab |
HIV-1/HIV-2 Plus O |
Ultrio Elite HCV |
JCV PCR |
|
Hepatitis B Core Total Ab |
HTLV I/II AB |
Ultrio Elite HIV-1/2 |
COVID-19 |
|
Quality Attribute |
Test |
|
Quality |
· Appearance · Size · rtPCR |
|
Strength |
· Protein Concentration by A280nm · RNA Extraction |
|
Purity |
· SEC-HPLC · SDS-PAGE non-reduced Coomassie Blue Stained · RNA Extraction |
|
Identity |
· Western Blot for specific surface markers · ONI Imaging for specific surface markers · RRT by SEC-HPLC |
|
Safety |
· Mycoplasma · Bacterial Endotoxin · Sterility by Direct Inoculation · Patriciate Matter in Injections by Light Obstruction Method by USP <788> for Therapeutic Protein Injections |
|
Biological Activity |
· Cell-Based ELISA Potency Assay · rtPCR |
|
Percent |
||||
|
Satisfaction: Exosomes |
30 Days |
60 Days |
90 Days |
120 Days |
|
Dissatisfied |
0 |
0 |
0 |
0 |
|
Satisfied |
80 |
55 |
15 |
0 |
|
Very Satisfied |
20 |
20 |
30 |
25 |
|
Extremely Satisfied |
0 |
25 |
55 |
75 |
|
Percent |
||||
|
Satisfaction: Exosomes |
30 Days |
60 Days |
90 Days |
120 Days |
|
Dissatisfied |
35 |
45 |
55 |
40 |
|
Satisfied |
65 |
55 |
35 |
45 |
|
Very Satisfied |
0 |
0 |
10 |
15 |
|
Extremely Satisfied |
0 |
0 |
0 |
0 |
References
- Jeffrey D. McBride, Divya Aickara, Evangelos Badiavas (2020) Exosomes in cutaneous biology and dermatologic disease. Exosomes, A Compendium. Editor(s): Lawrence Edelstein, John Smythies, Peter Quesenberry, Denis Noble. Academic Press 2020: 239-255.
- Chernoff, W. Gregory, Boss William (2000) Autologous Cultured Fibroblasts as Cellular Therapy in Plastic Surgery. Found in Clinics in Plastic Surgery 27: 613-626.
- Berman, Lander (2018) A Prospective Safety Study of Autologous Adipose-Derived Stromal Vascular Fraction Using a Specialized Surgical Processing System. The American Journal of Cosmetic Surgery 2018: 1-14.
- Lander, Berman (2018) Autologous Stromal Vascular Fraction: A New Era of Personal Cell Therapy. J Stem Cell Res Dev Ther 4: 011.
- Chernoff, Greg, Bryan, Nathan, et al. (2018) Mesothelial Stem Cells and Stromal Vascular Fraction: Use in Functional Disorders, Wound Healing, Fat Transfer, and Other Conditions. p487-501. Facial Plastic Surgery Clinics 26: p403-532.
- Gnecchi M, Danieli P, Malpasso G, Ciufferda MC, et al. (2016) Paracine Mechanisms of Mesenchymal Stem Cells in Tissue Repair Methods Mol Biol 1416: 123-146.
- Caplan AI, Dennis JE (2006) Mesenchymal stem cells as trophic mediators. J Cell Biochem 98: 1076-1084.
- Rashed MH, Bayrakar E, Helal GK, et al. (2017) Exosomes: From Garbage Bins to Promising Therapeutic Targets. International Journal of Molecular Sciences 18: 538.
- Lo Cicero A, et al. (2015) Exosomes released by keratinocytes modulate melanocyte pigmentation. Nat Commun 6: 7506.
- Waster P, et al. (2016) Extracellular vesicles are transferred from melanocytes to keratinocytes after UVA irradiation. Sci Rep 6: 27890.
- Bin BH, et al. (2016) Fibronectin-containing extracellular vesicles protect melanocytes against ultra- violet radiation-induced cytotoxicity. J Invest Dermatol 136: 957-966.
- Chavez-Munoz C, et al. (2008) Primary human keratinocytes externalize stratifin protein via exo- somes. J Cell Biochem 104: 2165-2173.
- Medina A, Ghahary A (2010) Transdifferentiated circulating monocytes release exosomes contain- ing 14-3-3 proteins with matrix metalloproteinase-1 stimulating effect for dermal fibroblasts. Wound Repair Regen 18: 245-253.
- Cai XW, et al. (2017) A novel noncontact communication between human keratinocytes and T cells: exosomes derived from keratinocytes support superantigen-induced proliferation of resting T cells. Mol Med Rep 16: 7032-7038.
- Nickoloff BJ, et al. (1993) Accessory cell function of keratinocytes for superantigens. Dependence on lymphocyte function-associated antigen-1/intercellular adhesion molecule-1 interaction. J Immunol 150: 2148-2159.
- Kotzerke K, et al. (2013) Immunostimulatory activity of murine keratinocyte-derived exosomes. Exp Dermatol 22: 650-655.
- Zhou L, et al. (2018) Regulation of hair follicle development by exosomes derived from dermal pa- pilla cells. Biochem Biophys Res Commun 500: 325-332.
- Nakamura K, et al. (2016) Altered expression of CD63 and exosomes in scleroderma dermal fibro- blasts. J Dermatol Sci 84: 30-39.
- CheungKL,et al. (2016) PsoriaticTcellsrecognizeneolipidantigensgeneratedbymastcellphospho- lipase delivered by exosomes and presented by CD1a. J Exp Med 213: 2399-2412.
- Fang H, et al. (2018) Proinflammatory role of blister fluid-derived exosomes in bullous pemphigoid. J Pathol 245: 114-125.
- Hu L, et al. (2016) Exosomes derived from human adipose mensenchymal stem cells accelerates cuta- neous wound healing via optimizing the characteristics of fibroblasts. Sci Rep 6: 32993.
- Shabbir A, et al. (2015) Mesenchymal stem cell exosomes induce proliferation and migration of normal and chronic wound fibroblasts, and enhance angiogenesis in vitro. Stem Cells Dev 24: 1635-1647.
- McBride JD, et al. (2017) Bone marrow mesenchymal stem cell-derived CD63(+) exosomes trans- port Wnt3a exteriorly and enhance dermal fibroblast proliferation, migration, and angiogen- esis in vitro. Stem Cells Dev 26: 1384-1398.
- McBride JD, et al. (2018) Dual mechanism of type VII collagen transfer by bone marrow mesenchy- mal stem cell extracellular vesicles to recessive dystrophic epidermolysis bullosa fibroblasts. Biochimie 155: 50-58.
- Fang S, et al. (2016) Umbilical cord-derived mesenchymal stem cell-derived exosomal microRNAs suppress myofibroblast differentiation by inhibiting the transforming growth factor-beta/ SMAD2 pathway during wound healing. Stem Cells Transl Med 5: 1425-1439.
- Zhang B, et al. (2016) HucMSC exosome-delivered14-3-3zetaorchestratesself-controloftheWntre- sponse via modulation of YAP during cutaneous regeneration. Stem Cells 34: 2485-2500.
- Liang X, et al. (2016) Exosomes secreted by mesenchymal stem cells promote endothelial cell angio-genesis by transferring miR-125a. J Cell Sci 129: 2182-2189.
- Bronckaers A, et al. (2014) Mesenchymal stem/stromal cells as a pharmacological and therapeutic approach to accelerate angiogenesis. Pharmacol Ther 143: 181-196.
- Overmiller AM, et al. (2017) Desmoglein 2 modulates extracellular vesicle release from squamous cell carcinoma keratinocytes. FASEB J 31: 3412-3424.
- Hatanaka M, et al. (2014) Cleaved CD147 shed from the surface of malignant melanoma cells activates MMP2 produced by fibroblasts. Anticancer Res 34: 7091-7096.
- Pfeffer SR, et al. (2015) Detection of exosomal miRNAs in the plasma of melanoma patients. J Clin Med 4: 2012-2027.
- Plebanek MP, et al. (2017) Pre-metastatic cancer exosomes induce immune surveillance by patrolling monocytes at the metastatic niche. Nat Commun 8: 1319.
- Languino LR, et al. (2016) Exosome-mediated transfer from the tumor microenvironment increases TGFbeta signaling in squamous cell carcinoma. Am J Transl Res 8: 2432-2437.
- Sun Y, et al. (2018) Extracellular vesicles as biomarkers for the detection of a tumor marker gene in epidermolysis bullosa-associated squamous cell carcinoma. J Invest Dermatol 138: 1197-1200.
- Peinado H, et al. (2012) Melanoma exosomes educate bone marrow progenitor cells toward a prometastatic phenotype through MET. Nat Med 18: 883-891.
- Cheng Z, HE X (2017) Anti-inflammatory effect of stem cells against spinal cord injury via regulating macrophage polarization. Journal of Neurorestoratology 5: 31-38.
- Lankford KL, Arroyo EJ, Nazimek K, et al. (2018) Intravenously delivered mesenchymal stem cell-derived exosomes target M2-type macrophages in the inured spinal cord. Plas One 2018: 13.
- Zhang S, Chuah SJ, Lai RC, et al. (2018) MSC exosomes mediate cartilage repair by enhancing proliferation, attenuating apoptosis and modulating immune reactivity. Biomaterials 156: 16-27.
- Ruppert KA, Nguyen TT, Prabhakra KS, et al. (2018) Human Mesenchymal Stromal Cell Derived Extracellular Vesicles Modify Microglial Response and Improve Clinical Outcomes in Experimental Spinal Cord Injury. Scientific Reports 8.
- Wang L. Hu L, Zhou X, et al. (2017) Exosomes secreted by human adipose mesenchymal stem cells promote scarless cutaneous repair by regulating extracellular matrix remodeling. Scientific Reports
- Arslan F, Lai RC, Smetts, MB et al. (2013) Mesenchymal stem cell-derived exosomes increase ATP levels, decrease oxidative stress and activate P13K/Akt pathway to enhance myocardial viability and present adverse remodeling after myocardial ischemia/reperfusion injury. Stem Cell Res 10: 301-312.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.