The Use of a Novel Desiccating Agent as a Adjuvant Therapy to Surgical Debridement in the Infected Diabetic Foot: A Case Series
by H. Erhan Güven1, Leandro Tapia Garcia2, Thomas Serena2*
1Department of General Surgery, University of Health Sciences, Ankara Etlik City Hospital,; Diabetic Foot and Chronic Wounds, Ankara, Turkey
2SerenaGroup® 125 Cambridge Park Dr. Cambridge, MA, USA
*Corresponding author: Thomas Serena, SerenaGroup® 125 Cambridge Park Dr. Cambridge, MA, USA
Received Date: 05 June 2024
Accepted Date: 10 June 2024
Published Date: 12 June 2024
Citation: Güven HE, Garcia LT, Serena T (2024) The Use of a Novel Desiccating Agent as a Adjuvant Therapy to Surgical Debridement in the Infected Diabetic Foot: A Case Series. J Surg 9: 11070 https://doi.org/10.29011/2575-9760.11070
Abstract
A common complication of diabetes, diabetic foot infections, can lead to devastating complications. Early antibiotic and surgical treatment are key to preserving the affected limb. Emergent surgical intervention is the mainstay of therapy; however, despite aggressive surgical debridement, some patients still go onto lower extremity amputation. Amputation in diabetics has a prognosis worse than the most common cancers. The need for advanced therapies in the treatment of the infected diabetic foot remains an unmet need. This case series reviewed the use of a novel Topical Desiccating Agent (TDA), containing methanesulfonic acid, in combination with surgical debridement and antibiotics in the treatment of severe diabetic foot infections. Research suggests that the addition of a TDA facilitates debridement and disrupts both planktonic and biofilm-based bacteria promoting healing and decreasing the time to definitive reconstruction. A total of eleven patients were treated with the novel TDA. It was applied in the operating room at the time of the initial surgical intervention. Two cases are presented in detail. Overall, there appeared to be a more complete debridement and more rapid time to grafting with the addition of the desiccant. Further research into the role of TDAs in the treatment of the infected diabetic foot is warranted.
Keywords: Chemical debridement; Desiccating agent; Diabetic foot infection; Diabetic foot ulcer; Debridement; Necrotizing infection
Introduction
The World Health Organization defines Diabetic Foot Syndrome (DFS) as an ulceration of the foot associated with infection, neuropathy, and ischemia [1]. Threatening limb and life, DFS, is one of the most serious complications of diabetes [2]. Rapidly spreading infection in the diabetic foot can lead to extensive tissue destruction necessitating amputation. Prompt diagnosis and intervention reduces the risk of complications including amputation, sepsis, and death [3]. In addition to antibiotic therapy, surgery to remove necrotic material, including the fascial tissue, and drain pockets of purulence is the mainstay of treatment [4]. In most cases, the initial procedure for the severely infected diabetic foot does not remove all the nonviable and infected tissue. Repeat operative debridement is required [5]. The goal of treatment, once the acute infection subsides, focuses on reconstruction of the anatomy and wound closure. For many years, local flaps and split thickness skin grafting have played an integral role in the surgical approach [6]; however, these procedures require a granulating, uninfected wound bed without the presence of biofilm [7,8]. The addition of local agents that accelerate the debridement process may reduce the time to grafting or flap closure. In this case series, surgical debridement was combined with a novel topical desiccating agent (TDA)(DEBRICHEM, DEBx Medical B.V., Amsterdam, Netherlands) applied at the time of the initial surgical intervention in patients with severe diabetic foot infections. The goal was to supplement surgical debridement by removing residual infected tissue and disrupting biofilm and thereby decreasing the time to definitive closure.
Several studies suggest that acid-based desiccants are effective in the treatment of periodontal disease [9-11]. It is believed that the desiccants remove nonviable tissue and dehydrate and destroy biofilm [12]. Skin and soft tissue infections, like periodontal infections, have high bacterial bioburden, complex biofilm formation and high levels of inflammatory proteases; however, the desiccants used to treat periodontal disease are too astringent for open wounds. The novel topical desiccant agent used in this study is, formulated by combining 83% methanesulfonic acid with proton acceptors and dimethyl sulfoxide. This combination is more suitable for open wounds [13].
Materials and Methods
This study was conducted by the primary author at a single medical center. It received ethics committee approval for publication by the local institutional review board (Ethical Board Approval, Date:14.02.2024 Number: AEŞH-BADEK-2024-124, Ankara Etlik Şehir Hastanesi). Prior to surgery, all patients signed an informed consent that included the publication of deidentified information and photography. Eleven(11) patients suffering from severe diabetic foot infections with necrotizing fasciitis of plantar and/or dorsal facia of the foot were treated through a combined surgical and chemical debridement approach using a topical desiccating agent. Six of the 11 patients were recommended below-the-knee amputation at other hospitals. Preoperative evaluation, included history and physical examination, X-rays and comprehensive laboratories. Patient demographics and an overview of laboratory findings are shown in table 1. Broad spectrum antibiotics were started prior to taking the patient to the operating room because of the accompanying sepsis. The surgical intervention involved the excision of necrotic material, infected tissue, and drainage of abscesses. All the procedures were performed under a popliteal nerve block to minimize the risks associated with general anesthesia. Following the surgical debridement and thorough irrigation of the affected area, the topical desiccating agent was applied to further aid in debridement and biofilm control. Postoperatively, antibiotic therapy was continued to mitigate the risk of secondary infections and facilitate recovery. Repeat operative debridement was performed at the discretion of the surgeon. After resolution of the acute infection, the patients underwent split thickness skin grafting for wound closure.
|
Patient |
Age |
Sex |
Comorbidities |
Wound localization |
|
1 |
62 |
M |
Diabetes mellitus, acute myocardial infarction. |
Right heel, and dorsal foot |
|
2 |
61 |
M |
Diabetes mellitus |
Left medial dorsal foot |
|
3 |
70 |
F |
Diabetes mellitus |
Dorsum right foot |
|
4 |
58 |
F |
Diabetes mellitus, hypertension, hyperlipidemia, |
Left dorsal foot |
|
5 |
42 |
M |
Diabetes mellitus. |
Interdigital space between 4th and 5th toes left foot |
|
6 |
49 |
M |
Diabetes mellitus, asthma. |
First toe right foot |
|
7 |
58 |
M |
Diabetes mellitus, cataract, cerebrovascular aneurysm, congestive heart failure. |
Fifth toe |
|
8 |
72 |
M |
Diabetes mellitus |
Left foot first toe, and between 1 and 2 |
|
9 |
59 |
F |
Diabetes mellitus, rheumatoid arthritis |
Left foot |
|
10 |
60 |
M |
Diabetes mellitus, hyperlipidemia |
Right foot |
|
11 |
51 |
M |
Diabetes mellitus |
Right plantar foot |
Table 1: Patient Demographics.
Case Studies
Case 1: A 62-year-old male with long standing diabetes mellitus was referred to the surgery department for treatment of a Wagner 4 diabetic foot ulcer on the right heel. The ulcer had been present for several weeks (Figure 1). His medical history included diabetes mellitus primarily treated with oral hypoglycemic agents. He had a history of coronary artery disease and suffered an acute myocardial infarction 20 years earlier and treated with a percutaneous coronary intervention (PCI). He had peripheral arterial disease for which he underwent stenting of an 80% occlusion of the right iliac artery and 100% occlusion of the right superficial femoral artery, in the month prior to admission. His blood work on admission is shown in Table 2. The patient’s severe diabetic foot infection required immediate surgical intervention which included a prompt surgical drainage and debridement, complemented with chemical debridement with a topical desiccating agent spread over all the exposed surface of the wound (Figure 2). Three days post-surgery the patient underwent further surgical debridement and negative pressure wound therapy was initiated (Figure 3). Following a four-month healing period, during which the wound developed adequate granulation tissue, the patient underwent a successful grafting procedure (Figure 4). He had 100% graft take and complete wound closure (Figure 5).
|
Parameter |
Patient |
Normal Range |
Unit |
LRINEC |
|
WBC |
15.87 |
4.5-10 |
103/mm3 |
1 |
|
Hb |
10 |
13-17 |
g/dL |
2 |
|
Glu |
196 |
80-120 |
mg/dL |
1 |
|
CRP |
138 |
0-5 |
mg/dL |
0 |
|
Cr |
1.28 |
0.7-1.2 |
mg/dL |
0 |
|
Na |
131 |
136-145 |
mmol/L |
2 |
|
Total |
6 |
|||
|
HbA1c |
9.4 |
4-6.1 |
% |
Table 2: Blood work on admission.


Figure 1: Upon admission.

Figure 2: Surgical debridement, and application of topical desiccating agent (right upper photo).

Figure 3: Negative pressure wound therapy installed on the third postoperative day.

Figure 4: Grafting 4 months after the initial operation.

Figure 5: Healed Wound, 2.5 months post-operative. (2.5 months post-grafting).
Case 2: A 61-year-old male was referred to the general surgery department from the infectious disease department for treatment of a bullous lesion on the medial dorsal surface of the left foot. His medical history included diabetes mellitus, hypertension, cataract surgery in 2016, and cessation of smoking 25 years prior. Upon admission, the physical examination revealed purulent discharge from the wound suggestive of a deep infection. His lab work corroborated the physical findings: he had leukocytosis, and elevated C-reactive protein (Table 3, Figure 6). The patient underwent a metatarsophalangeal joint disarticulation (first toe amputation), metatarsal head resection due to osteomyelitis, drainage through a created skin tunnel and chemical debridement with a topical desiccating agent (Figure 7).
|
Parameter |
Patient |
Normal Range |
Unit |
LRINEC |
|
WBC |
14.17 |
4.5-10 |
103/mm3 |
0 |
|
Hb |
9.1 |
13-17 |
g/dL |
2 |
|
Glu |
303 |
80-120 |
mg/dL |
1 |
|
CRP |
228 |
0-5 |
mg/dL |
4 |
|
Cr |
0.82 |
0.7-1.2 |
mg/dL |
0 |
|
Na |
126 |
136-145 |
mmol/L |
2 |
|
Total |
9 |
|||
|
HbA1c |
9.4 |
4-6.1 |
% |
Table 3: Laboratory Values.

Figure 6: First day of admission.

Figure 7: Intraoperative.
On post-operative day 4 debridement and irrigation were repeated in the operating room and, negative pressure wound therapy was applied (Figure 8). On post-operative day eleven debridement, partial suturing of the amputation defect was performed and negative pressure wound therapy continued. On post-operative day 21 the patient underwent total callus and ulcer excision in addition to delayed primary closure. All of his wounds were closed by post-operative day 35 and he was discharged from the hospital.
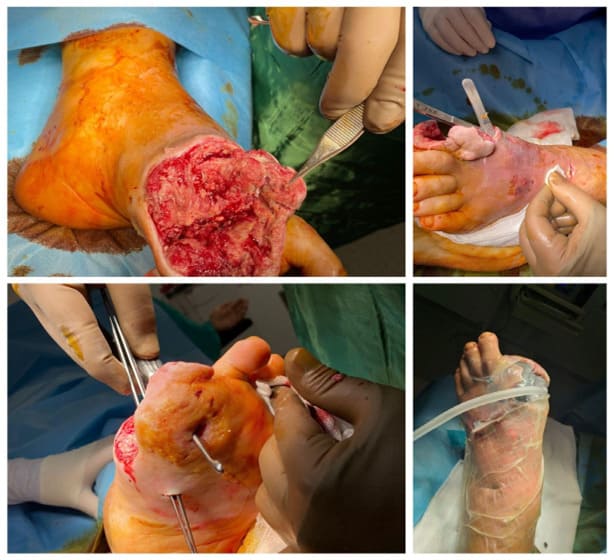
Figure 8: Day four of admission.
On his first follow up visit, 3 weeks later, an abscess was noticed with elevated c-reactive protein levels, the patient was taken to the OR for an emergency drainage. Post-procedure, magnetic resonance image and bone scintigraphy were obtained. The patient was advised to maintain strict bed rest to offload the wound. Fifteen days later, grafting was performed on both defects (Figure 9). He achieved complete closure as shown in Figure 10.

Figure 9: Photo of the follow up visit and, after the graft.

Figure 10: Photos of Follow-up 2 months after grafting.
Results
All eleven patients (8 male, 3 female) had a satisfactory reconstructive result. The average age of the patients was 58 years old. They required an average of 1.7 surgical debridement procedures and 1 chemical procedure (overall average of debridement procedures is 2.45). Patients’ wound duration ranged from 1 week to 5 months. The minimum time to grafting was 33 days, with a maximum time to grafting of 4 months. The median LRINEC score on admission for the eleven patients was 9 indicating the presence of a necrotizing infection [14]. The median LRINEC score on Day 7 for the 11 patients was 3 (Tables 4,5). There were no adverse events related to TDA.
|
LRINEC Score (Day 0) |
LRINEC Score (Day 7) |
|
|
Case 1 |
6 |
2 |
|
Case 2 |
9 |
4 |
|
Case 3 |
4 |
2 |
|
Case 4 |
10 |
4 |
|
Case 5 |
8 |
0 |
|
Case 6 |
8 |
3 |
|
Case 7 |
10 |
4 |
|
Case 8 |
11 |
5 |
|
Case 9 |
8 |
2 |
|
Case 10 |
10 |
6 |
|
Case 11 |
9 |
3 |
|
Mean |
8.45 |
3.2 |
Table 4: Summary of 11 patients - LRINEC.
|
Age/ Gender |
DM duration |
Story of foot problem |
Surgical Treatment |
Microbiology- initial wound culture (tissue) |
PTA |
Result |
|
|
Case 1 |
62 / M |
23 years |
Cracked heel 3 months ago, redness and pain for a week |
Drainage + debridement |
No bacteria isolated |
R-CI and R-SFA |
Grafted after 115 days |
|
Case 2 |
61 / M |
20 years |
Bullous lesion on the plantar side of the 1st toe, purulent discharge for a month, redness and pain for 5 days |
1st toe amputation + MT head resection + drainage + incision of the ankle skin creating a tunnel |
Normal skin flora |
None |
Grafted after 98 days |
|
Case 3 |
70 / F |
25 years |
Trauma related wound on the dorsum of the foot 1 week |
Drainage + debridement |
No bacteria isolated |
R-PTA |
Grafted after 52 days |
|
Case 4 |
58 / F |
25 years |
Draining wound of the foot for 5 months after 5th toe amputation, progressive reddening and pain for 4 days |
Debridement + drainage + 5th mt resection |
Normal skin flora |
L-PTA |
First 3 skin defects grafted after 43 days, last one after 68 days |
|
Case 5 |
42 / M |
10 years |
0.5x0.5 cm “ hole “ like wound between 4th and 5th toes of the left foot for 3 months. Purulent discharge, reddening of the lateral part of the foot for 1 week |
Drainage + debridement |
Streptococcus anginosus |
None |
Grafted after 33 days |
|
Case 6 |
49 / M |
4 years |
Drainage from longstanding callus on the 1st toe of the right foot. Swelling and darkening in color of the 1st toe of the right foot for 10 days. |
1st toe amputation + MT head resection + debridement + drainage |
Trueperella bernardiae |
None |
Grafted after 42 days |
|
Case 7 |
58 / M |
25 years |
Discoloration of the 5th toe for a month, pain, discharge for a couple of days |
5th toe amputation with MT head resection + debridement + drainage |
Streptococcus anginosus |
R-ATA |
Fast wound healing, waiting to heal |
|
Case 8 |
72 / M |
6 years |
Redness and discharge from 1st toe and between 1st and 2nd toe for 3 days |
1st toe amputation with MT head resection + sesamoids’ excision + debridement drainage |
No bacteria isolated |
R-SFA and R-PTA |
Graft planning in 2 weeks |
|
Case 9 |
59 / F |
10 years |
Redness, pain, swelling on 5th for 3 days |
5th toe amputation + debridement + drainage |
No bacteria isolated |
None |
Grafted after 24 days |
|
Case 10 |
60 / M |
10 years |
Small dry necrotic lesions on both feet for 3 months ago, pain, discharge from right foot 15 days after peripheral revascularization |
Drainage + debridement |
Enterococcus faecalis |
R-PTA |
5th toe amputation on day 34 due to complete necrosis. Inpatient wound care |
|
Case 11 |
51 / M |
10 years |
Right foot plantar sideburn from electric heater 3 weeks ago, 1 week later burn from hot water bottle right ankle to 5th toe. Purulent discharge for 2 days |
Drainage + debridement |
Streptococcus agalactiae Staphylococcus aureus |
None |
In-patient wound care |
Table 6: Summary of Time to Grafting.
Discussion
Severe diabetic foot infections challenge the most experienced surgeons. A delay in treatment can lead to catastrophic results. Early surgical intervention has decreased the incidence of amputations associated with severe infections in this population; however, there are still many patients who undergo lower extremity amputation [15]. In one study, the 1- and 5-year survival in diabetics postamputation was 67% and 32% respectively [16]. Most data suggests that the 10-year survival rate is less than 10% [16]. These survival statistics are worse than most common cancers [17]. There is a need for further advances in the treatment of this devastating disease. This case series highlighted the use of a novel topical desiccating agent in combination with aggressive surgical intervention in the treatment of severe diabetic foot infections. Although, this is the first report of using a TDA in combination with surgery for necrotizing diabetic foot infections, there are studies that reported the use of desiccating agents in nonhealing wounds. One case involved the use of a Sulfonic acid desiccant to successfully treat three deep chronic wounds with extensive biofilm [18]. A second case series reported the successful use of the same TDA used in hard-to-heal Venous Leg Ulcers (VLUs). In addition, this study found that the use of TDA in VLUs was cost effective.
There is a paucity of comparative data on length of hospital stay and time to grafting. This study found that the median hospital stay was 31.4 days. One longitudinal study that examined length of stay (LOS) and readmission rates following diabetic foot surgery reported an average hospital stay of 18 days [19]. This is consistent with our findings; however, LOS is influenced by the severity of the disease and the patient’s co-morbidities. The eleven patients reported here had severe necrotizing diabetic foot infections. The same longitudinal study [19] found that hospital readmission rates following diabetic foot surgery were as high as 55%. In this limited case series there was only one readmission for a recurrent abscess (case 2). The sample size in this case series is too small to draw definitive conclusions; however, the findings suggest that the addition of TDA may enhance the debridement procedure and led to more rapid time to reconstruction. The major limitations of this case series is the small number of patients treated, the lack of a control arm and the lack of comparator data on this population of patients.
Conclusion
The results presented here suggest that the addition of a TDA to a surgical debridement procedure may benefit patients with severe necrotizing diabetic foot infections. TDA might make it possible for a surgeon to perform more conservative surgery by avoiding the need to explore every tunnel connecting foot planes beneath the skin. Further study into the use of TDA in infected diabetic foot infections is warranted.
References
- Tuttolomondo A, Maida C, Pinto A (2015) Diabetic foot syndrome: Immune-inflammatory features as possible cardiovascular markers in diabetes. World J Orthop 6: 62-76.
- Arsanjani Shirazi A, Nasiri M, Yazdanpanah L (2016) Dermatological and musculoskeletal assessment of diabetic foot: A narrative review. Diabetes Metab Syndr 2016: S158-164.
- Senneville É, Lipsky BA, Abbas ZG, Aragón-Sánchez J, Diggle M, et al. (2020) Diagnosis of infection in the foot in diabetes: a systematic review. Diabetes Metab Res Rev 2020.
- Adams CA Jr., Deitch EA (2001) Diabetic foot infections. In: Holzheimer RG, Mannick JA, editors. Surgical Treatment: Evidence-Based and Problem-Oriented. Munich: Zuckschwerdt.
- Jeff G. van Baal (2004) Surgical Treatment of the Infected Diabetic Foot, Clinical Infectious Diseases 2004: S123-S128.
- Clemens MW, Attinger CE (2010) Functional reconstruction of the diabetic foot. Semin Plast Surg 24: 43-56.
- Unal S, Ersoz G, Demirkan F, Arslan E, Tütüncü N, et al. (2005) Analysis of skin-graft loss due to infection: infection-related graft loss. Ann Plast Surg 55: 102-106.
- Hom DB, Ostrander BT (2023) Reducing Risks for Local Skin Flap Failure. Facial Plast Surg Clin North Am 31: 275-287.
- Cogo A, Quint BJ, Bignozzi CA (2021) Restarting the Healing Process of Chronic Wounds Using a Novel Desiccant: A Prospective Case Series. Wounds 33: 1-8.
- Pini-Prato G, Magnani C, Rotundo R (2016) Treatment of acute periodontal abscesses using the biofilm decontamination approach: a case report study. Int J Periodontics Restorative Dent 36: 55-63.
- Lauritano D, Petruzzi M, Nardi GM (2015) Single application of a dessicating agent in the treatment of recurrent aphthous stomatitis. J Biol Regul Homeost Agents 29: 59-66.
- Lombardo G, Signoretto C, Corrocher G (2015) A topical desiccant agent in association with ultrasonic debridement in the initial treatment of chronic periodontitis: a clinical and microbiological study. New Microbiol 38: 393-407.
- Cogo A, Bignozzi AC, Hermans MH, Quint BJ, Snels JP, et al. (2022) A desiccation compound as a biofilm- and necrosis-removing agent: a case series. J Wound Care 31: 816-822.
- Hoesl V, Kempa S, Prantl L, Ochsenbauer K, Hoesl J, et al. (2022) The LRINEC Score-An Indicator for the Course and Prognosis of Necrotizing Fasciitis? J Clin Med 11: 3583.
- Taylor Jr LM, & Porter JM (1987) The clinical course of diabetics who require emergent foot surgery because of infection or ischemia. Journal of vascular surgery 6: 454-459.
- Christopher J. Schofield, Gillian Libby, Geraldine M. Brennan, Ritchie R. MacAlpine, Andrew D. Morris, Graham P (2006) Leese, for the DARTS/MEMO Collaboration; Mortality and Hospitalization in Patients After Amputation: A comparison between patients with and without diabetes. Diabetes Care 29: 2252-2256.
- Armstrong DG, Swerdlow MA, Armstrong AA, Conte MS, Padula WV, et al. (2020) Five-year mortality and direct costs of care for people with diabetic foot complications are comparable to cancer. J Foot Ankle Res 13: 16.
- Guest JF, Deanesi V, Segalla A (2022) Cost-effectiveness of Debrichem in managing hard-to-heal venous leg ulcers in the UK. J Wound Care 31: 480-491.
- Kim TG, Moon SY, Park MS, Kwon SS, Jung KJ, et al. (2016) Factors Affecting Length of Hospital Stay and Mortality in Infected Diabetic Foot Ulcers Undergoing Surgical Drainage without Major Amputation. J Korean Med Sci 31: 120-124.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.