The Sphenoid Sinus Revisited
Geerinck K, Dockx M, Eloy Ph*
CHU UCL Namur, site of Godinne, Avenue Therasse, 5530, Yvoir, Belgium
*Corresponding author: Pr Eloy, ENT department, CHU UCL Namur, site of Godinne, Avenue Therasse, 5530, Yvoir, Belgium
Received Date: 19 August 2022
Accepted Date: 23 August 2022
Published Date: 26 August 2022
Citation: Geerinck K, Dockx M, Eloy Ph (2022) The Sphenoid Sinus Revisited. Review Article. Ann Case Report 7: 922. DOI:https://doi.org/10.29011/2574-7754.100922
Abstract
In the past, the sphenoid sinus has often been overlooked. It was considered as an inaccessible paranasal sinus cavity due to its specific anatomical location, making it difficult to diagnose diseases.
Today, the sphenoid sinus is regarded as equal to any other paranasal sinus cavity, and thus home to various diseases. Over the years, the assessment of these diseases has improved. Indeed, nasal endoscopy and qualitative head imaging (CT-scan and MRI) have been developed. These technologies provide information about the nature of disease, about the state of the walls of the sphenoid sinus and about extension of a lesion to adjacent structures. The endoscopic endonasal approach has improved safety and efficacy of sphenoid sinus surgery. Moreover, the sphenoid sinus acts as a gateway to the skull base. In fact, it enables removal of sellar and parasellar lesions. This endoscopic endonasal transsphenoidal approach (EETA) has lower morbidity rates than transcranial approaches.
The authors propose an overview of the sphenoid sinus from an ENT point of view.
Introduction
The sphenoid sinuses are the most posterior and medial paranasal sinus cavities, located deep inside the head. Different important neurovascular structures surround them. Embryologically, they originate from the cartilaginous nasal capsule (1). They result from the pneumatization of the sphenoid bone. There is no sphenoid sinus in newborns. Pneumatization starts at the age of 3, initially in posterior, inferior and lateral directions. At the age of 7 the pneumatization goes up to the sella turcica. At 18 the development is completed (2).
In adults, 4 different degrees of pneumatization have been described: the conchal, presellar, sellar and postsellar pattern.
In the conchal type, the posterior wall of the sinus is located anteriorly to the sella turcica. Among Caucasians, this type of pneumatization is the least common one. Its incidence varies from 0% to 5% (3,4).
Because of the thickness of bone present between the anterior sphenoid wall and the sella turcica, a transsphenoidal approach is not recommended in case of sellar surgery. In the presellar type, the posterior limit of the sinus extends into the anterior portion of the sella. Its incidence varies from 24% to 28% in Caucasians.
Finally, the sellar and postsellar types of pneumatization are most prevalent. Together, their incidence varies from 67% to 80%. These are the preferred types when performing endonasal surgery of the sphenoid sinus and surgery of the pituitary gland (3,5,6).

Figure 1: The 4 types of pneumatization of the sphenoid sinus. (A) In conchal pneumatization, the sinus cavity is almost virtual. (C, D) The most appropriate patterns for endoscopic endonasal transsphenoidal surgery are the sellar and post-sellar types.
Relevant anatomy
Generally, the sphenoid sinuses are separated by at least one intersinus septum. This septum is a thin sagittal bony plate, rarely median, which should always be identified on preoperative imaging. Indeed, it might be inserted onto the carotid or the optic nerve canal instead of the sellar floor. Some sphenoid sinuses have no intersinus septum, others have an accessory septum or even multiple ones (6).
The Onodi cell (OC) is the most posterior and lateral ethmoidal cell. It has important relationships with the optic nerve, which is lateral and superior to it. The sphenoid sinus is situated more medially, inferiorly and posteriorly (3,7).
Each sphenoid sinus communicates with the nasal cavity by means of an aperture in the upper part of the anterior wall. This aperture, also called an ostium, is situated at the junction of the superior third and the two inferior thirds of the anterior wall of the sphenoid sinus. The superior turbinate is the best surgical landmark to identify the natural ostium. It separates the sphenoethmoidal recess and the posterior ethmoid (8). In 85% of cases the ostium is situated medially to the posterior end of the superior turbinate (ST), in the sphenoethmoidal recess. In 15% of cases, it is situated lateral to the tail of the ST (9-11).
The lateral sinus wall contains noble structures. Often, the internal carotid artery (ICA) and the optic nerve (ON) can be identified bulging in the sphenoid cavity. In between there is the optico-carotid recess (OCR). In some cases, the maxillary nerve or the second branch of the trigeminal nerve (V2) and the Vidian nerve (V) may be recognized. The more pneumatized the sphenoid sinus, the more these structures are protruding. Therefore, they may be at risk during surgery, in case the surgeon is too posterior and lateral in the sphenoid cavity (3,12).
After removal of the bone covering the sella and the planum sphenoidale, access to the dura mater is gained. When the dura is opened, the following structures can be seen: The optical chiasma, the pituitary stalk, the sella, the basilar artery and the genu of the internal carotid artery (which might be close to the pituitary gland).
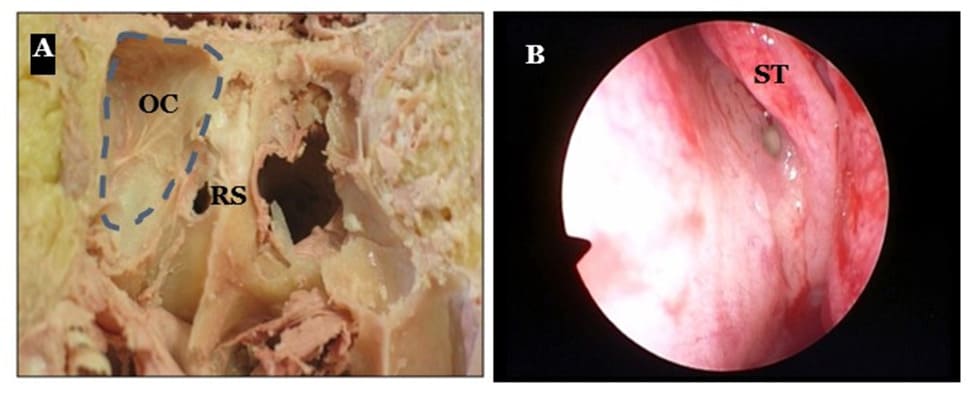
Figure 2:(A) The Onodi cell (OC) and the Rostrum Sphenoidale (RS) on a cadaver. (B) Endoscopic view showing the ostium of the sphenoid sinus along the tail of the superior turbinate - left side.
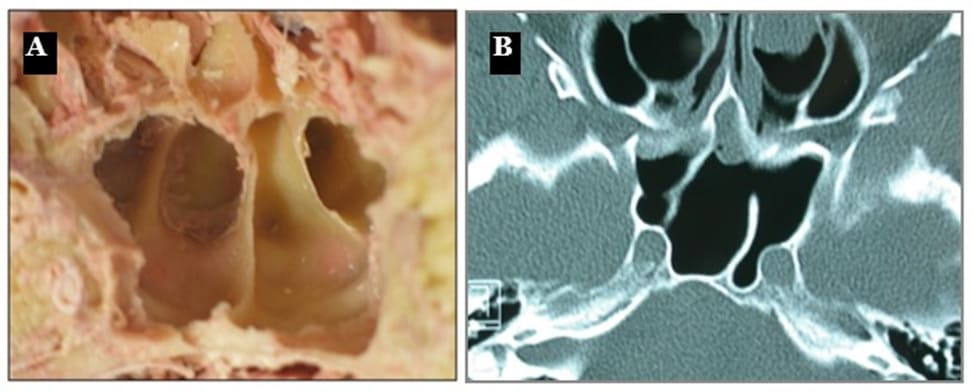
Figure 3: (A) Coronal cadaver view of the sphenoid sinuses. (B) Axial CT-scan demonstrating an oblique paramedian intersinus septum and a bony partition in the left sphenoid sinus.
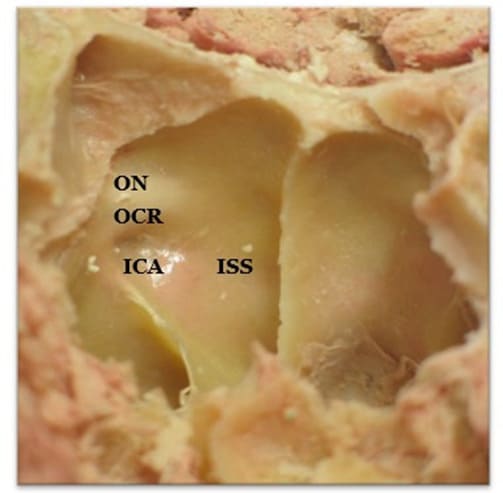
Figure 4: Cadaveric anterior view of the lumen of the sphenoid sinus and its right bony laterall wall, after removal of mucosa. The bulges of the internal carotid artery (ICA) and of the optic nerve (ON) can be seen. These form the optico-carotid recess (OCR). In the middle, the posterior insertion of the intersinus septum (ISS).
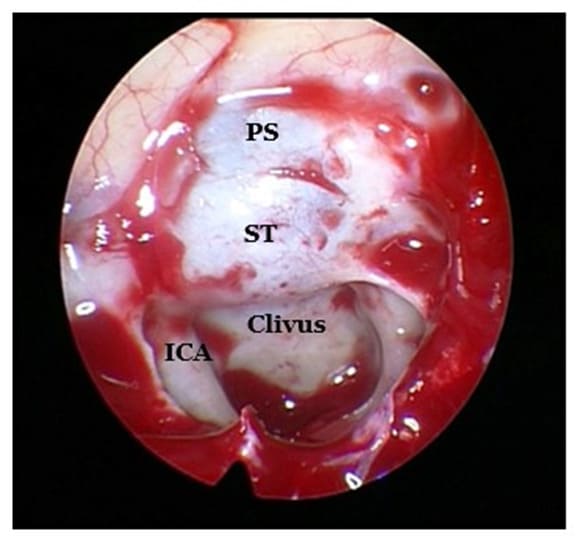
Figure 5: Endoscopic view during surgery showing the superior wall of the sphenoid sinus. Centrally, the bulge of the sella turcica (ST), anterior to it the planum sphenoidale (PS) and posterior to it the clivus. Lateral to the clivus, the paraclival portion of the ICA can be seen.
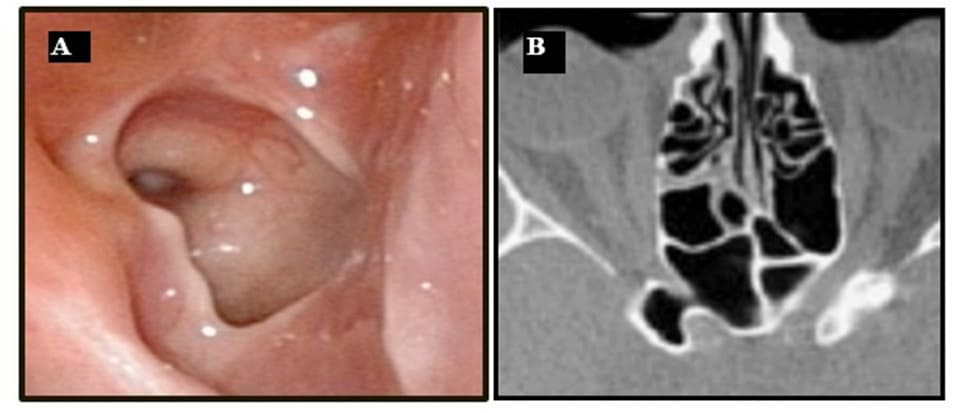
Figure 6: (A) Endoscopic view of the lateral wall with protrusion of the ICA and of the optic nerve. (B) Axial CT-scan showing the optic nerve in the sphenoid cavity.
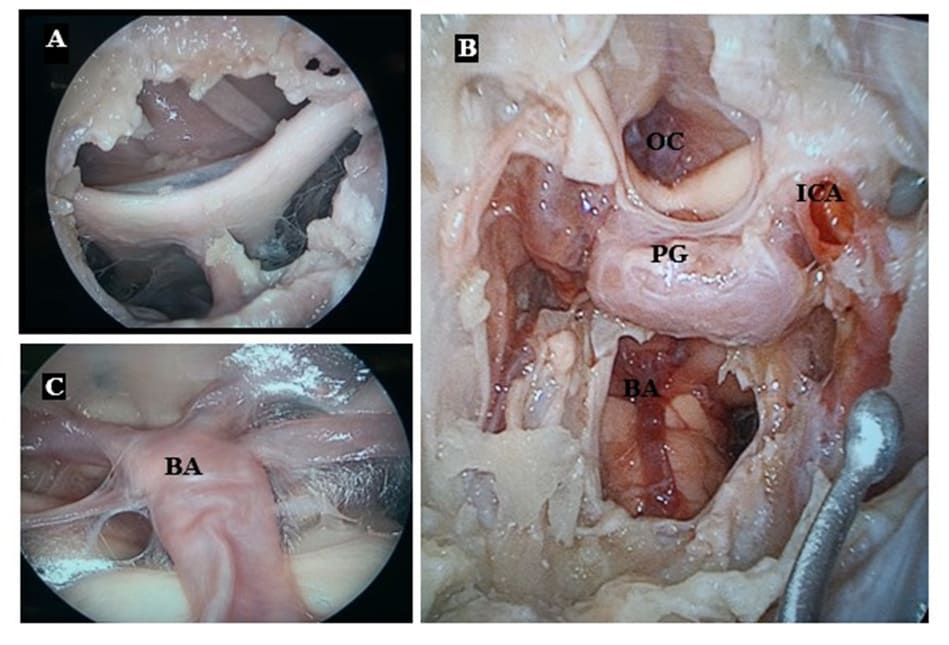
Figure 7: (A) Dissection on cadaver; visualization of the optical chiasma after removal of the planum sphenoidale and incision of the dura mater. (B) Wide dissection showing the pituitary gland (PG) in the center, the proximity of the genu of the ICA, the optical chiasma (OC) and the basilar artery (BA) once the clivus is drilled out. (C) Basilar artery in front of the pons.
Another important space is the lateral recess. It is found in well-developed sphenoid sinuses, where it is formed by pneumatization of the superior portion of the pterygoid process. Two important structures limit the lateral recess medially: the Vidian nerve lying in the Vidian canal inferiorly and the maxillary nerve (V2) superiorly, at the level of the foramen rotundum. These structures can be identified on a CT-scan. A lateral recess is correlated with a greater distance between those two nerves. Thus, it informs on the potential risk to neurovascular structures. This is important when using the transnasal approach for middle cranial fossa surgery (12).

Figure 8: The lateral recess (LR) and its medial limits: the Vidian canal (VC) and the foramen rotundum with the V2 on a coronal CT-scan.
Pathologies
In the past, the sphenoid sinus has often been overlooked. Indeed, it was considered as an inaccessible paranasal sinus.
In the past decades, nasal endoscopy and superior imaging (CT and MRI) have been developed and improved. Thus, the sphenoid sinus has gained equal importance as any other paranasal sinus cavity. In fact, a variety of pathologies can now be diagnosed and treated (13-15).
Pathologies of the sphenoid sinus are generally classified into infectious, inflammatory and primary tumors (benign and malignant). The sphenoid sinus can also be invaded by abnormal adjacent structures such as an aneurysm of the internal carotid artery. A meningocele, associated or not with a CSF leak, can fill the sphenoid sinus through a skull base defect (16). Tumors from adjacent structures may occupy the sphenoid cavity. Even metastatic disease might develop in the sinus (13).
The infectious diseases include acute, subacute and chronic sphenoiditis and infected mucoceles (mucopyoceles), as well as fungal sinusitis (fungus ball or mycetoma, invasive fungal sphenoiditis, allergic fungal sinusitis) (17,18).
The mucocele and the sphenochoanal polyp are often considered as inflammatory diseases. A mucocele can be primary (presumed to be caused by blockage of the natural ostium) or secondary to sinus surgery, to a trauma or it can be related to a tumor (14,22).
Fibrous dysplasia and inverted papilloma are benign tumors which can rapidly extend and invade or erode surrounding bone, thus leading to serious neurologic complications.
Primary malignant tumors include but are not limited to chondrosarcoma, adenocarcinoma and lymphoepithelioma.
The sphenoid sinus can also be invaded by a nearby sinonasal tumor such as juvenile angiofibroma (JNA) or adenocarcinoma of ethmoid. Another cause of secondary invasion is a tumor originating from adjacent tissue as in meningioma or invasive pituitary gland adenoma.
Physical findings and history alone are often not helpful in determining the nature of the pathology. Only longstanding nonevolutive symptoms may evoke a benign disease. However, even benign lesions have been reported to rapidly cause neurological
complications. In fact, a case of fibrous dysplasia has led to obliteration of the optic foramina causing bilateral blindness (13). Mucopyoceles have been described to cause bone erosion and cranial nerve palsy (14). Headache is often the initial symptom. Should it rapidly worsen or in case of persistence despite analgesics, then nasal endoscopy and head imaging are required (15,23). On the images, the sphenoid sinus should be carefully inspected for any anomaly. Indeed, sphenoid diseases may present without any nasal symptoms. Even more so, they might present at first with cranial nerve involvement. Then, the optic (II), the maxillary (V2) and the abducens nerve (VI) are most commonly involved (13).
Infectious diseases
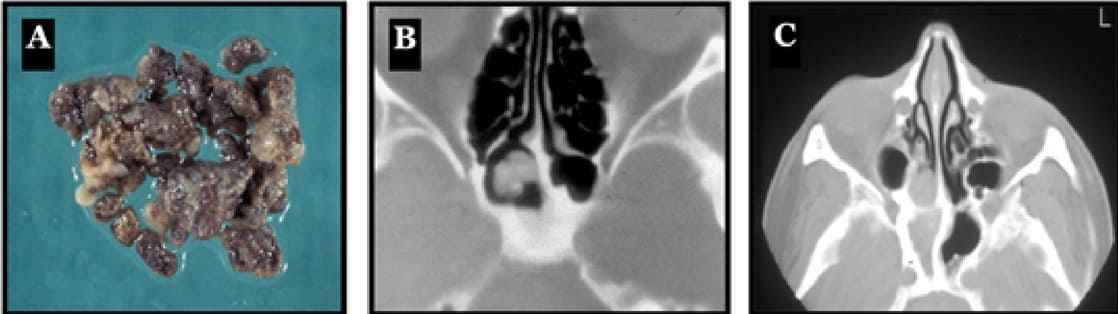
Figure 9:(A) Macroscopic view of a mycetoma shows grey and compact material. (B) Axial CT-scan of a mycetoma characterized by an opacity in the sphenoid sinus with surprisingly, a patent ostium. (C) Typical axial CT-scan of a fungal ball in the sphenoid sinus. The image reveals a polyp extruding from the ostium of the sphenoid cavity, a sclerosis of the bony walls and a complete opacity of the sphenoid sinus. In this case, no microcalcifications can be seen.
Inflammatory diseases
A sphenochoanal polyp is a rare form of a choanal polyp originating from the sphenoid sinus and extending to the choanae through the sphenoethmoidal recess. Far less common than the antrochoanal polyp, the sphenochoanal polyp originates from the sphenoid sinus itself or from the sphenoid ostium. Endoscopic surgery is indicated to relieve the nasal obstruction (19-21).
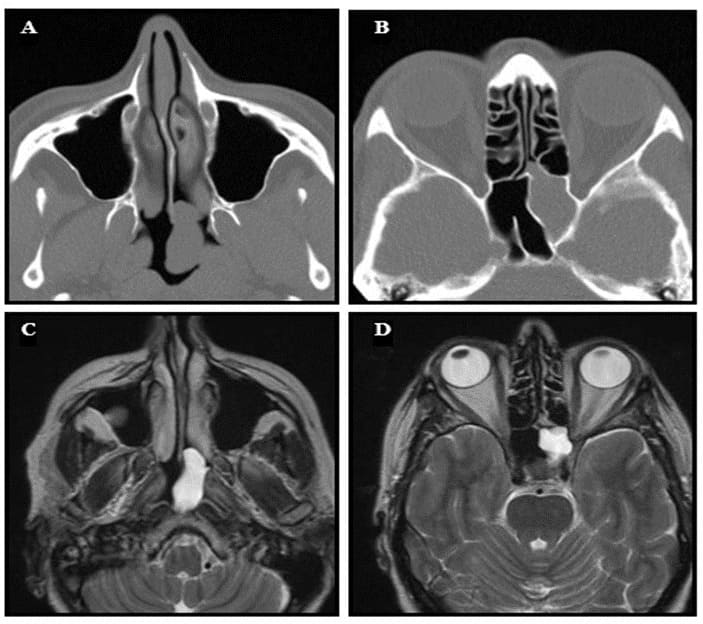
Figure 10: A case of a sphenochoanal polyp. (A) Axial CT-scan showing an opacity in the nasopharynx. (B) Axial CT-scan showing opacity of the left sphenoid sinus. (C) T2-weighted axial MRI showing homogeneous opacity of the polyp in the nasopharynx. (D) T2weighted axial MRI showing a hyperintense lesion in the sphenoid sinus.

Figure 11: Axial CT-scan of a mucocele.

Figure 12: Coronal CT-scan showing a meningocele protruding in the right sphenoid sinus through a bony dehiscence (black arrow), thus filling the lateral recess (LR). It might be associated with an encephalocele.
Tumors
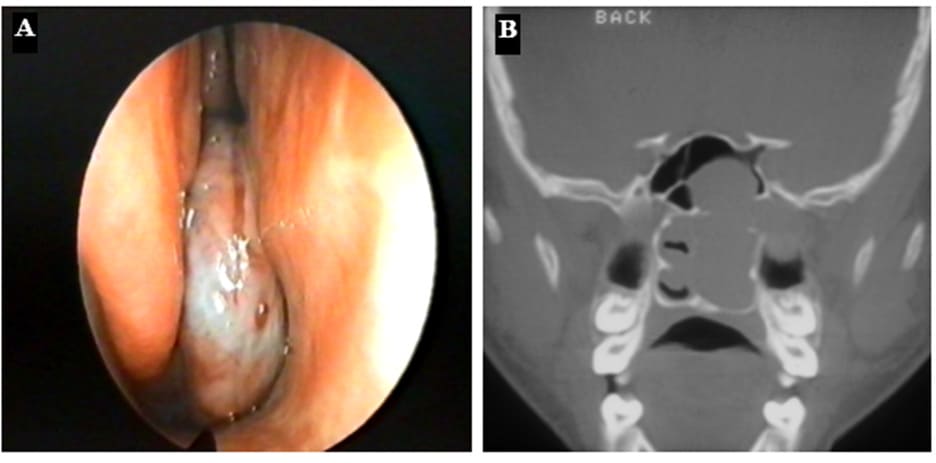
Figure 13: (A) Endoscopic view of a JNA in the posterior part of the right nasal cavity. (B) Coronal CT-scan of a patient with a JNA on the left side: complete nasal obstruction, bulging in the sphenoid sinus and widening of the pterygopalatine fossa.
Surgical approaches
During the last decade, surgical approaches to the sphenoid sinus have evolved, mostly thanks to the development of the nasal endoscope (24). Besides removal of sphenoid sinus lesions, the endoscopic technique allows for safe and efficient skull base surgery. Indeed, the endoscopic endonasal transsphenoidal approach (EETA) enables removal of sellar and parasellar lesions with lower morbidity rates than transcranial approaches (25).
However, the transseptal approaches remains well known among experienced rhinologists and neurosurgeons.
The transseptal approach
This approach was the golden standard before the development of the endoscopic techniques. It has the advantage of approaching the sphenoid sinus on the midline, far from the lateral sinus wall and its noble neurovascular structures. It has been used in case of isolated sphenoid diseases, distorted anatomy and pituitary or skull base surgery.
There are two different ways to perform it: either via a sublabial approach or via an endonasal approach.
1) The sublabial transseptal approach
This approach was commonly used by the neurosurgeon for pituitary surgery performed with the microscope. Indeed, this approach gave a large opening, giving the possibility to use a large nasal speculum such as a Dott speculum. After visualization of the anterior walls of both sphenoid sinuses, the neurosurgeon used the microscope to realize the neurosurgical steps of the procedure (26).


Figure 14: (A) Sublabial approach. (B) Intraoperative view with the operating microscope. The anterior walls of the sphenoid sinuses can be identified on both sides.
2) The endonasal transseptal approach
This approach was preferred by the rhinologists. It has the same advantages than the sublabial approach, but with less risk of hypoesthesia of the teeth or of the superior lip. The absence of resection of the anterior nasal spine also reduces the risk of nasal collapse. The surgery starts with patient in supine position. After infiltration of the nasal septum with xylocaine 1% + diluted adrenaline, the surgeon starts the procedure with an endonasal incision similar as in a septoplasty.
Then, the mucoperichondrium is elevated on both sides, exposing the quadrangular cartilage and the vertical plate of the ethmoid bone.
An inferior and a posterior chondrotomy are performed, displacing the quadrangular cartilage to the opposite side. The vertical plate of the ethmoid is then resected up to the rostrum sphenoidale. The anterior wall of the sphenoid sinus is then opened, on both sides if needed.
Some adverse events were reported with the transseptal approach. These include a fracture of the anterior nasal spine, a nasal collapse (possibly presenting with a saddle nose), a septal dislocation, a hematoma or a septal perforation (27).

Figure 15: The transseptal approach with the nasal speculum in place.
The endoscopic approaches
1) The transostial sphenoidotomy (via the sphenoethmoidal recess)
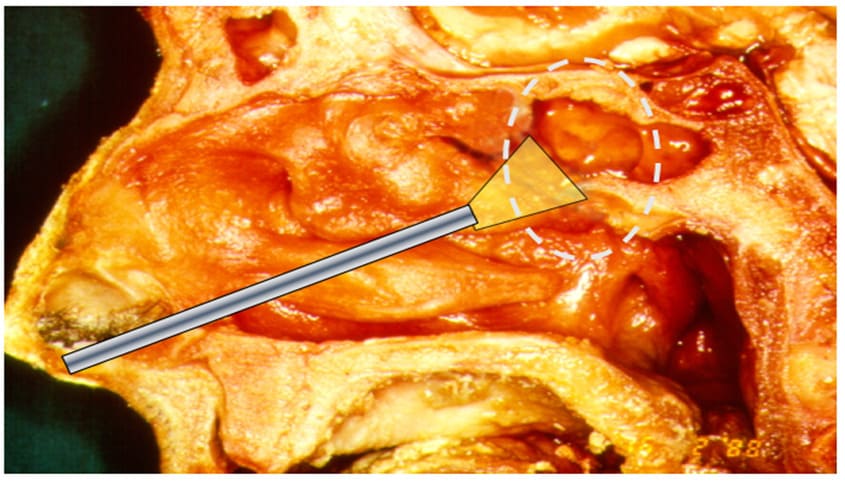
Figure 16: The transostial approach to the sphenoid sinus on a cadaver.
Over the last twenty years, the transostial approach has progressively become the first-line approach for the treatment of isolated sphenoid sinus diseases and for resection of pituitary adenomas and other sellar lesions (28,29). This approach is simple and direct. It is associated with low morbidity. However, recurrence of disease has been described, in some cases due to postoperative closure of the sphenoidotomy (30,31).
The procedure starts with an outfracture of the inferior turbinate and a lateral retraction of the middle and superior turbinates exposing the sphenoethmoidal recess and the sphenoidal ostium. The superior turbinate separates the sphenoethmoidal recess medially from the superior meatus laterally. In case the approach is too narrow, a partial resection of the middle turbinate, a limited septoplasty or even an opening of the last ethmoidal cell may be realized (32).
Once the ostium is identified, it is enlarged with a Cottle elevator or with a bone rongeur (a Kerrison or Citelli forceps). If it is not found, the anterior wall of the sinus may be perforated at its weakest point. The surgeon should keep in mind that the septal branch of the sphenopalatine artery runs on the anterior wall of the sphenoid sinus at the level of the free border of the superior turbinate. This artery can be cauterized to avoid significant bleeding. If the bony wall is too thick, a drill might be used. The mucosa of the sphenoid sinus is usually preserved except in case of tumor. The size of the sphenoidotomy is adapted to the conditions of control and of resection of the disease (33).
In 2014, D Simmen et al. described 3 types of sphenoidotomy (34).
Type I consists of opening the ostium, whereas in Type II this opening is widened inferiorly, laterally and superiorly. Type III consists of a paraseptal approach combining a bilateral type II sphenoidotomy with a septal window.
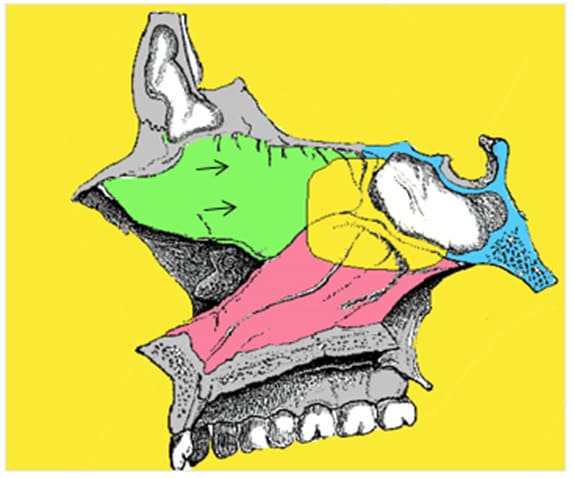
Figure 17: The septal window (black arrows).
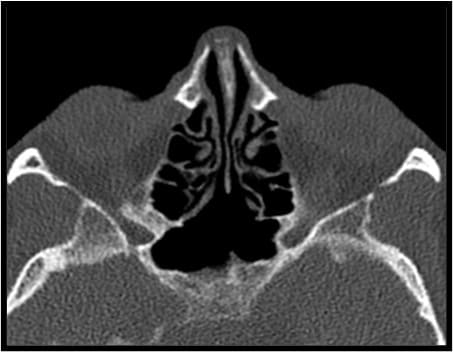

Figure 18: CT-scan showing the postoperative result of a Type III sphenoidotomy.
2) The transethmoidal approach
This approach gives a larger access. It is performed after a complete ethmoidectomy or after opening the posterior ethmoidal cells only. Here, the superior turbinate is resected. It is important to note that the sphenoid sinus is situated medially, inferiorly and posteriorly to the last ethmoidal cell, the Onodi cell. The superior turbinate remains the chief landmark (35).

Figure 19: The relationship between the Onodi cell (OC), the superior turbinate (ST) and the ostium of the sphenoid sinus. Left side.
3) The transpterygoid approach
This approach is performed in some specific cases, as when entrance to the lateral recess of the sphenoid is needed.
An indication is the repair of a CSF leak associated with a meningoencephalocele originating from Sternberg’s (lateral craniopharyngeal) canal. The pterygoid bone is also crossed when Meckel’s cave needs to be accessed. This might be the case for removal of a trigeminal schwannoma or a meningioma. It comprises a large middle meatal antrostomy, ligation of the sphenopalatine artery, a large sphenoidotomy and a drilling of the base of the pterygoid bone. Then, the use of the navigation system is recommended (12,36,37).
Conclusion
The sphenoid sinus has its own very specific anatomy with close relationships to vital neurovascular structures. Imaging allows for more accurate determination of the nature and extension of diseases. Moreover, it provides information about the sphenoid anatomy and its multiple variations. This is especially helpful when approaching the skull base. The endoscope has vastly improved safety and efficacy of surgery. The endonasal endoscopic transsphenoidal approach has become the golden standard to treat sellar, suprasellar and parasellar lesions.
Author Contributions: KG: conception, drafting the article, collection of relevant articles, revising the article for important intellectual content. MD: initial drafting, collection of relevant articles. PE: conception, drafting the article, revising the article for important intellectual content. Image courtesy of PE. All authors contributed to the article and approved the submitted version.
Conflict of Interest: The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- Wang RG, Jiang SC, Gu R. (1994) The cartilaginous nasal capsule and embryonic development of human paranasal sinuses. J Otolaryngol. 23: 239-43.
- Wolf G, Anderhuber W, Kuhn F (1993) Development of the paranasal sinuses in children: implications for paranasal sinus surgery. Ann Otol Rhinol Laryngol. 102: 705-11.
- Lang J (1989) Clinical Anatomy of The Nose, Nasal Cavity, and Paranasal Sinuses. New York, NY, Thieme.
- Congdon ED (1920) The distribution and mode of origin of septa and walls of the sphenoid sinus. Anat Rec. 8: 97-123
- Wang J, Bidari S, Inoue K, Yang H, Rhoton A Jr (2010) Extensions ofthe sphenoid sinus: a new classification. Neurosurgery, 66: 797-816.
- Hamid, O., El Fiky, L., Hassan, O., Kotb, A., & El Fiky, S. (2008). Anatomic Variations of the Sphenoid Sinus and Their Impact on Trans-sphenoid Pituitary Surgery. Skull base : official journal of North American Skull Base Society ... [et al.], 18(1), 9–15.
- Meybodi AT, Vigo V, Benet A (2017) The Onodi Cell: An Anatomic World Neurosurg. 103: 950.e5-950.e6.
- Kim HU, Kim SS, Kang SS, et al. (2001) Surgical anatomy of thenatural ostium of the sphenoid sinus. Laryngoscope 111: 1599-1602.
- Van Alyea OE (1941) Sphenoid sinus: Anatomic study, with consideration of the clinical significance of the structural characteristics of the sphenoid sinus. Arch Otolaryngol. 34: 225–253.
- Campero, J. Emmerich, M. Socolovsky, Martins C, Yasuda A, et al.(2010) Microsurgical anatomy of the sphenoid ostia J Clin Neurosci, 17: 1298-1300.
- Bolger WE, Keyes AS, Lanza DC (1999) Use of the superior meatus and superior turbinate in the endoscopic approach to the sphenoid Otolaryngol Head Neck Surg 120: 308-313.
- Vaezi A, Cardenas E, Pinheiro-Neto C, Paluzzi A, Branstetter BF 4th, et (2015) Classification of sphenoid sinus pneumatization: relevance for endoscopic skull base surgery. Laryngoscope. 125: 577-81.
- Levine H (1978) The sphenoid sinus, the neglected nasal sinus. Arch 104: 585-7.
- Sethi D (1999) Isolated sphenoid lesions: diagnosis and management. Otolaryngol Head Neck Surg. 120: 730-6.
- Yap HJ, Ramli RR, Yeoh ZX, Sachlin IS (2022) Series of isolated sphenoid disease: Often neglected but perilous. SAGE Open Med Case Rep. 10: 2050313X221097757.
- Yıldırım AE, Dıvanlıoglu D, Cetinalp NE, Belen AD. Endoscopic endonasal repair of spontaneous sphenoid sinus lateral wall meningocele presenting with cerebrospinal fluid leak. J Neurosci Rural Pract. 2014;5(2):168-170. doi:10.4103/0976-3147.131668
- Eloy P, Grenier J, Pirlet A, Poirrier AL, Stephens JS, Rombaux P (2013) Sphenoid sinus fungall ball: a retrospective study over a 10- year period. Rhinology. 51: 181-8.
- Karkas, R. Rtail, E. Reyt, N. Timi, C.A. Righini (2013) Sphenoid sinusfungus ball. Eur Arch Otorhinolaryngol, 893-898.
- Eloy PH, Evrard I, Bertrand B, Delos M (1996) Choanal polyp of sphenoidal origin -Report of two cases. Acta oto-rhino-laryngologica belg 50: 183-189.
- Crampete L, Mondain M, Rombaux PH (1995) Sphenochoanal polyp in children. Diagnosis and treatment. Rhinology 33: 43-45.
- Weissman JL, Tabor EK, Curtin HD (1991) Sphenochoanal Polyps: Evaluation with CT and MR Imaging. Radiology 178:145-148.
- Michael J Brockbank and Gerald B. Brookes (1991) The sphenoiditis spectrum, Clinical otolaryngology, 16: 15-20.
- Wang ZM, Kanoh N, Dai CF, Kutler DI, Xu R, et al. (2002) Isolated sphenoid sinus disease: an analysis of 122 cases. Ann Otol Rhinol 111: 323-7.
- Cheung DK, Martin GF, Rees J (1992) Surgical approaches to thesphenoid sinus. J Otolaryngol. 21: 1-8.
- Van Gerven, L., Qian, Z., Starovoyt, A., Jorissen, M., Meulemans, J., van Loon, J., De Vleeschouwer, S., Lambert, J., Bex, M., & Vander Poorten, V. (2021). Endoscopic, Endonasal Transsphenoidal Surgery for Tumors of the Sellar and Suprasellar Region: A Monocentric Historical Cohort Study of 369 Patients. Frontiers in oncology, 11, 643550.
- Lee K. J. (1978). The sublabial transseptal transsphenoidal approach to the hypophysis. The Laryngoscope, 88(7 Pt 2 Suppl 10), 1–65.
- Escajadillo, J. R., & de Gortari, E. (1983). Transseptal approach for the treatment of pituitary lesions. Archives of otolaryngology (Chicago, Ill. : 1960), 109(5), 326–328.
- Eloy, P., Watelet, J. B., Donckier, J., Gustin, T., Gaudon, I. P., Collet, S., Rombaux, P., Gillard, C., & Bertrand, B. (2005). Endoscopic and microscopic paraseptal transsphenoidal approach to the sella turcica. Rhinology, 43(4), 271–276.
- Varshney, S., Gupta, C., Bansal, K. K., Bist, S. S., & Bhagat, S. (2013). Endoscopic Trans-Nasal Trans-Sphenoidal (TNTS) Approach For Pituitary Adenomas: Our Experience. Indian journal of otolaryngology and head and neck surgery : official publication of the Association of Otolaryngologists of India, 65(Suppl 2), 308–313.
- Gilain, D. Aidan, A. Coste, R. Peynegre (1994) Functional endoscopic sinus surgery for isolated sphenoid sinus disease. Head Neck, 16: 433-437.
- Castelnuovo P, Pagella F, Semino L, De Bernardi F, Delù G. (2005) Endoscopic treatment of the isolated sphenoid sinus lesions. Eur Arch 262: 142-7.
- DA Kieff N. Busab (2002) Treatment of isolated sphenoid sinus inflammatory disease by endoscopic sphenoidotomy without Laryngoscope, 112: 2186-2188.
- Stammberger (1985) Endoscopic surgery for mycotic and chronic recurring sinusitis. Ann Otol Rhinol Laryngol Suppl, 119: 1-11.
- Simmen D, Jones N (2014) Sphenoethmoidektomie sphenoidale Sinusotomie Typ I, II, III-Teil I [Sphenoethmoidectomy with or without sinusotomy type I, II, III - I]. Laryngorhinootologie. 93: 423-9.
- Socher, J. A., Cassano, M., Filheiro, C. A., Cassano, P., & Felippu, A. (2008). Diagnosis and treatment of isolated sphenoid sinus disease: a review of 109 cases. Acta oto-laryngologica, 128(9), 1004–1010.
- Bolger WE, Osenbach R (1999) Endoscopic transpterygoid approach to the lateral sphenoid recess, ear Nose Throat journal 78: 36-46.
- Kasemsiri P, Solares CA, Carrau RL, Prosser JD, Prevedello DM, et al. (2013) Endoscopic endonasal transpterygoid approaches: anatomical landmarks for planning the surgical corridor. Laryngoscope. 123: 811
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.