The Largest Ever Reported Ovarian Cystadenofibroma: A Case Report
by Ayodele David Aina*, Saboohi Tariq, Kevin Hickey
University Hospital Limerick, Ireland
*Corresponding Author: Ayodele David Aina, University Hospital Limerick, Ireland
Received Date: 08 June 2025
Accepted Date: 16 July 2025
Published Date: 18 July 2025
Citation: Aina AD, Tariq S, Hickey K (2025). The Largest Ever Reported Ovarian Cystadenofibroma: A Case Report. Ann Case Report. https://doi.org/10: 2344. DOI:10.29011/2574-7754.102344
Keywords: Ovarian Cystadenofibroma; Benign Tumour; Malignant Tumours; Abdominal Hysterectomy.
Introduction
Ovarian Cystadenofibroma is a rare benign tumour of the ovary, mainly affecting women aged 15-65 years and occur in 1.7% of benign ovarian tumours [1]. It arises from the germ cells in the ovarian stroma and are categorised according to the epithelial cell types. The tumour can be solid, cystic, or semi-solid depending upon the fraction of the epithelium and the stroma it contains [2]. Presentation can vary from being asymptomatic to vague abdominal pain, heaviness, or abdominal distension. The presentation is usually as a solitary ovarian mass or less commonly as multiple masses of a single ovary, but rarely involves both ovaries [3].
Magnetic resonant imaging (MRI) showing dense fibrous stromal proliferation with scattered small cystic glandular structures on the T2-weighted images can help diagnose ovarian Cystadenofibroma and differentiate between benign and malignant tumours [4], although multiple imaging modalities are often used.
Case Report
A 71year old woman, presented with increasing abdominal distention and weight gain over four years. She had a prior total abdominal hysterectomy with left Salpingo-oophorectomy thirty years earlier for heavy periods. On presentation she was clinically well with no pain but significant abdominal pressure and swelling. Initial laboratory investigations including full blood count, renal and liver function which were all normal and CA 125 was 140iu/ ml. Pelvic ultrasound showed a large cystic mass.
A CT scan confirmed a complex midline predominantly cystic multiloculated abdominopelvic mass with enhanced internal septation and nodularity present, approximately 54cm in size. Portal vein and inferior vena cava compression seen as well as significantly dilated renal pelves and hydroureter secondary to compression. Assessment of lymphadenopathy, omental and peritoneal disease was not possible due to severe compression of structures by the cyst.
As illustrated in (Figure 1, 2) intraabdominal organs were severely compressed with pressure on the spinal vertebrae and rib cage.
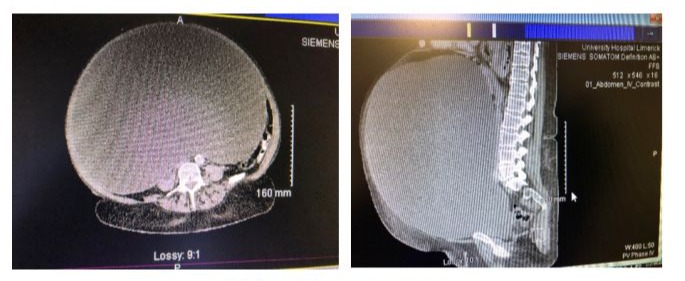
Figure 1 and 2: CT abdo-Pelvis
Intraoperative findings: At midline laparotomy, a large tight ovarian cyst filled the entire abdomen and was adherent to the normal peritoneum. The Omentum, liver, paracolic gutters and hemi diaphragms were all grossly normal. There were no palpable enlarged pelvic or para-aortic lymph nodes. The cyst was mobilised and decompressed of about 23litres of serous fluid and right oophorectomy completed after carefully dissecting off the significantly dilated right ureter. Omentectomy and appendectomy were done for full staging purposes. Estimated blood loss was 150mls. (Figure 3,4,5)

Figure 3: Pre-operative appearance

Figure 4: Immediate post-operative appearance

Figure 5: Ovarian cyst wall
She recovered well and was discharged home four days after surgery. On discharge she was 20kg lighter compared to her admission weight (95kg at admission vs 70.9kg at discharge). Her follow up appointment was uneventful six weeks post op. she reported significant improvement in her quality of life and five dress size change since the surgery. The histopathology report confirmed a benign ovarian Cystadenofibroma with unremarkable Omentum and Appendix.
Discussion and Conclusion
Cystadenofibroma is a rare form of benign ovarian cyst in contrast to cystadenoma which is more common. Serous Cystadenofibroma are the commonest subtype although others can occur, such as, endometroid, mucinous and clear cell type [5]. Epithelial proliferation and its degree to stromal component are the features used to classify the tumour as benign, borderline, and malignant. Risk factors for ovarian Cystadenofibroma are unknown, however high body weight and menopausal women on hormone replacement therapy are reported to have a higher risk [6] Clinical presentation is varied and vague including abdominal pain, distension, abdominal lump and infrequently urinary and/or bowel symptoms. Sometimes the large mass develops gradually over many years.
Pre-operative diagnosis is often difficult as the tumour mimics malignant features on radiological imaging due to their solid components. When imaged by ultrasonography or CT, ovarian Cystadenofibroma may appear as a complex solid and cystic mass and be difficult to differentiate from malignancy. Magnetic resonance imaging MRI may be an essential modality for diagnosis especially when the characteristic “black sponge” appearance is observed on T2-weighted images [7,8]. Frozen sections may be helpful in the intraoperative assessment of ovarian masses to provide guidance for appropriate surgical management; however, this is often time consuming or impractical, especially for a large specimen.
Cystadenofibroma rarely grow beyond 20 cm diameter, unlike Cystadenoma which have been reported to be as large as 80cm in size. A case report published reported a Cystadenofibroma of about 40cm which is the largest so far [9,10] and the highlighted concern is mainly compressive effects like bowel obstruction [11]. It is important to also consider such Adenofibromas when women present with large ovarian masses to avoid unnecessary radical surgeries. This case report represents what we think is the largest ovarian Cystadenofibroma ever reported.
References
- Czernobilsky B, Borenstein R, Lancet M. (1974) Cystadenofibroma of the ovary. A clinicopathologic study of 34 cases and comparison with serous cystadenoma. Cancer. 34: 1971–1981.
- Taheri H, Kholti MR, Hmila A, Saadi H, Mimouni A. (2020) Ovarian cystadenofibroma: a three cases report. Int J Reprod Contracept Obstet Gynecol. 9: 1728–1731.
- Singh P, Gothwal M, Yadav G, Ghuman NK. (2019) Cystadenofibroma of ovary: a rare case report. J South Asian Feder Menopause Soc. 7: 94–96.
- Wasnik A, Elsayes K. (2010) Ovarian cystadenofibroma: a masquerader of malignancy. Indian J Radiol Imaging. 20: 297–299.
- Wolfe SA, Seckinger DL. (1967) Various anatomical types of ovarian adenofibroma. Am J Obstet Gynecol. 99: 121–125.
- Lin HW, Tu YY, Lin SY, Su WJ, Lin WL, et al. (2011) Risk of ovarian cancer in women with pelvic inflammatory disease: a populationbased study. The Lancet Oncol. 12: 900–904.
- Outwater EK, Siegelman ES, Talerman A, Dunton C. (1997) Ovarian fibromas and cystadenofibromas: MRI features of the fibrous component. J Magn Reson Imaging. 7: 465–471.
- Takeuchi M, Matsuzaki K, Kusaka M, Shimazu H, Yoshida S, et al. (2003) Ovarian cystadenofibromas: characteristic magnetic resonance findings with pathologic correlation. J Comput Assist Tomogr. 27: 871– 873.
- Mc Nulty JR. (1999) The ovarian serous cystadenofibroma – A report of 25 cases. Am J Obstet Gynecol. 77: 133847.
- Colović R, Bandović J, Colović N, Grubor N. (2002) Giant cystadenofibroma of the ovary. Srp Arh Celok Lek. 130: 100–102.
- Mechera R, Menter T, Oertli D, Hoffmann H. (2016) Large ovarian cystadenofibroma causing large bowel obstruction in a patient with Klippel-Feil syndrome – A case report. Int J Surg Case Rep. 20: 17–20.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.