The Effectiveness of Burr Hole Surgery with a High Speed Drill for Chronic Subdural Hematoma: Technical Notes
by Yuichi Hirata1,2*, Yu Takahashi2, Akito Ikeda2, Yutaka Yamauchi2, Shingo Nishihiro2, Satoshi Kuramoto2, Eiji Iwado2, Yasuhiro Ono2, Shota Tanaka1, Tomotsugu Ichikawa2
1Department of Neurological Surgery, Okayama University Graduate School of Medicine, Dentistry and Pharmaceutical Sciences, Shikata cho, Kita-ku, Okayama, Japan
2Department of Neurological Surgery, Kagawa Prefectural Central Hospital, 1-chome-2-1 Asahimachi, Takamatsu, Kagawa 760-8557, Japan
*Corresponding author: Yuichi Hirata, Department of Neurological Surgery, Okayama University Graduate School of Medicine, Dentistry and Pharmaceutical Sciences, 700-8558 2-5-1, Shikata cho, Kita-ku, Okayama, Japan
Received Date: 20 September 2025
Accepted Date: 25 September 2025
Published Date: 27 September 2025
Citation: Hirata Y, Takahashi Y, Ikeda A, Yamauchi Y, Nishihiro S, et al. (2025) The Effectiveness of Burr Hole Surgery with a High Speed Drill for Chronic Subdural Hematoma: Technical Notes. J Surg 10: 11453 https://doi.org/10.29011/2575-9760.011453
Abstract
Conventionally, burr hole creation has been performed using a hand-cranked drill. However, this technique carries a risk of a complication known as plunging, defined as an uncontrolled, rapid increase in drilling depth, which can result in severe injury. With technological advancements, various devices for burr hole creation have been developed. Among them, the automatic-releasing cranial perforator is useful but expensive and still carries a risk of plunging. Since October 2020, we have used a high-speed drill for burr hole creation in over 100 patients with Chronic Subdural Hematoma (CSDH). This procedure offers several advantages. Trainees can become accustomed to using a high-speed drill, and it significantly reduces the risk of plunging and brain injury. In our experience with over 100 cases, we have not encountered any major complications. Additionally, the cost is lower than that of the perforator. The smaller burr hole created by the high-speed drill also provides a better cosmetic outcome and allows for effective drainage of CSDH. This technique offers clear benefits in terms of education, safety, cost-effectiveness, and cosmetic outcomes, with no major drawbacks. Here, we report on the effectiveness of burr hole surgery using a high-speed drill.
Keywords: Burr Hole Surgery; Chronic Subdural Hematoma; High Speed Drill; Perforator
Introduction
Historically, burr hole surgery was performed using a hand-cranked drill. According to a previous report, over 60% of neurosurgeons had experienced plunging with a hand-cranked drill, defined as an uncontrolled rapid increase in depth while using the drill or a perforator [1]. With technological advances, automatic-releasing cranial perforators have been developed. These drills stop automatically once the inner table of the skull is perforated [2]. They are very useful and are now widely used in most craniotomy procedures. However, their cost is significant, and this cannot be overlooked in burr hole surgery, which generally yields low profit margins. In some cases, we have also experienced failure in creating a burr hole with a perforator, requiring additional apparatus and thus incurring further cost. Since October 2020, we have performed burr hole creation using a high-speed drill for patients with Chronic Subdural Hematoma (CSDH). This method is more cost-effective than using a perforator, and also carries a lower risk of plunging. Trephining the skull is a fundamental skill in neurosurgical training, and this procedure allows trainees to become proficient with the high-speed drill. In this way, the technique also offers significant educational value. Here, we report the effectiveness of burr hole surgery using a high-speed drill.
Methods
Study Design
Patients who underwent surgery for CSDH with this procedure between October 2020 and December 2024 were included in this study. Patient demographics, including age, gender, affected side, bone thickness, operation time, diameter of the high-speed drill tip, complications, and cost, were investigated. Bone thickness was measured on coronal Computed Tomography (CT) images taken the day after surgery. In patients treated for bilateral CSDH, bone thickness was measured on both sides. Patients treated with drain placement only, without irrigation, were excluded from the study. Patients who underwent unilateral and bilateral surgeries were categorized into the unilateral and bilateral groups, respectively.
Statistical Analysis
Age was presented as the mean ± standard deviation, while bone thickness, operation time, and affected side percentages were presented as medians with interquartile ranges. Statistical analysis was performed using Prism 10 (GraphPad Software, San Diego, CA, USA). Data normality was assessed using the Shapiro-Wilk normality test. Spearman’s rank correlation was used to evaluate the correlation between bone thickness and operation time. The Kruskal-Wallis test was used to compare operation times between 4 mm and 6 mm drill tips. A p-value of less than 0.05 was considered statistically significant. This study did not require ethics committee, Institutional Review Board (IRB) approval, nor informed consent from participants, because it is a retrospective technical report based on routine clinical practice, with no prospective data collection or experimental intervention. All data were anonymized and analyzed in aggregate.
Operative Procedure
As with standard burr hole surgery for CSDH, the patient’s head is secured on a horseshoe pillow. Under local anesthesia, a linear skin incision is made on the affected side. After opening the incision with a scalpel, the burr hole is created using a high-speed drill is performed. The surgeon holds the high-speed drill in the right hand and the suction tube in the left (Figure 1). A burr hole with a diameter of about 10 mm is made. The assistant irrigates the site with water during drilling to maintain visibility. The high-speed drill is applied to the skull vertically to create an initial groove. Once a certain depth is reached, the high-speed drill is rotated in a circular motion to shave off the surrounding bone. The surgeon perceives a change in resistance when transitioning from the outer to the inner table. As the bone becomes thinner, the dura mater becomes visible through the remaining bone. Because the drill tip is 4 or 6 mm in diameter, preoperative measurement of bone thickness allows the surgeon to anticipate the depth required during the procedure. Once the dura mater is visible, continuing to drill vertically helps avoid dural injury. A spatula is sometimes used to carefully remove the inner table. Once the dura mater is fully exposed, standard drainage for CSDH is performed (Figure 2).
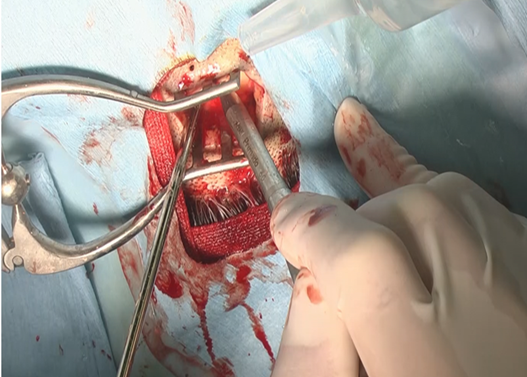
Figure 1: Burr hole creation using a high-speed drill, The surgeon holds the high-speed drill in the right hand and the suction device in the left hand (A).
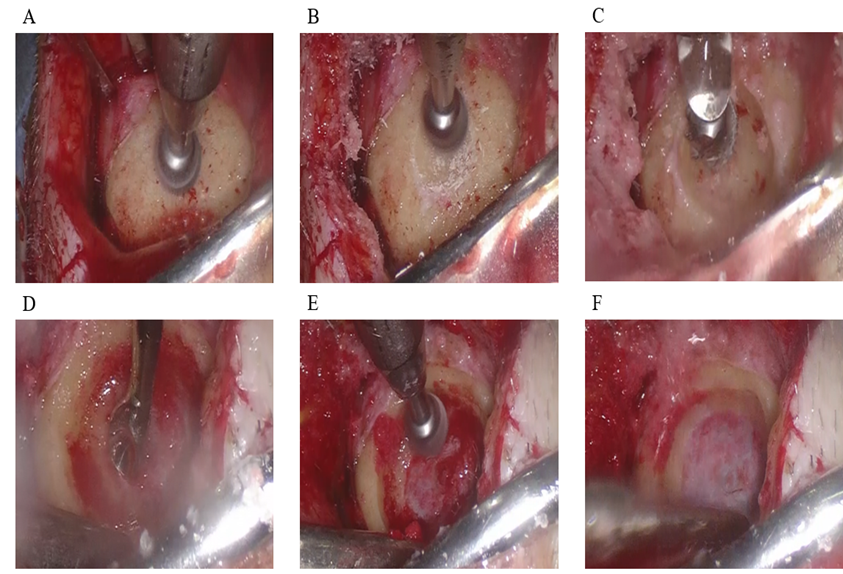
Figure 2: Burr hole creation using a high-speed drill, The high-speed drill is first applied vertically to the skull (A) to create an initial groove (B). Once a certain depth is reached, the drill is rotated in a circular motion (C). A spatula is sometimes used to carefully remove the inner table (D). Operating the drill vertically helps avoid injury to the dura mater (E). The dura mater is finally exposed (F).
Results
We performed 129 surgeries for CSDH patients using this technique between October 2020 and December 2024. Of these, 118 cases (91.5%) were unilateral and 11 cases (8.5%) were bilateral. The mean patient age was 78.9 ± 12.1 years, and 87 patients (67.4%) were men. In the unilateral group, 74 cases (62.7%) were on the left side. Median bone thickness was 8.7 (7.6-9.9) mm, and median operation time was 38 (33-45) min. In this group, 87 cases (73.7%) were performed using a 4 mm drill tip, and 31 cases (26.3%) with a 6 mm drill tip. In the bilateral group, the median bone thickness was 8.9 (7.6-9.3) mm, and median operation time was 67 (52-80) min. Only one case (9.1%) in this group was treated with a 6 mm drill tip. As an intraoperative complication, dural damage with sudden hematoma release occurred in two cases treated with a 4 mm drill tip in the unilateral group. However, no postoperative neurological deficits were observed. Clinical data are summarized in Table 1.
|
number of patients |
129 |
|
age (mean ± SD) |
78.9 ± 12.1 |
|
man (%) |
87 (67.4) |
|
left (%) |
74 (57.4) |
|
right (%) |
44 (34.1) |
|
bilateral (%) |
11 (8.5) |
|
bone thickness (mm) |
8.7 (7.6-9.9) |
|
operation time (min) |
|
|
unilateral |
38 (34-45) |
|
bilateral |
67 (52-80) |
|
diameter of the high-speed drill tip |
|
|
6 mm |
32 (24.8) |
|
4 mm |
97 (75.2) |
|
complication (%) |
2 (1.6) |
M: Male; Lt: Left; Rt: Right; Bil: Bilateral
Table 1: Patients characteristics.
In the unilateral group, no significant correlation was found between operation time and bone thickness (p = 0.24), nor was there a significant difference in operation time between 4 mm and 6 mm drill tips (p = 0.056). Similarly, in the bilateral group, no correlation was observed between operation time and bone thickness (p = 0.42). Cost comparisons for burr hole creation using hand-cranked drills, perforators, and high-speed drills are shown in Table 2. A hand-cranked drill (MIZUHO MEDY Co. Ltd., Saga, Japan) costs 150,000 yen in Japan and can be re-used for a long period. A reusable perforator and disposable perforator (ACRA-CUT; MC Medical, Tokyo, Japan) cost 530,000 yen and 38,990 yen, respectively. High-speed drill tips (Midas Rex; Medtronic, Dublin, Ireland) cost 17,500 yen (4 mm) and 18,500 yen (6 mm). Although high-speed drills are more expensive than hand-cranked drills, they are cheaper than perforators. Creating a burr hole with a high-speed drill takes approximately 1 to 2 min, longer than with a perforator, but faster than with a hand-cranked drill.
|
apparatus |
cost (yen) |
|
hand-cranked drill (MIZUHO MEDY Co. Ltd.) |
1,50,000 |
|
reuse perforator (ACRA-CUT, MC medical) |
5,30,000 |
|
disposable perforator (ACRA-CUT, MC medical) |
38,990 |
|
cutting burr (4mm) (Midas Rex, Medtronic) |
17,500 |
|
cutting burr (6mm) (Midas Rex, Medtronic) |
18,500 |
Table 2: Comparison of the cost between Hudson hand drill, perforator, and high speed drill.
Discussion
CSDH is a neurological disorder that predominantly affects the elderly and is associated with serious morbidity and mortality. Burr hole surgery with hematoma drainage is a commonly performed treatment for this condition [3,4]. Historically, burr hole surgery was performed using a hand-cranked drill, but this technique carries the risk of complications during the drilling process. According to a previous report based on an anonymous postal questionnaire sent to 304 neurosurgeons in Britain and Ireland, 65.6% of respondents had experienced plunging. In addition, 22.3% had experienced plunging at least twice. In 79% of cases, the dura mater was penetrated during the plunging incident, indicating that it is not a rare complication [1]. They also reported that 12% of patients who experienced plunging suffered severe complications such as intracerebral hematoma, cortical laceration, or death. In most cases, a hand-cranked drill was used.Another study reported nine cases of plunging in 1,652 (0.54%) burr hole procedures using automatic-releasing cranial perforators [5]. Although no complications occurred in these cases, the risk suggests that even automatic-releasing cranial perforators are not entirely safe. Zolnourian et al. reported predictors of clinical outcomes, complications, and hospital length of stay in patients undergoing burr hole surgery for CSDH [6]. Factors such as age less than 80 years, preadmission independence, preoperative Glasgow Coma Scale motor score of 6, and taking fewer than 5 regular medications were associated with significantly better outcomes and being discharged home. In addition, they also correlated with lower rates of postoperative complications and shorter hospital stays.
In contrast, surgical variables such as laterality and the number of burr holes were not associated with outcomes. Another study reported that male gender, bilateral hematoma, and low drainage volumes were significantly associated with reccurence [7]. Stachys et al. performed a comparative analysis of surgical techniques for CSDH and identified risk factors for poor outcomes. They compared burr hole surgery and minicraniotomy [8]. The rates of recurrence, postoperative complications, death, and poor long-term outcomes did not differ significantly between the two procedures. According to a similar report, however, minicraniotomy was significantly associated with complications [9]. A smaller range of bone shaving may therefore be favorable for CSDH surgery. To the best of our knowledge, no previous study has explored the correlation between operation time and bone thickness. In this study, no such correlation was observed in either the unilateral or bilateral groups, suggesting that variations in bone thickness do not affect operation time. Hwang reported that a site 1 cm anterior to the coronal suture at the level of the superior line is a suitable entry point for burr hole surgery for CSDH, based on hematoma thickness and the location of the middle meningeal artery [10]. At this site, bone thickness was reported to be 8 (5-13) mm. Several reports have compared twist drill craniotomy and burr hole surgery for patients with CSDH [11-13].
However, the results have been inconsistent, and the effectiveness of twist drill craniotomy remains controversial. In our experience of 129 burr hole surgeries using a high-speed drill, we have not encountered any cases of plunging or major complications. This procedure offers several advantages. First, it provides an educational benefit for trainees, allowing them to gain experience using a high-speed drill in a safe and controlled setting. Second, the likelihood of plunging and damaging the brain is low. While we encountered two cases of dural injury, no postoperative complications occurred. In addition, as the dura mater is often shrunken in conventional surgery for CSDH, it is not considered a serious issue. Third, it is cost-effective. Although high-speeds drill are more expensive than hand-cranked drills, they are less costly than disposable perforators. For example, a high-speed drill tip costs 17,500 yen, compared to 38,990 yen for a disposable perforator, resulting in a saving of 21,490 yen per surgery. Fourth, while there may be concern about patient head movement, it is not necessary to fix the patient’s head rigidly during the drilling process, which may reduce patient distress. Fifth, because the drill tip has a fixed diameter (4 mm or 6 mm), the surgeon can accurately estimate the depth of the burr hole. Sixth, only a small burr hole is needed to drainage CSDH effectively. For instance, Codman perforators produce burr holes of 9, 11, or 14 mm in diameter, depending on the size used. The hole created with a high-speed drill can be smaller, which is more cosmetically favorable. Seventh, while burr hole creation using a perforator can sometimes fail mid-procedure and require further equipment, we have never experienced such a failure using a high-speed drill. As disadvantages, certain points should be carefully considered. Bone dust generation is inevitable, and the procedure takes slightly longer than with a perforator. However, according to our results, the time difference is not significant and is unlikely to pose a major concern. In addition, patient movement during drilling can be dangerous, so light anesthesia is needed in such cases. This study has several limitations. First, bone thickness was measured using coronal CT images; while three-dimensional measurement is desirable, it was not performed. Second, multiple surgeons conducted the procedures, so the choice of drill tip diameter may reflect operator preference, introducing potential selection bias. Although no correlation was found between operation time and drill tip diameter, surgeries using the 6 mm tip tended to have shorter durations. This may have been influenced by the individual surgeon’s technique. Third, the educational benefit for trainees was not assessed using objective measures. In summary, this procedure offers advantages in terms of trainee education, safety, cost, and cosmetic outcome. Additionally, it eliminates the need for additional apparatus to create the burr hole. Furthermore, there are no significant disadvantages. For these reasons, we consider this procedure to be effective.
Conclusion
Burr hole surgery with a high-speed drill is effective in terms of education, safety, cost-effectiveness, and cosmetic outcomes.
Conflicts of Interest Disclosure: The authors have no conflicts of interest concerning the materials or methods used in this study or the findings reported in this paper.
References
- Caird JD, Choudhari KA (2003) “Plunging” during burr hole craniostomy: A persistent problem amongst neurosurgeons in Britain and Ireland. British Journal of Neurosurgery 17: 509-512.
- Smith GW (1950) An automatic drill for craniotomy. J Neurosurg 3: 285-286.
- Asghar M, Adhiyaman V, Greenway MW, Bhowmick BK, Bates A (2002) Chronic subdural haematoma in the elderly--a North Wales experience. J R Soc Med 95: 290-292.
- Baechli H, Nordmann A, Bucher HC, Gratzl O (2004) Demographics and prevalent risk factors of chronic subdural haematoma: Results of a large single-center cohort study. Neurosurgical Rev 27: 263-266.
- Vogel TW, Dlouhy BJ, Howard MA (2011) Don’t take the plunge: Avoiding adverse events with cranial perforators: Clinical article. J Neurosurg 115: 570-575.
- Zolnourian A, Manivannan S, Edwards B, Chua A, Arora M, et al. (2025) Factors affecting outcomes following burr hole drainage of chronic subdural hematoma: a single-center retrospective study. J Neurosurg 142: 1606-1615.
- Zhu F, Wang H, Li W, Han S, Yuan J, et al. (2021)Factors correlated with the postoperative recurrence of chronic subdural hematoma: An umbrella study of systematic reviews and meta-analyses. EClinicalMedicine 43: 101234.
- Hounkpatin S, Stierer M, Frechon P, Rault F, Kelani A, et al. (2024) Comparative analysis of surgical techniques in the management of chronic subdural hematomas and risk factors for poor outcomes 47: 254.
- Zolfaghari S, Bartek J Jr, Strom I, Djärf F, Wong SS, et al. (2021) Burr hole craniostomy versus minicraniotomy in chronic subdural hematoma: a comparative cohort study. Acta Neurochir (Wien) 163: 3217-3223.
- Hwang SC, Im SB, Kim BT, Shin WH (2009) Safe entry point for twist-drill craniostomy of a chronic subdural hematoma: Clinical article. J Neurosurg 110: 1265-1270.
- Wang K, Chen D, Cao X, Gao L (2017) A prospective comparative study of twist drill craniostomy versus burr hole craniostomy in patients with chronic subdural hematoma. Turk Neurosurg 27: 60-65.
- Gökmen M, Sucu HK, Ergin A, Gökmen A, Bezircio Lu H (2008) Randomized comparative study of burr-hole craniostomy versus twist drill craniostomy; Surgical management of unilateral hemispheric chronic subdural hematomas. Zentralbl Neurochir 69: 129-133.
- Horn EM, Feiz-Erfan I, Bristol RE, Spetzler RF, Harrington TR (2006) Bedside twist drill craniostomy for chronic subdural hematoma: A comparative study. Surg Neurol 65: 150-153.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.