The COVID-19 Pandemic and Health Care Utilization Evidence from Austrian Register Data
by Wolfgang Frimmel1*, Gerald J. Pruckner1,2
1Johannes Kepler University Linz, Austria
2Christian Doppler Laboratory for Aging, Health, and the Labor Market, Austria
*Corresponding author: Wolfgang Frimmel, Department of Economics, Johannes Kepler University, Linz, Altenberger str. 69, A-4040 Linz, Austria
Received Date: 23 October, 2025
Accepted Date: 31 October, 2025
Published Date: 05 November, 2025
Citation: Frimmel W, Pruckner GJ (2025) The COVID-19 Pandemic and Health Care Utilization Evidence from Austrian Register Data. J Community Med Public Health 9: 541. https://doi.org/10.29011/2577-2228.100541
Abstract
The outbreak of the COVID-19 pandemic had an enormous impact on social and economic life and in particular. for human health care. In this paper, we document the impact of the COVID-19 pandemic and its accompanying policies on individual health care utilization. We use detailed administrative health registry data for Upper Austria for the years 2019 to 2021 and estimate the change in outpatient and inpatient health care utilization after the pandemic outbreak in March 2020 in a dynamic differences-in-difference setting. We document significant collateral damage to the health care system. While the number of outpatient visits and expenditures stabilized a few months after the outbreak, inpatient care decreased significantly and continued to decline during the subsequent quarantine periods. Chronically ill patients stocked up on necessary medications at the onset of the pandemic and the number of drug prescriptions steadily increased as the pandemic progressed. Spending on inpatient care and new diagnosis for cardiovascular disease and cancer dropped significantly below 2019 levels during the lockdown periods and many orthopaedic, cataract, and vein procedures were either postponed or not performed. Finally, we find clear evidence of deteriorating mental health over the course of the pandemic.
JEL Classification: I11, I12, H51
Keywords: COVID-19 pandemic; Health care utilization; Collateral damage; Differences- in-difference
Introduction
The outbreak of the COVID-19 pandemic has had a profound impact on social and economic life. In addition to the dramatic loss of life, major challenges arose in the labor market. Businesses were threatened and many people were affected by unemployment and the loss of their livelihoods. In addition, the pandemic has negatively affected national and international food chains through border closures, trade barriers or other coercive measures1.
Naturally, the pandemic has had a particularly severe impact on human health care. With the need to treat large numbers of COVID19-infected patients with severe and very severe disease, the health systems of almost all countries have reached their capacity limits. When these were reached, other treatments could not be offered, or could only be offered with a time delay. Such collateral damage has also occurred because hospitals, in anticipation of new waves of COVID infection, have reduced their services in advance and reserved capacity for COVID patients in normal and intensive care units (see Mira and Lorenzo (2021) and the literature cited therein for an overview). In addition to these re- ductions in health care services, a pandemic-related change in patient health care behavior has been observed. Fear of being infected with COVID-19 has led patients to reduce out- patient visits to physicians and hospitals and to avoid unnecessary hospitalizations. Such behavioral changes have been documented mainly for the first wave(s) of the pandemic (see, e.g., Czeisler et al. (2020), Zhang (2021))2.
In this paper, we analyze the use of health care services during a pandemic in Austria using comprehensive individual-level data from the Upper Austrian health registers. Using a dynamic differences-in-difference design, we compare inpatient and outpatient service utilization in the pandemic years 2020 and 2021 with that in 2019, controlling for seasonal influences. Our analysis focuses on the collateral damage of the pandemic and its accompanying measures, such as hospital closures and treatment restrictions. We look at trends over time for three different groups of services: (i) treatment of life-threatening conditions such as cancer and major cardiovascular disease, (ii) elective hospital procedures, and (iii) mental health. The comprehensiveness of the data available allows detailed analysis of all components of health care, including pharmaceuticals and preventive services.
We find that health care spending declined significantly with the onset of the pandemic. While spending on outpatient visits stabilized after June 2020, inpatient care continued to decline significantly during the subsequent lockdowns, as hospitals held capacity in reserve in anticipation of the impending waves of infection. Chronically ill patients stocked up on necessary medications at the onset of the pandemic. As the pandemic progressed, we saw a steady increase in the number of prescriptions, which was possible despite restrictions on doctor visits due to the increased use of e-medication. Spending on inpatient care for cardiovascular disease and cancer dropped significantly below 2019 levels during the lock- down periods which was also reflected in a decrease of first-time diagnoses of myocardial infarction and new cancer diagnoses.
We also provide clear evidence of non-life-threatening collateral damage. Many orthopaedic procedures have been postponed or not performed. The same is true for cataract and venous care. Finally, we find clear evidence of deteriorating mental health over the course of the pandemic, as documented by the significant and sustained increase in the use of psychotropic drugs from June 2020 to the end of the pandemic.
Literature: The literature on the impact of the pandemic and its accompanying measures on health and health care utilization is extensive. Many studies focus on individual countries and regions or on the impact of the pandemic on specific patient groups and diseases. Methodologically, most analyses use difference-indifferences approaches and event study designs.
Mulligan and Arnott (2022) report that Americans died from nonCOVID causes at an annual rate of nearly 100,000 above previous trends between April 2020 and the end of 2021. Hypertension, myocardial infarction, diabetes, obesity, alcohol abuse, and especially an alarming increase in drug-related deaths are cited as major causes of the excess deaths. While COVID-19 deaths predominantly affected older populations, the absolute numbers of non-COVID excess deaths are very similar in the 18-44, 4564, and over 65 age groups3. In addition to its impact on excess mortality, the COVID-19 pandemic outbreak was associated with significant changes in health care utilization.
Already in July 2020, Ziedan, et al. (2020) publish a working paper on the evolution of non-COVID care in the U.S. since early March 2020. The authors analyze data from a national electronic health record system with more than 35 million patients. Using difference-in-differences and event study approaches, they find that state closure policies have significantly reduced outpatient visits. The aggregate trend in outpatient visits is reported to decline by 40% after the first week of 2020, with more than one-third of the decline attributable to state policies. The authors also report a rebound around mid-April 2020, with visits remaining below prepandemic levels through July 2020.
In his analysis of electronic health record data from approximately 9 million patients from the U.S. Veteran’s Health Administration Corporate, Zhang (2021) documents a reduction in emergency department and inpatient hospital visits by 37 and 46%, respectively, between mid-March and early May 2020. By the end of October 2020, the reductions were still 10 and 17%, respectively. He also reports a 19.5% increase in veteran mortality during the first two months of the pandemic, with an estimated 7.9% of the excess deaths due to hospital avoidance.
Using employer-sponsored insurance data for more than 6 million people in the US and cell phone data, Cantor et al. (2022) find that the introduction of social distancing policies was also associated with a reduction in preventive and elective care with the onset of the pandemic. When the endogeneity of policy implementation was taken into account, the impact of these policies was reduced. Based on a sample of more than 14.5 million U.S. adults, Mafi et al. (2022) provide evidence that overall use of ambulatory care services increased to pre-pandemic levels between March 2020 and February 2021, after an initial decline following the onset of the COVID-19 pandemic.
In their remarkable review of the direct and indirect health effects of the COVID-19 pandemic in the United States, Alsan, et al. (2021) address the disparities in the impact on different populations. Older age groups were found to be particularly vulnerable, and age- related COVID-19 mortality rates were higher among historically disadvantaged groups such as blacks, Hispanics, and American Indians4.
Fetzer and Rauh (2022) support findings that the COVID-19 pandemic had significant adverse effects on the accessibility and quality of non-COVID-19 care. Using individual- level public administrative data from the NHS in England, the authors provide evidence of a sharp decline in accident and emergency (A&E) attendances during the first wave of the pandemic, limited access to specialist care, and delayed or even inaccessible diagnostic services. In addition, the authors document impaired access to and quality of cancer care and more excess deaths for non-COVIDrelated hospital episodes. Using administrative data from a large prefecture-level city in China, Huang and Liu (2023) analyze the impact of the pandemic and related policies and find reductions in outpatient care utilization. The largest decrease during the lockdown period is reported for preventive care visits.
Several reviews examine the impact of the COVID-19 pandemic on health service utilization in a number of low, middle, and highincome countries. The data and studies included in these reviews confirm that health care utilization for non-COVID-19 conditions decreased almost universally, with varying degrees of disruption in service delivery depending on the type of disease, national income levels, or the severity of the pandemic and its accompanying policies (Arsenault et al., 2022; Roy et al., 2021; Moynihan et al., 2021)5.
The pandemic revealed another interesting trend in the use of medical services. While face-to-face visits decreased sharply with the onset of the pandemic, there was a huge increase in virtual visits (see, for example, Fu et al. (2022) and Hatef et al. (2022)). Reges et al. (2022) present the main socio-economic and demographic factors associated with the use of telemedicine.
Special attention will be given to the impact of the pandemic on mental health. This includes psychiatric problems directly related to COVID-19 infection (direct effect) and the impact of the pandemic and its accompanying measures on the mental health of the general public (indirect effect). In their systematic review of the literature containing evidence for both effects, Vindegaard and Benros (2020) find high levels of post-traumatic stress symptoms and significantly higher levels of depressive symptoms in patients with COVID-19. The studies included in the review on the mental health of the general population show lower levels of psychological well-being and higher levels of anxiety and depression compared to pre-pandemic levels. Female gender, poor self-reported health, and COVID-19-infected relatives are reported to be the most important factors associated with a higher risk of psychiatric symptoms. For a selection of studies on the impact of the pandemic on mental health in high- and low-income countries, see for example Aknin et al. (2022), Pierce et al. (2021), Raina et al. (2021), Beutel et al. (2021), Varga et al. (2021) and Aksunger et al. (2023). The studies confirm that anxiety, depression and distress increased in the early months of the pandemic and that symptoms of mental disorders remained largely stable as the pandemic progressed6.
While the literature is growing continuously, most studies remain rather segmented and consider specific elements of a health care system in partly non-representative samples. Therefore, we can contribute in two ways: first, the use of administrative health register allows us to analyze the change and potential collateral damages from the pandemic for a full population, therefore having high external validity. Second, due to the richness of our data and in particular the combination of inpatient and outpatient data for the identical population we can study the impact of the pandemic in a very comprehensive way, i.e. life-threatening diseases and elective procedures in the inpatient sector, or drug prescriptions, medical attendance and health behavioral aspects such as screening in the outpatient sector.
Data and Institutional Background
The Austrian Health Care System and the COVID Crisis
Austria has a Bismarckian health care system that guarantees the population free access to high-quality health care services. Social health insurance covers the cost of hospitalization, visits to general practitioners and specialists, and medicines. The outpatient sector is financed by income-related social security contributions from employees and employers, while inpatient stays are covered by social security contributions and taxes at various federal levels. Under the umbrella of the Austrian Health Insurance Fund (Osterreichische Gesundheitskasse), nine regional health insurance funds provide compulsory insurance for all employees and their dependents. There is no free choice of health insurance fund; assignment to the regional fund depends on the province in which the employer is located. The insured group of employees represents about 75 to 80% of the Austrian population7. Access to services is generally free, with only moderate deductibles for drugs and hospitalization.
The COVID crisis in (Upper) Austria: Figure 1 shows the timeline of infections and related infection control measures in Upper Austria. The first viral infections in Austria were registered on February 25, 2020. On March 16, 2020, a nationwide lockdown was imposed, which, in addition to the closure of schools and universities, included significant travel restrictions, the cancellation of events, the closure of all businesses not necessary for basic services, the closure of restaurants from 15:00, and a general curfew. There was also an obligation to maintain social distance and to wear face masks. The nationwide lockdown was gradually relaxed starting on Easter 2020 and was completely lifted on May 1, 2020. As shown in Figure 1, a second wave of infection occurred between November 2020 and January 2021, which was initially countered by mandatory face masks in public indoor spaces, and later by a second and third lockdown, again with exit restrictions, followed by voluntary mass testing of the entire population. The vaccination campaign against COVID began in early 2021.
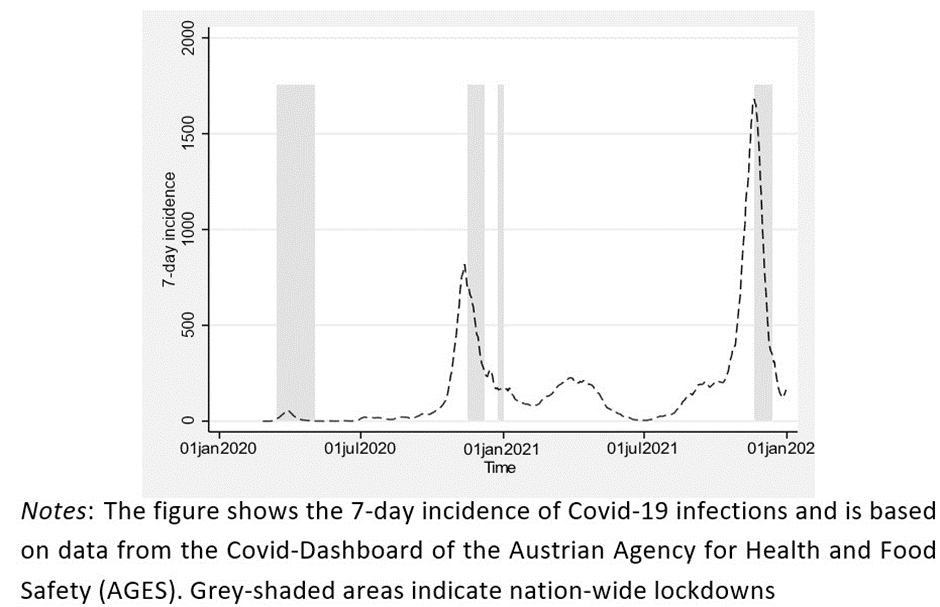
Figure 1: Timeline and infections in Upper Austria.
While there was a renewed but moderate increase in the number of infections in March and April 2021, the fourth and strongest wave of infections began in September 2021 with over 15,000 new infections per day all over Austria. The peak daily number of new infections in the province of Upper Austria was 1,700. The general quarantine that had been in place since late November was lifted on December 12 for vaccinated and recovered persons. Mandatory vaccination went into effect in February 2022, but was not enforced.
During the pandemic, suspected cases and infected persons were isolated and placed in home quarantine by order of the health authorities. Patients were referred to hospitals for acute medical treatment of COVID cases. Hospitals prepared for the increase in infections by setting up isolation wards and quarantine areas. Although Austria has a high number of intensive care beds relative to the population, with an average long- term occupancy rate of about 80 %, there was a risk that intensive care units would reach capacity during the pandemic. So, countermeasures such as increasing the number of ICU beds by 20 %, significantly reducing non-acute hospital operations or temporary closure of mainly elective hospital departments were implemented to provide additional COVID capacity.
In addition to the precautions taken in the inpatient sector, the number of contacts with outpatient physicians was significantly reduced. Two measures that supported this development were the possibility to prescribe medication and to issue sick notes by telephone.
In Upper Austria, similar to the country as a whole, massive excess mortality was observed in the second and fourth waves of infection. In calendar weeks 43 to 53 of 2020, the number of deaths among people over 65 was more than 40% higher than in the long- term comparison period (Land Oberosterreich, 2022). By the end of 2021, the excess deaths were again very high. However, the percentage increases were lower than in the second COVID wave.
Data
To empirically analyze the impact of the COVID pandemic on health care utilization, we use extensive individual data from the inpatient and outpatient health registries of Upper Austria. The Upper Austrian Health Insurance Fund provides extramural claims data for 1.3 million insured persons employed in the province of Upper Austria. These data include detailed information on the use of medical services (general practitioners and specialists) as well as the prescription of drugs, including ATC (Anatomical Therapeutic Chemical Classification) drug groups. The data on inpatient stays come from the Upper Austrian Hospital Fund. They include the admission diagnoses according to the ICD-10 system, the length of stay, and the billed DRG (diagnosis-related-group) points. The intra- and extramural data are linked by a pseudonymized social security number. We construct an individual-level monthly panel over the period 2019 to 2021 ending up with 44,612,914 observations of 1,469,616 individuals.
Estimation strategy
Descriptively, one could compare averages in health care expenditures over time to assess the change in utilization around the onset of the pandemic. Such an approach, however, would completely neglect the seasonality in health care utilization, i.e. respiratory diseases are more common in winter season relative to cardiovascular diseases. In order to account for seasonality, we estimate an empirical model in the spirit of a dynamic differencesin- difference model with the pre-pandemic year 2019 as a control period. More specifically, we estimate health care expenditure Y for an insured person i in month j of year k:
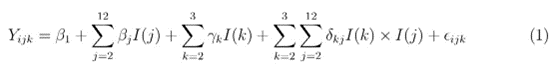
I(j) and I(k) denote dummy variables for calendar months and years, respectively. In our estimations we choose January as the baseline month. The coefficients of interest are δkj. The interaction effects of month and year reflect the difference in spending for a given month in a pandemic year (2020 and 2021) compared to spending for the same month in the pre-pandemic year 2019. The comparison with the year 2019 controls for seasonal effects on the level of health care spending. We need to assume that the pre-pandemic year of 2019 serves as a valid counterfactual period and was not affected by different seasonal patterns8. Since the year 2021 is fully associated with the pandemic, and the year indicators measure the difference in outcomes between January 2019 and the respective year, the year dummy for 2021 will therefore not only capture a yearly trend in outcomes but also incorporate a change in outcomes due to the pandemic as well. This would imply that the interaction terms alone are likely underestimating the true change in health care utilisation due to the pandemic. In our analysis, we will therefore consider the sum of γk and δkj and interpret our findings solely as the change in outcomes relative to the prepandemic period of 2019.
Results
Outpatient and inpatient service utilization
With the onset of the pandemic, there was a significant reduction in hospital services, while spending on medicines increased. After a slight decrease in the first year of the pandemic, spending on outpatient physician services also increased significantly. Table 1 contains descriptive statistics for the years 2019 to 2021. It shows that in 2021, spending on physician visits and drugs was 9 and 13% higher, respectively, than in the last year before the pandemic. In the inpatient sector, total services (measured in billed DRG points) decreased by 8.2% over the same period. This reduction was accompanied by a decrease in the number of hospital days of more than 10%, while the amount of inpatient spending (total revenues transferred to hospitals) decreased by only 2.1%9. In contrast, hospital outpatient spending decreased only in the first year of the pandemic, while increasing by 3.5 % in 2021, in line with the overall trend in outpatient spending.
|
2019 |
2020 |
2021 |
Diff. [%] 2020- 2019 |
Diff. [%] 2021- 2019 |
||||
|
Individual characteristics |
||||||||
|
Age |
40.5 |
40.6 |
41.1 |
|||||
|
Female |
0.498 |
0.498 |
0.497 |
|||||
|
Foreign |
0.204 |
0.207 |
0.208 |
|||||
|
Number of first cancer diagnosesa |
0.00047 |
0.00044 |
0.000464 |
-6.4 |
-1.3 |
|||
|
First cancer diagnoses (high 5-yr survival)a |
0.00029 |
0.00028 |
0.00029 |
-6.0 |
0.3 |
|||
|
First cancer diagnoses (low 5-yr survival)a |
0.000172 |
0.000160 |
0.000165 |
-7.0 |
-4.1 |
|||
|
Number of first AMI diagnosesa |
0.00001 |
0.00001 |
0.00001 |
-8.5 |
-14.1 |
|||
|
Number of first stroke diagnosesa |
0.0001 |
0.0001 |
0.0001 |
-3.6 |
0.0 |
|||
|
DRG points aggregatedb |
1.55E09 |
1.37E09 |
1.42E09 |
-11.8 |
-8.2 |
|||
|
Hospital daysa |
0.11 |
0.10 |
0.099 |
-9.4 |
-10.1 |
|||
|
Inpatient expenditures |
85.08 |
81.40 |
83.33 |
-4.3 |
-2.1 |
|||
|
Hospital outpatient expenditures |
16.71 |
16.21 |
17.29 |
-3.0 |
3.5 |
|||
|
Outpatient doctor expenditures |
38.13 |
37.79 |
41.56 |
-0.9 |
9.0 |
|||
|
Medication expenditures |
26.32 |
27.37 |
29.78 |
4.0 |
13.1 |
|||
|
Inpatient expenditures |
||||||||
|
Neoplasms |
12.96 |
12.84 |
12.74 |
-0.9 |
-1.7 |
|||
|
Myocardial infarction |
0.906 |
0.841 |
0.814 |
-7.2 |
-10.2 |
|||
|
Cardiac arrest |
0.118 |
0.112 |
0.0915 |
-5.1 |
-22.5 |
|||
|
Stroke |
1.493 |
1.580 |
1.561 |
5.8 |
4.6 |
|||
|
Endoprosthetics |
3.97 |
2.912 |
3.044 |
-26.6 |
-23.3 |
|||
|
Cataracts senilis |
0.976 |
0.880 |
1.174 |
-9.8 |
20.3 |
|||
|
Other cataracts |
0.302 |
0.164 |
0.119 |
-45.7 |
-60.6 |
|||
|
Varicose veins |
0.421 |
0.275 |
0.252 |
-34.7 |
-40.1 |
|||
|
Mental and behavioral disorders |
3.49 |
5.222 |
5.131 |
49.6 |
47.0 |
|||
|
Outpatient expenditures |
||||||||
|
GP |
10.12 |
10.44 |
11.91 |
3.2 |
17.7 |
|||
|
Neurology/Psychiatry |
0.881 |
0.866 |
0.903 |
-1.7 |
2.5 |
|||
|
Psychotherapy and psychology |
0.791 |
0.816 |
0.820 |
3.2 |
3.7 |
|||
|
Medication expenditures |
||||||||
|
Nervous system |
3.292 |
3.454 |
3.768 |
4.9 |
14.5 |
|||
|
Antidepressants |
0.605 |
0.582 |
0.558 |
-3.8 |
-7.8 |
|||
|
Migraine drugs |
0.0818 |
0.119 |
0.172 |
45.5 |
110.3 |
|||
|
Anxiolytic drugs |
0.0317 |
0.0273 |
0.0251 |
-13.9 |
-20.8 |
|||
|
Screening participationa |
||||||||
|
General health check |
0.0155 |
0.0137 |
0.0167 |
-11.6 |
7.7 |
|||
|
Mammography |
0.00450 |
0.00414 |
0.00511 |
-8.0 |
13.6 |
|||
|
Colposcopy |
0.0186 |
0.0171 |
0.0176 |
-8.1 |
-5.4 |
|||
|
PSA |
0.00848 |
0.00808 |
0.00976 |
-4.7 |
15.1 |
|||
|
Individuals |
1,469,616 |
|||||||
|
Observations |
44,612,914 |
|||||||
|
Notes: Expenditures in € per capita and month; a per month; b per year. |
||||||||
Table 1: Descriptives.
Figure 2 shows the development of service utilization over time during the pandemic10. The estimation results of equation (1) show that expenditures for outpatient physician visits (panel a), inpatient hospital care (panel c), and hospital outpatient services (panel d) decreased significantly with the onset of the pandemic. In quantitative terms, these decreases ranged from 30% (inpatient and outpatient hospital expenditures) to 45%. While physician services reached and even exceeded their pre-pandemic levels by June 2020, hospital inpatient services experienced further significant declines during the subsequent lockdown periods with their imposed supply reductions.
Medication use (panel b) shows a significant increase with the onset of the pandemic in March 2020. The subsequent decline in prescriptions was followed by a significant increase of more than 10 % from June 2020. Overall, the pandemic did not reduce drug use.
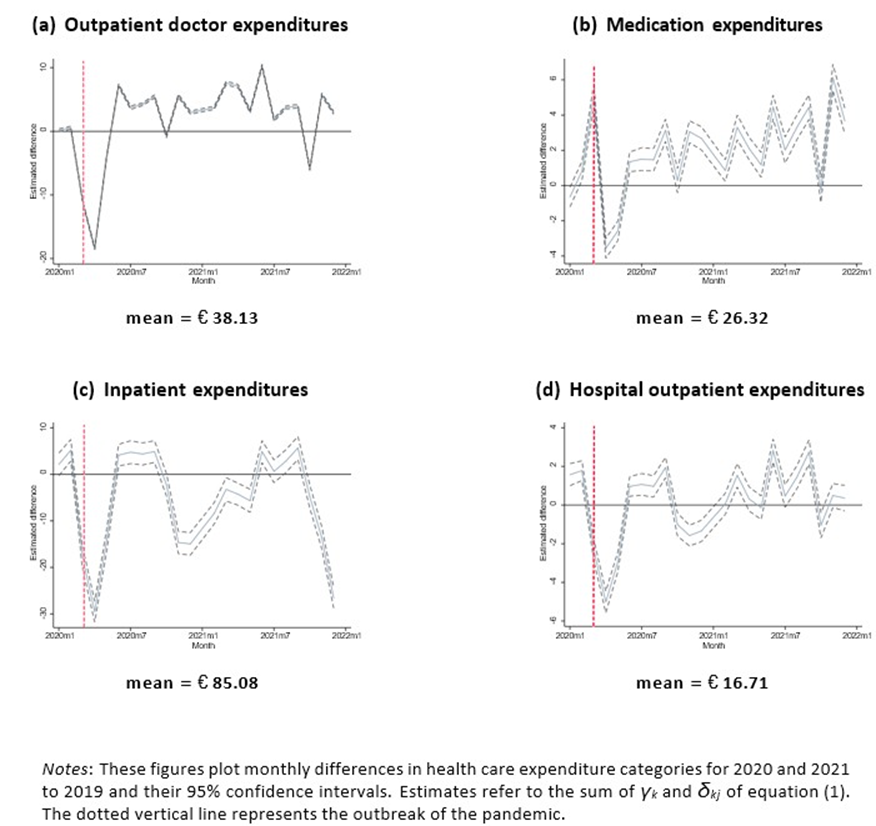
Figure 2: Aggregate healthcare utilization.
Collateral damages
The previous look at trends in health care utilization makes it clear that the outbreak of the pandemic and the measures taken to combat it must have had a massive impact on those who were not infected. The immediate and sometimes recurrent decline in the use of health care services suggests a disruption of routine procedures in the form of cancellations and postponements of necessary diagnostic and therapeutic services. In the following, we analyze the collateral damage of the pandemic and its accompanying measures at (three) different levels: (i) life-threatening conditions, (ii) quantitatively important non- life-threatening health conditions, and (iii) mental health.
Life-threatening conditions
In Austria, too, the most common causes of death are cardiovascular diseases (about 35%) and cancer (about 23%), followed by diseases of the respiratory and digestive organs. The descriptive figures in Table 1 indicate a decrease in the treatment of both cancer and the major cardiovascular diseases during the COVID-19 pandemic.
Figure 3 shows how inpatient spending for cancer and cardiovascular disease have evolved. Expenditures for both categories dropped significantly below 2019 levels during the lockdowns and recovered in the following summer months of 2020 and 2021. Services related to cancer and cardiovascular disease are diverse. In addition to the diagnosis and immediate treatment of the diseases, they include readmissions for monitoring and follow-up examinations. Therefore, we also analyze the first occurrence of malignant neoplasms, stroke and myocardial infarction as an alternative estimate of the short-term collateral damage of a life-threatening disease.
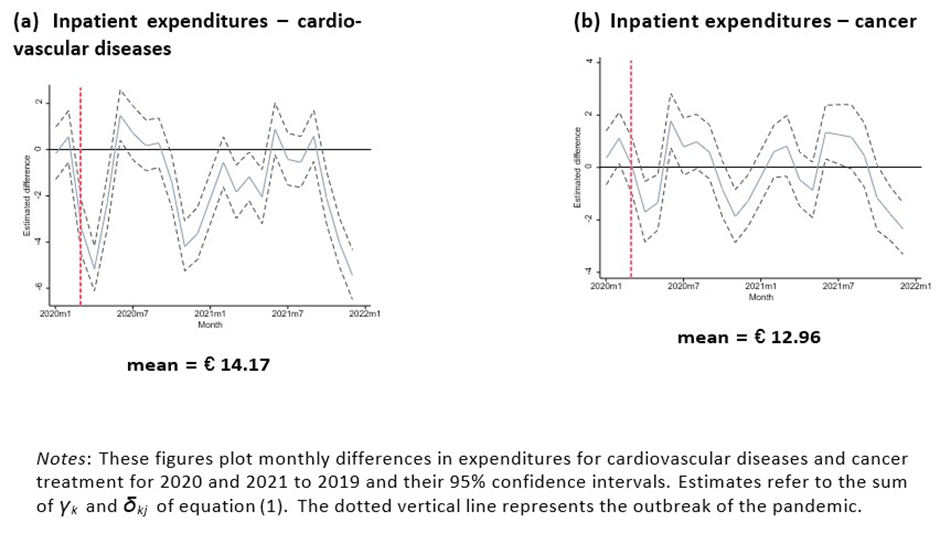
Figure 3: Life-threatening conditions – expenditures.
Panels (a) and (b) of Figure 4 show that the first occurrence of myocardial infarction declined with the onset of the pandemic in March 2020 and in waves three and four by up to more than 30% in individual months, while the decline in the number of stroke cases was quantitatively much smaller. Similarly, panel (c) shows a 30% decrease in new cancer diagnoses after the onset of the pandemic. Although quantitatively smaller, significant declines in diagnoses were also observed with the onset of the second wave in the fall of 2020 and during the fourth COVID wave and associated lockdown at the end of 2021. However, as in the case of cancer treatment expenditures, the decline in diagnoses was partially offset by an increase in the summer months of 2020 and 2021. As can be seen in the descriptive Table 1, the decrease in the number of first-time diagnoses of malignant neoplasms in 2021 was only 1.3% compared to 2019.
Panels (d) and (e) show that the incidence of cancers with the highest 5-year survival rates (testicular, thyroid, prostate, breast, and Hodkin’s disease) and the lowest survival rates (pancreatic, liver, oesophageal, lung, and brain) followed similar trends until September 2021. In contrast, the decline in first-time oncology diagnoses in the fourth quarter of 2021 was driven primarily by cancers with low survival rates.
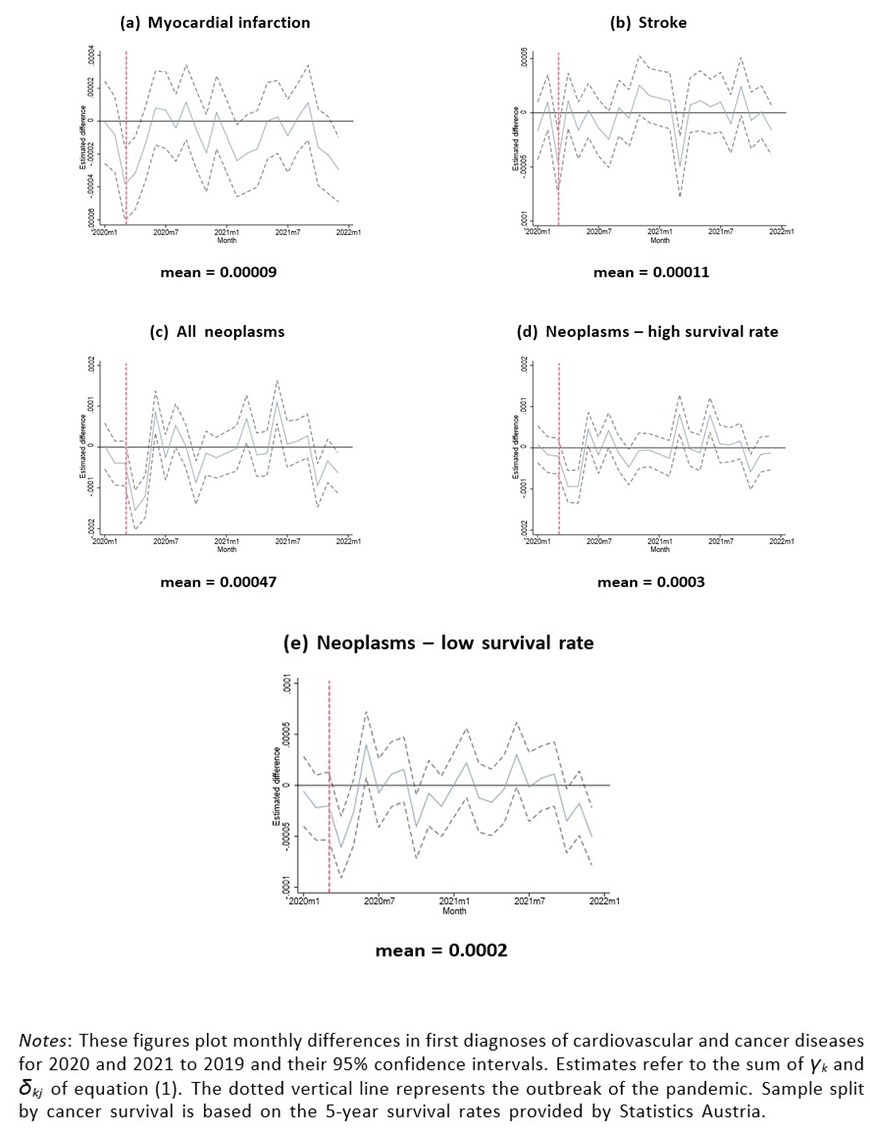
Figure 4: Life-threatening conditions – first diagnoses.
Health screenings
The Austrian health care system offers several preventive health care programs to its insured. The general medical check-up, which is free of charge for adults, aims to identify risk factors for cardiovascular diseases and to change unhealthy lifestyles through medical advice. In addition, specific cancer screening programs provide early detection of malignant oncological diseases. Pandemic-related failures or delays in these screening programs can have a significant impact on the future incidence of these diseases.
As expected, the onset of the pandemic was associated with a significant decline in participation in both general and gender-specific screening (Figure 5). The declines for colposcopy (panel (d)) and psa testing (panel (c)) were about 50%, while participation in general screening and mammography was 75 to 80 %. However, with the exception of colposcopy, significant positive deviations were observed from June 2020, leading to a significant overall increase in participation in 2021. In contrast, participation in colposcopy declined significantly from mid-2021.
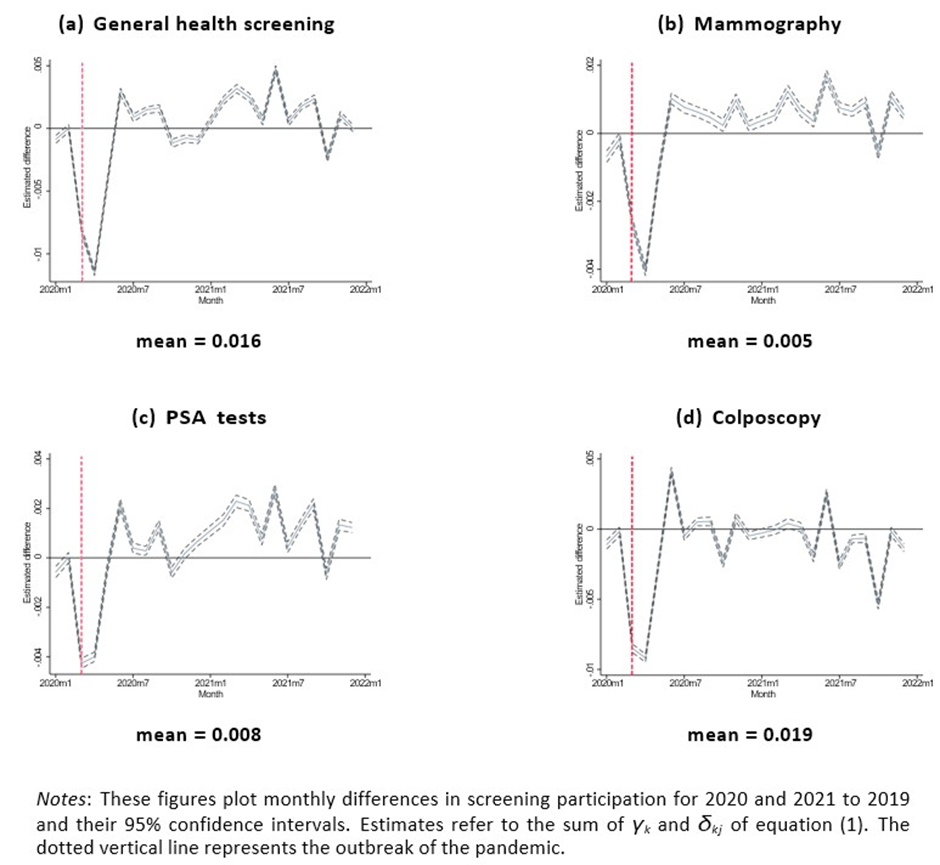
Figure 5: Screening participation.
Elective surgery
Another important area of potential collateral damage that is not directly life-threatening is the failure or postponement of planned medical interventions. Three quantitatively important areas of services that, if not performed or performed too late, worsen people’s quality of life are orthopaedic endoprosthetics, cataract surgery, and varicose vein surgery. Changes in the use of these services are shown in Figure 6.
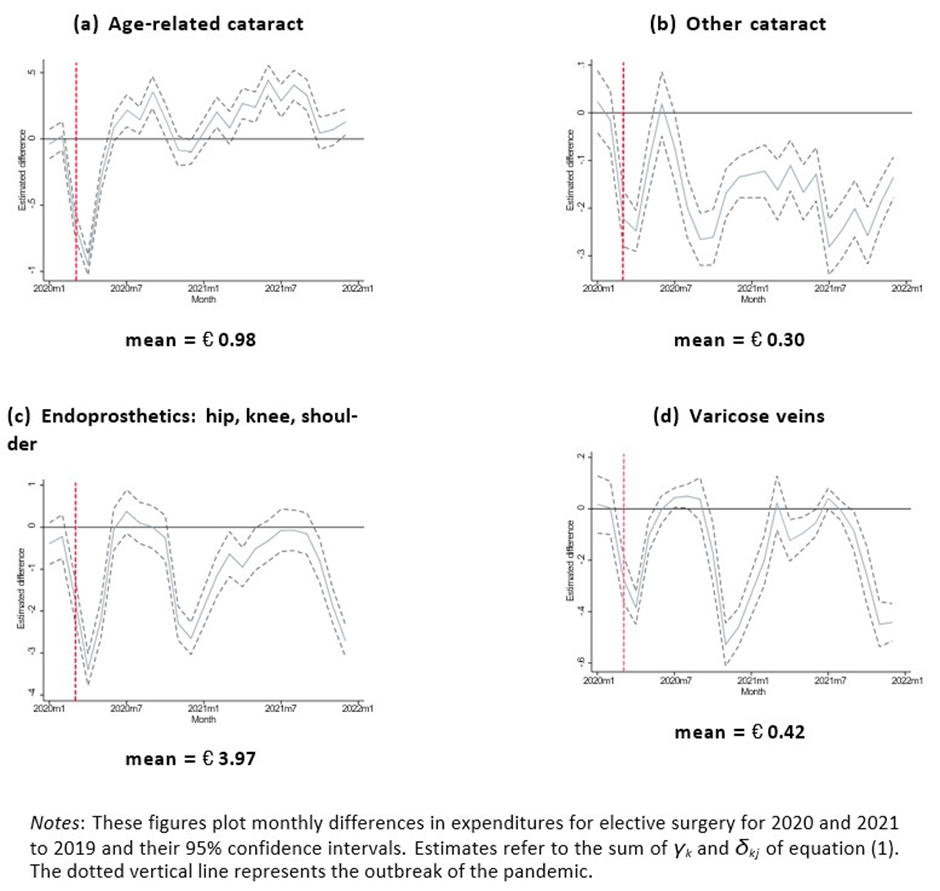
Figure 6: Elective surgery.
The decline in spending on elective surgery with the onset of the pandemic was dramatic, with decreases of up to 100%. With the exception of age-related cataract surgery, scheduled services also declined sharply in the subsequent lockdowns. In 2021, the declines still averaged 60.6% (other cataracts), 40.1% (varicose veins), and 23.3% (endoprosthetics). On the other hand, the decrease in agerelated cataract surgeries since the outbreak of the pandemic could be overcompensated in 2021 (+20.3%).
Mental health
Both academic literature and public discourse have addressed the negative impact of the pandemic and its accompanying measures on people’s mental health. Two different mechanisms appear to be responsible. On the one hand, it can be assumed that, as in many other service areas, medical care for mental illness declined with the outbreak of the pandemic. On the other hand, the pandemic, with all its accompanying symptoms such as lockdowns, home-schooling, reduced social contacts, loss of employment and income, risk of infection, and concern about serious illness, is likely to be associated with considerable psychological distress.
Key findings from our empirical analysis of mental health services are summarized in Figure 7. As can be seen in panels (a) and (b), outpatient spending on mental health care broadly followed the familiar pattern seen in private practice, with a significant decline in services at the onset of the pandemic. However, the subsequent catch-up effects were much smaller than in other medical fields. At 2.5 % (neurology and psychiatry) and 3.7% (psychotherapy and psychology), the average annual increase in services in 2021 was significantly lower than for all physicians in the outpatient sector.
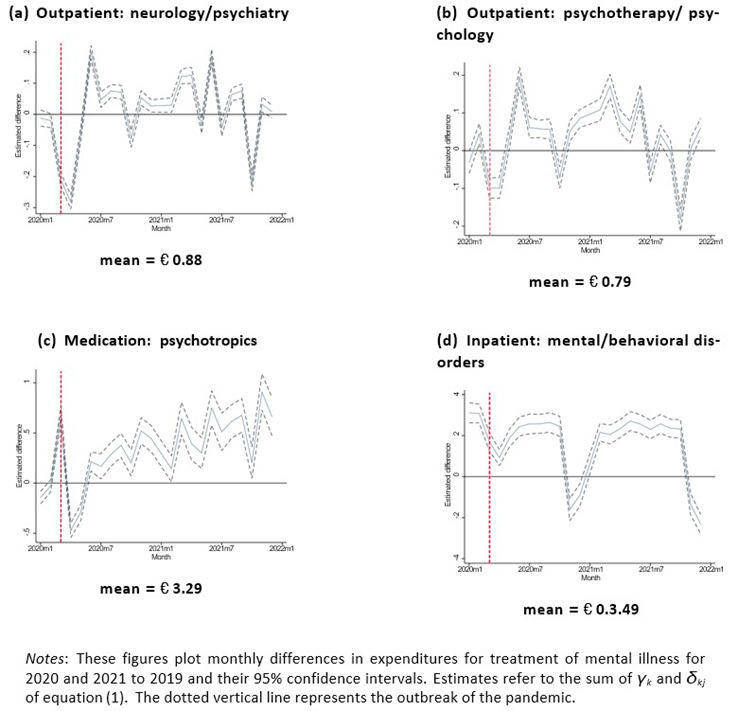
Figure 7: Mental health expenditures.
Panel (c) shows a clear upward trend in the use of psychotropic drugs over time. At the beginning of the pandemic, we first observe the familiar pattern of medication use. The possibility of e-medication led patients to stock up on the necessary drugs immediately after the start of the pandemic. This increase was followed by a decrease in the following months, before a steady increase in the prescription of psychotropic drugs was observed from June 2020 onwards11. For the first and second pandemic years, the overall increase in psychotropic prescriptions was 4.9 and 14.5%, respectively (Table 1). A similarly strong trend in use, indicating an increase in mental disorders and illnesses during the pandemic, was not observed for other groups of drugs.
The trend in expenditure on inpatient treatment of mental and behavioural disorders in panel (d) is difficult to interpret. On the one hand, we observe the familiar decrease in hospital services with the onset of the pandemic and the subsequent lockdown phases. On the other hand, there was already a positive and significant level shift in January and February 2020, making a serious assessment of pandemic-related service utilization difficult.
Discussion and Concluding Remarks
With the outbreak of the COVID-19 pandemic, health care spending in Upper Austria has dropped significantly. In March and April 2020, spending on physician services fell by 32% and 47%, respectively. From June, spending on physician visits stabilized at a higher level than in 2019. The decline in inpatient medical services with the onset of the pandemic was similarly pronounced. Total spending on inpatient care in March and April 2020 fell by 24% and 35%, respectively. Unlike outpatient care, inpatient care continued to decline significantly during the subsequent lockdowns, as hospitals held capacity in reserve in anticipation of the impending waves of infection.
In the immediate aftermath of the pandemic, significantly more drugs were prescribed in March 2020 and significantly less in April and May of that year. Thereafter, there was a steady increase in prescribing patterns above 2019 levels throughout the pandemic. Chronically ill patients stocked up on needed medicines at the onset of the pandemic, and the ability to e-prescribe meant that there was no overall decrease in the supply of medicines to the population.
Spending on inpatient care for cardiovascular disease and cancer fell significantly below 2019 levels during the lockdown periods. This is reflected in a reduction of up to 30% in new diagnoses of myocardial infarction, while the reduction in the number of stroke cases was quantitatively smaller. The decrease in new cancer diagnoses immediately after the start of the pandemic (30%) and in subsequent COVID waves was partially offset by an increase in the summer months of 2020 and 2021. Both the decline in spending on cardiovascular and oncological care and the significantly lower incidence of new diagnoses of cancer and myocardial infarction suggest significant collateral damage in the area of life-threatening diseases. This finding is supported by the fact that the decline in first-time cancer diagnoses was more pronounced for entities with lower survival probabilities.
Combined with lower rates of participation in general and specific health screening in the first year of the pandemic, our short-term results suggest that cancers and heart attacks were diagnosed less frequently or at a later stage, making them more difficult to treat. However, a serious quantitative assessment of the negative impact of the pandemic on medical care for life-threatening diseases would require longer-term data.
We provide clear evidence of non-life-threatening collateral damage caused either by the pandemic outbreak itself or by accompanying policies. The significant postponement of otherwise elective orthopaedic procedures is associated with a deterioration in the quality of life of affected patients. In addition, the age structure of the patient population and limited treatment capacity mean that not all missed surgeries can be made up. The same is true for the decline in cataract and varicose vein procedures. Declines in major elective procedures ranged from 10% to 35% in the first year of the pandemic. With the exception of geriatric cataract procedures, whose decline was offset in the second year of the pandemic, hip, shoulder, knee, and vein procedures experienced similar or greater declines in 2021 than in the previous year. The backlog of elective procedures caused by the pandemic cannot be made up. The shortage of medical and nursing staff will make it impossible to fully utilize Austria’s surgical capacity even after the pandemic ends.
We also find evidence of a deterioration in mental health over the course of the pandemic. Physician outpatient spending on mental health care declined at the onset of the pandemic and later in the subsequent quarantine period. Combined with the finding that physician expenditures stabilized during the (summer) months of low infection rates, this suggests behavioral effects on patients and physicians similar to those seen in other specialties. Access to physicians’ offices was limited or, in some cases, unavailable for several weeks, and patients may not have made appointments for fear of infection.
In contrast to spending on medical care for mental health, there was a significant and sustained increase in the use of psychotropic drugs from June 2020 to the end of the pandemic. The percentage increase for the second pandemic year was 14.5% compared with 2019. This sharp increase in the use of psychotropic drugs suggests a marked deterioration in mental health over the course of the pandemic. The ability to prescribe drugs electronically was the institutional prerequisite for the dynamic development of this group of drugs.
Heterogeneous pandemic effects: The trend in expenditures for physician visits and hospitalizations during the pandemic was almost identical for men and women and for different age groups12. However, we found significant differences in drug use by patient age. Appendix Figure A.1 shows that the increase in drug use from mid-2020 was particularly pronounced in younger cohorts (panels (a) and (b)), while it remained almost unchanged for older patients over 65 years (panel (d)).
The incidence of cardiovascular disease during the pandemic was also similar for men and women, as shown in panels (a)-(d) of Figure A.2. Similarly, panels (e) and (f) of the figure suggest that the trends in initial oncology diagnoses over time were identical for women and men. However, in January 2020 - before the onset of the pandemic - the number of initial cancer diagnoses was lower for women and higher for men than in January 2019. When these non-COVID-related time effects are taken into account, the decrease in first diagnoses is mainly driven by men. This could be interpreted as an indication that women are generally more aware of their health and less likely to postpone or forgo appropriate medical check-ups. The significant decline in elective procedures such as endoprostheses, cataracts and vein surgery affected men and women equally.
The most striking gender and age effects are found in the use of psychotropic drugs. Figure A.3 shows that the increase in the use of mental health drugs was particularly pronounced among males and younger cohorts. Figure A.4 shows a strong and sustained increase in the use of migraine medication, while the time course for antidepressants does not at first sight suggest a significant increase. However, it should be noted that the prescription levels at the beginning of 2020, before the pandemic outbreak, were significantly lower than at the same time in 2019, which makes it difficult to interpret the further course over time. The figure also shows that there are no gender differences for either drug group. The strongest increase in the use of antidepressants can be observed in the age group below 25 years, which can be taken as an indication that the youngest cohorts have suffered most psychologically from the restrictions imposed by the pandemic (Figure A.5). In the case of migraine medications, the percentage increase in use is particularly pronounced in the middle cohorts, in addition to the youngest age group. This may indicate that the psychological burden on parents with school-age children was also particularly high during the pandemic.
This study provides interesting insights into the extent of collateral damage in a Bis- marckian health sector during the COVID-19 pandemic. Although we cannot clearly distinguish between the effects caused by the pandemic itself and those caused by ac- companying policy measures, the empirical evidence shows a clear reduction in the use of services during the pandemic period compared with pre-pandemic levels. This finding is largely in line with the results of a number of comparable international studies cited above. Changes in health care utilization do not allow direct conclusions to be drawn about the health status of individuals. However, the decline in first-time diagnoses of cancer and cardiovascular disease suggests that serious diseases were not detected or were detected late. In addition, the sharp and significant reduction in elective health care ser- vices is likely to have had a negative impact on patients’ quality of life13. Finally, the steady increase in the use of psychotropic drugs over the course of the pandemic is an undeniable indication of a deterioration in the mental health of the population, especially among younger age groups.
A final assessment of the pandemic management in (Upper) Austria is not easy based on the available evidence. On the one hand, inpatient care for COVID-19 patients was very good, even by international standards; on the other hand, this must be set against the lack of care for other diseases. In addition, it is not clear to what extent the shortcomings in care are due to a reduction in medical services or to changes in patient behavior.
The extent to which the short-term decline in the use of medical services for life- threatening diseases leads to a long-term increase in severe diseases can only be answered satisfactorily with data available beyond the pandemic period. The fact that the decline in initial diagnoses of oncological diseases in 2021 compared with pre-pandemic levels is significantly lower than in 2020 suggests that no negative long-term effects are to be expected in this area of care. The stabilization of cancer screening uptake from summer 2020 onwards supports this view.
Several conclusions can be drawn from this work. The negative effects of the lack of coordination between the outpatient and inpatient sectors in Austria were significantly exacerbated during the pandemic. Policy measures in the hospital sector were insufficiently accompanied or mitigated by countermeasures in the outpatient sector. The lack of central control and financing of the health care system is particularly ineffective and inefficient in the exceptional situation of a global and national health crisis. The (negative) experience of the pandemic could be used as a catalyst for a renewed discussion on financing the inpatient and outpatient sectors from a single source.
Catching up on elective hospital services, which declined sharply during the pandemic, is proving difficult due to the acute shortage of health workers. All human resource development measures that have a positive impact on the medical staff should be supported, as well as all options that help to reduce the physical and mental strain on staff.
Finally, the evidence presented here on the deterioration of mental health in the population calls for special attention and appropriate countermeasures. Improved preventive and therapeutic services, especially for young and middle-aged cohorts, appear essential, both in terms of the negative mental health effects that have occurred and in terms of potential future health crises.
Declarations Funding
We gratefully acknowledge financial support from the Austrian
Federal Ministry for Digital and Economic Affairs and the National Foundation for Research, Technology, and Development.
Conflicts of Interest: The authors report no conflicts of interest.
Availability of Data and Materials
There is an online appendix available with additional empirical results. Data used in this study cannot be made available due to data privacy restrictions.
Ethics Approval: Not applicable Author Contributions
Both authors contributed equally to this study conception; empirical analysis (Wolfgang Frimmel); first draft of the manuscript (Gerald J. Pruckner); both authors commented on versions of the manuscript and approved the final manuscript.
References
- Aknin LB, De Neve JE, Dunn EW, Fancourt DE, Goldberg E, et al. (2022) Mental health during the first year of the covid-19 pandemic: A review and recommendations for moving forward. Perspect Psychol Sci 17: 915-936.
- Aksunger N, Vernot C, Littman R, Voors M, Meriggi NF, et al. (2023) Covid-19 and mental health in 8 low- and middle-income countries: A prospective cohort study. PLoS Med 20: 1-22.
- Alsan M, Chandra A, Simon K (2021) The Great Unequalizer: Initial Health Effects of COVID-19 in the United States. Journal of Economic Perspectives 35: 25-46.
- Arsenault C, Gage A, Kim MK, Kapoor NR, Akweongo P, et al. (2022). COVID-19 and resilience of healthcare systems in ten countries. Nat Med 28: 1314-1324.
- Beutel ME, Hettich N, Ernst M, Schmutzer G, Tibubos AN, et al. (2021) Mental health and loneliness in the German general population during the COVID-19 pandemic compared to a representative pre-pandemic assessment. Sci Rep 11: 14946.
- Bhatt AS, Moscone A, McElrath EE, Varshney AS, Claggett BL, et al. (2020) Fewer hospitalizations for acute cardiovascular conditions during the COVID-19 pandemic. J Am Coll Cardiol 76: 280-288.
- Brodeur A, Gray D, Islam A, Bhuiyan S (2021) A literature review of the economics of covid-19. J Econ Surv 35: 1007-1044.
- Cantor J, Sood N, Bravata DM, Pera M, Whaley C (2022) The impact of the covid-19 pandemic and policy response on health care utilization: Evidence from county-level medical claims and cellphone data. J Health Econ 82: 102581.
- Chang WH (2020) The The influences of the COVID-19 pandemic on medical service behaviors. Taiwan J Obstet Gynecol 59: 821-827.
- Czeisler MÉ, Marynak K, Clarke KEN, Salah Z, Shakya I, et al. (2020) Delay or Avoidance of Medical Care Because of COVID-19-Related Concerns - United States, June 2020. MMWR Morb Mortal Wkly Rep 69: 1250-1257.
- Deng J, Zhou F, Hou W, Heybati K, Lohit S, et al. (2023) Prevalence of mental health symptoms in children and adolescents during the COVID-19 pandemic: A meta-analysis. Ann N Y Acad Sci 1520: 53-73.
- Fetzer T, Rauh C (2022) Pandemic Pressures and Public Health Care: Evidence from England. CAGE Working Paper (607).
- Fu R, Sutradhar R, Li Q, Eskander A (2022) Virtual and in-person visits by Ontario physicians in the COVID-19 era. J Telemed Telecare 30: 706-714.
- Godøy A, Grøtting MW (2023) Implementation and spillovers of local non-pharmaceutical interventions. Health Econ 32: 822-852.
- Hatef E, Lans D, Bandeian S, Lasser EC, Goldsack J, Weiner JP (2022) Outcomes of In-Person and Telehealth Ambulatory Encounters During COVID-19 Within a Large Commercially Insured Cohort. JAMA Netw Open 5: e228954.
- Huang F, Liu H (2023) The impact of the COVID-19 pandemic and related policy responses on non-COVID-19 healthcare utilization in China. Health Econ 32: 620-638.
- Lai AG, Pasea L, Banerjee A, Hall G, Denaxas S, Chang WH, et al. (2020) Estimated impact of the COVID-19 pandemic on cancer services and excess 1-year mortality in people with cancer and multimorbidity: near real-time data on cancer care, cancer deaths and a population-based cohort study. BMJ Open 10: e043828.
- Land Oberosterreich AS (2022) Verursachte das Coronavirus in Oberösterreich eine Übersterblichkeit?
- Leong C, Kowalec K, Eltonsy S, Bolton JM, Enns MW, et al. (2022) Psychotropic Medication Use Before and During COVID-19: A Population-Wide Study. Front Pharmacol 13: 886652.
- Mafi J, Craff M, Vangala S, Pu T, Skinner D, et al. (2022) Trends in US Ambulatory Care Patterns During the COVID-19 Pandemic, 20192021. JAMA 327: 237.
- Mira JJ, Lorenzo S (2021) Collateral damage for failing to do in times of COVID-19. J Healthc Qual Res 36: 125-127.
- Moynihan R, Sanders S, Michaleff ZA, Scott AM, Clark J, et al. (2021) Impact of COVID-19 pandemic on utilisation of healthcare services: a systematic review. BMJ Open 11: e045343.
- Mulligan CB, Arnott RD (2022) Non-covid excess deaths, 2020-21: Collateral damage of policy choices? Working Paper 30104, National Bureau of Economic Research.
- Nadarajah R, Wu J, Hurdus B, Asma S, Bhatt DL, et al. (2022) The collateral damage of COVID-19 to cardiovascular services: a metaanalysis. Eur Heart J 43: 3164-3178.
- Oberndorfer M, Dorner TE, Brunnmayr M, Berger K, Dugandzic B, et al. (2022) Health-related and socio-economic burden of the COVID-19 pandemic in Vienna. Health Soc Care Community 30: 1550-1561.
- Pierce M, McManus S, Hope H, Hotopf M, Ford T, et al. (2021) Mental health responses to the COVID-19 pandemic: a latent class trajectory analysis using longitudinal UK data. Lancet Psychiatry 8: 610-619.
- Raina P, Wolfson C, Griffith L, Kirkland S, McMillan J, et al. (2021) A A longitudinal analysis of the impact of the COVID-19 pandemic on the mental health of middle-aged and older adults from the Canadian Longitudinal Study on Aging. Nat Aging 1: 1137-1147.
- Reges O, Feldhamer I, Wolff Sagy Y, Lavie G (2022) Factors Associated with Using Telemedicine in the Primary Care Clinics during the COVID-19 Pandemic in Israel. Int J Environ Res Public Health 19: 13207.
- Roy CM, Bollman EB, Carson LM, Northrop AJ, Jackson EF, et al. (2021) Assessing the indirect effects of COVID-19 on healthcare delivery, utilization and health outcomes: a scoping review. Eur J Public Health 31: 634-640.
- Sud A, Jones M, Broggio J, Loveday C, Torr B, et al. (2020) Collateral damage: the impact on outcomes from cancer surgery of the COVID-19 pandemic. Ann Oncol 31: 1065-1074.
- Thaler M, Khosravi I, Hirschmann M, Kort N, Zagra L, et al. (2020) Disruption of joint arthroplasty services in Europe during the COVID-19 pandemic: an online survey within the European Hip Society (EHS) and the European Knee Associates (EKA). Knee Surg Sports Traumatol Arthrosc 28: 1712-1719.
- Varga TV, Bu F, Dissing AS, Elsenburg LK, Herranz Bustamante JJ, et al. (2021) Loneliness, worries, anxiety, and precautionary behaviours in response to the COVID- 19 pandemic: A longitudinal analysis of 200,000 Western and Northern Europeans. Lancet Reg Health Eur 2: 100020.
- Vindegaard N, Benros ME (2020) Covid-19 pandemic and mental health conse- quences: Systematic review of the current evidence. Brain Behav Immun 89: 531-542.
- Zhang J (2021) Hospital Avoidance and Unintended Deaths during the COVID-19 Pandemic. American Journal of Health Economics 7: 405426.
- Ziedan E, Simon KI, Wing C (2020) Effects of state COVID-19 closure policy on non-COVID-19 health care utilization. National Bureau of Economic Research (w27621).
Endnotes
1For a comprehensive literature review of the economic consequences of the COVID pandemic and government responses, see Brodeur et al. (2021). Godøy and Grøtting (2023) analyze the economic consequences of local non-pharmaceutical interventions to contain the pandemic. They report a shift in local residents’ consumption of goods and services to neighbouring communities.
2For a related discussion of changes in the behavior of medical personnel with the onset of the pandemic, see Chang (2020).
3There was also a significant excess mortality in Upper Austria during the pandemic. For more details, see Section 2.1.
4Evidence from a survey study in Austria (Oberndorfer et al., 2022) confirms that the health and work-related burden of the pandemic fell disproportionately on residents of lower socioeconomic groups. The most striking inequalities were between income groups and for outcomes such as job loss, worsening financial situation and poorer mental health.
5There is extensive medical literature on the collateral damage of the pandemic. For example, in the area of life-threatening diseases, Nadarajah et al. (2022), based on their meta-analysis, provide evidence of substantial cardiovascular damage during the COVID-19 pandemic. Similarly, Bhatt et al. (2020) document a significant decrease in acute cardiovascular hospitalizations and their length of stay for the first phase of the pandemic in the U.S., while based on UK data, Sud et al. (2020) and Lai et al. (2020) find a significant decrease in life years gained due to pandemicrelated delays in oncologic procedures and dramatic reductions in demand for and supply of cancer services, respectively. Other medical evidence of disruption of elective services is reported by, for example, Thaler et al. (2020) for total joint arthroplasty.
6Deng et al. (2023) provide a systematic review and meta-analysis of the impact of the pandemic on adolescent mental health. They include 191 studies with 1.4 million children and adolescents and find a pooled prevalence of depressive symptoms (31%), anxiety symptoms (31%), and sleep disturbances (42%). Age, grade, education, gender, geographic region, and use of electronics are correlated with the prevalence of mental health disorders.
7Other occupational groups, such as civil servants, farmers, and the self-employed, are compulsorily insured with their own social insurance institutions.
8We cannot exploit data from previous periods due to a change in data sources, so values from 2019 onwards would not be perfectly comparable with data before 2018, but in fact the seasonal patterns before 2018 look very similar to 2019 patterns.
9This indicates that reimbursements transferred from the public sector to hospitals were not reduced to the full extent of the reduction in services.
10Note that Figure 2 and all subsequent figures show the sum of γk and δkj of equation (1). This implies that estimates for January are not necessarily zero if the yearly indicator for 2020 is significantly different from zero. This is, however, only the case for very few outcome variables.
11The pattern of psychotropic drug use in the first year of the pandemic is consistent with that documented, for example, in Leong et al. (2022).
12Since older cohorts are more likely to use the health care system, the pandemic-related reduction in services naturally has a greater impact on the elderly. This is particularly true for those services that are predominantly provided to older age groups. Geriatric cataract, endoprosthesis and vein surgery clearly fall into this category.
13However, there is no satisfactory answer to the question of whether the level of care, for example in joint replacement, was adequate before the outbreak.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.