The Challenging Management of an Acinetobacter Baumannii Infection and Recurrent Subcutaneous Abscess in an Elderly Patient Undergoing Surgery for Hip Fracture
by Maria Perrotti1, Filomena Forino1, Pasquale Majorano2, Roberto Formisano2, Giovanni Perrotta2, Carlo Miccio2, Carmine Dello Russo1, Luca Corbia1, Maddalena Conte1, Giuseppe Rengo1,2, Dario Leosco1, Laura Petraglia1,3*, Antimo Papa2
1Department of Translational Medical Sciences, University of Naples “Federico II”, Naples, Italy
2Istituti Clinici Scientifici Maugeri IRCCS-Scientific Institute of Telese Terme, Telese Terme, Benevento, Italy.
3ANASTE Humanitas Foundation, Roma, Italy
*Corresponding author: Laura Petraglia, Department of Translational Medical Sciences, University of Naples “Federico II”, Via Pansini, 5, 80131, Naples, Italy
Received Date: 22 May 2025
Accepted Date: 27 May 2025
Published Date: 29 May 2025
Citation: Perrotti M, Forino F, Majorano P, Formisano R, Perrotta G, et al (2025) The Challenging Management of an Acinetobacter Baumannii Infection and Recurrent Subcutaneous Abscess in an Elderly Patient Undergoing Surgery for Hip Fracture. Ann Case Report. 10: 2299. https://doi.org/10.29011/2574-7754.102299
Abstract
Background: Proximal femoral fractures are the most prevalent disabling traumatic injuries among the elderly, imposing significant human and societal burdens. Surgical fixation, preferably via intramedullary nailing due to its minimally invasive nature, is the standard treatment. However, postoperative complications, such as femoral shaft fractures, remain common and may necessitate reoperation. Early and intensive rehabilitation is crucial to optimize functional recovery and quality of life. While frailty is often considered an absolute contraindication to surgery, this case challenges that paradigm.
Case presentation: We present the case of an 84-year-old woman admitted for a comminuted fracture of the right femur on residual osteosynthesis (gamma nail implanted in 2017 for a prior subtrochanteric fracture). Her medical history included chronic lymphocytic leukemia, permanent atrial fibrillation requiring anticoagulant therapy (Edoxaban 30 mg), chronic heart and renal failure, previous colon cancer, and a stage II sacral ulcer, indicating limited potential for functional recovery. Shortly after admission, the patient underwent revision fixation of the right femoral fracture with the placement of a diaphyseal metal plate and cerclage wire. Postoperatively, she developed acute respiratory failure requiring non-invasive ventilatory support and brief intensive care unit (ICU) monitoring. Chest computed tomography (CT) revealed a left parieto-apico-basal pneumothorax, bilateral mucus plugging of lobar bronchi, complete atelectasis of the left lower lobe, mild hypoexpansion of the left upper lobe, and a thin left sided pleural effusion. Bronchoscopy was performed for airway clearance and identified Acinetobacter baumannii in the bronchoalveolar lavage. Further complications included dehiscence of the surgical wound, with imaging showing a semi-fluid collection and subcutaneous tissue imbibition. Thrombocytopenia (platelet count 59 × 10⁹/L) contributed to a bleeding tendency and prolonged wound healing. Notably, no episodes of delirium occurred throughout the hospitalization. A comprehensive rehabilitation program including joint mobilization, muscle strengthening, progressive weight-bearing, and respiratory physiotherapy was essential for recovery, aiming to prevent cognitive decline and the adverse effects of prolonged bed rest.
Conclusions: As the surgical population ages, comprehensive risk assessment that accounts for comorbidities and functional status is essential to prevent complications and optimize outcomes through targeted, multidisciplinary strategies. Frailty alone should not preclude surgical intervention; instead, a tailored perioperative approach, including comprehensive geriatric assessment, early rehabilitation, and multidisciplinary care, can substantially enhance postoperative outcomes in high- risk elderly patients.
Keywords: Hip Fracture; Comprehensive Geriatric Assessment; Elderly; Acinetobacter Baumannii Infection; Subcutaneous Abscess; Wound Dehiscence.
Introduction
The fractures of femur are a common cause of major functional decline in many elderly people. As the global population ages, the incidence of hip fractures is increasing, with projections indicating that by 2050, approximately 6.3 million individuals worldwide will experience a hip fracture [1]. Often termed "the last fracture of life," hip fractures profoundly impact patients' quality of life, strain social support systems and family members, and entail substantial healthcare costs [2]. Among the various types of hip fractures, subtrochanteric fractures occurring below the lesser trochanter in the upper femoral shaft are relatively uncommon, accounting for approximately 7% to 34% [3,4]. They may be classified as typical, caused by falls, and atypical, associated with prolonged bisphosphonate use. Management usually involves surgical fixation using an intramedullary hip screw (IMHS) [5].
The literature on reoperations in the elderly is limited, and the complexity of these procedures is further heightened by the need for tailored solutions that address the unique physiological and functional challenges of this population. [6]. The effects of orthopedic surgery on health outcomes in elderly patients are unpredictable and may not be immediately evident. In this population, such condition promotes bacterial colonization; specifically, surgical site infections serve as significant predictors of mortality. [7].
In hospitalized patients, a significant nosocomial pathogen has emerged both as a colonizer and an infectious agent: Acinetobacter baumannii, Acinetobacter baumannii is an opportunistic pathogen capable of causing a broad range of infections, including ventilator-associated pneumonia, urinary tract infections, meningitis, bloodstream infections, gastrointestinal disturbances, and various skin and soft tissue infections [8]. Antimicrobial therapy should be reserved exclusively for cases with confirmed infection, characterized by clear signs such as fever, elevated inflammatory markers, and radiological findings [9]. Infections caused by carbapenem-resistant and multidrug-resistant Acinetobacter baumannii are associated with poor clinical outcomes [10].
In elderly patients, the catabolic effects induced by surgical stress are exacerbated by postoperative immobility [11]. Physiotherapy tailored to the specific type of surgery and the individual patient's condition, in accordance with evidence-based medicine plays a crucial role. Patients should be encouraged to engage in gradual mobilization, with careful consideration of the fall risk. The goal of rehabilitation in geriatric medicine must be multidimensional, focusing on enhancing the patient's residual functional capacities [12]. Although the presence of urinary catheters and intravenous cannulas may interfere with mobilization, promoting early physical activity remains crucial for preventing post-hospital syndrome [13].
Facilitating interpersonal contact, particularly through the presence of family members, is essential for promoting cognitive stimulation and providing psychological support and reassurance. When not medically contraindicated, early oral hydration should be initiated, complemented by intravenous fluids as necessary. The introduction of solid food should also be considered early in the recovery process. If required, nutritional intake may be supplemented with high-protein, vitamin-enriched oral supplements to meet daily nutritional needs and prevent malnutrition, as well as the progression of pressure ulcers.
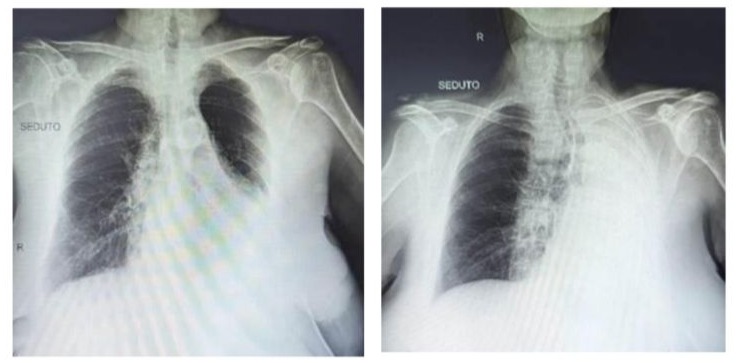
Chest X-Ray: massive pleural effusion occupying the entire left hemithorax.

Subcutaneous drains were placed at the site of the healing wound dehiscence.
Case presentation and discussion
We report the case of an 84-year-old female patient who was admitted to our hospital following a fall that resulted in a comminuted fracture at the site of a previous osteosynthesis of the right femur. The original fixation had been performed in 2017 using an intramedullary gamma nail for a subtrochanteric femoral fracture. The patient's medical history was notable for multiple comorbidities, suggesting a limited potential for functional recovery. These included chronic lymphocytic leukemia, permanent atrial fibrillation requiring anticoagulation therapy with Edoxaban (30 mg daily), chronic heart failure, chronic kidney disease, a history of colorectal cancer, and a stage II sacral pressure ulcer.
Following the surgery, the patient developed severe diaphragmatic dysfunction leading to acute respiratory failure, which required the employment of positive airway pressure ventilation, during a short time of observation in the Intensive Care Unit (ICU) department. After stabilization of her clinical condition, she was transferred to the Internal Medicine department, where she received oxygen supplementation through alternating use of a Venturi mask with FiO2 40% and high-flow nasal cannulas to prevent hypercapnia. Chest computed tomography (CT) revealed a left-sided parieto-apico-basal pneumothorax. Additionally, bilateral mucus plugging was identified, resulting in obstruction of the lobar bronchial branches. There was complete atelectasis of the left lower lobe, accompanied by partial hypo expansion of the left upper lobe. A small pleural effusion was also observed on the left hemithorax.
Given the clinical presentation, a comprehensive pulmonary evaluation was conducted, which led to the decision to perform a bronchoscopy. During the procedure, a large volume of thick, mucoid secretions was aspirated. A bronchoalveolar lavage (BAL) sample was obtained for cytological and non- specific microbiological analysis. The BAL specimen grew Acinetobacter baumannii, prompting the initiation of targeted antibiotic therapy.
In this case, the patient exhibited several risk factors both patient-related and procedure-related for nosocomial pneumonia caused by carbapenem-resistant Acinetobacter baumannii (CRAB), including advanced age, multiple chronic severe conditions (such as chronic lymphocytic leukemia and chronic heart failure), malnutrition, prolonged hospitalization (≥14 days), hypotension, metabolic acidosis, recent surgery, mechanical ventilation, and admission to the ICU [13].
During her stay in the Internal Medicine department, the patient again exhibited signs of respiratory insufficiency. Physical examination revealed absent vesicular breath sounds in the left hemithorax and the presence of moist crackles in the right hemithorax. A chest radiograph was subsequently ordered, revealing a massive pleural effusion occupying the entire left hemithorax. Based on these findings, oxygen therapy was reinitiated, and diuretic therapy was implemented, resulting in symptom improvement and gradual resolution of the effusion. Following the resolution of the infection, as confirmed by the control bronchial aspirate, the patient was transferred to a Highly Specialized Rehabilitation
Hospital. In this setting, the patient underwent a comprehensive pulmonary rehabilitation program tailored to her specific needs, utilizing a device to facilitate airway clearance through bronchial drainage with a specific pneumatic vibratory signal during exhalation. This device liquefies mucus in less than 2 seconds, aiding in its transport from the distal to the central airways [14]. This multidisciplinary approach aimed to enhance respiratory function, improve physical endurance, and facilitate reintegration into daily activities. Given her complex medical history, including chronic lymphocytic leukemia and chronic heart failure with pulmonary hypertension (at the time of admission, echocardiographic exam revealed a pulmonary artery systolic pressure -PAPS- of 55 mmHg and dilated right heart chambers with a D-shaped left ventricle), the rehabilitation team closely monitored her progress to ensure optimal outcomes.
Despite optimal repair of the bone lesion through the application of an external metal plate, the postoperative course was further complicated by delayed wound healing, resulting in surgical wound dehiscence along the lower third of the thigh, accompanied by abundant serohematic discharge. To address this complication, negative pressure wound therapy (NPWT) was initiated. NPWT has been shown to promote wound healing by enhancing granulation tissue formation, reducing edema, and improving local blood flow. Studies have demonstrated that vacuum- assisted closure (VAC) therapy accelerates wound closure, decreases infection rates, and enhances the quality of skin grafts.
However, NPWT has several contraindications. It should not be used in cases of coagulation disorders, active bleeding, or exposure of organs, vessels, and nerves [15]. To minimize the risk of bleeding, some physicians may opt to discontinue anticoagulant therapy in selected patients. This wound treatment system can also lead to complications as failure of the NPWT system (loss of seal, power failure, and blockage of the drainage system), wound infection, pain, bleeding, allergic reactions to the adhesive drape, excoriation of the skin, restricted mobility, tissue adherence to the foam, poor patient compliance, and skin necrosis [16].
During hospitalization, the patient exhibited gradual improvement in respiratory status, with a progressive reduction in oxygen support ultimately achieving eupnoea in ambient air. Inflammatory markers showed a trend toward normalization. However, despite initial improvement with VAC therapy, wound healing was impeded by persistent serohematic exudate and signs of local infection. Cultures obtained from the wound were negative, and imaging studies, including lower limb X-ray and contrast-enhanced CT, ruled out active osteomyelitis [17].
Given the lack of clinical progress and the development of a significant drop in platelet count (PLT 59x103/µL), anticoagulant therapy was discontinued. Advanced wound dressings were applied, the area was carefully cleansed and disinfected with a solution containing chlorhexidine and cetrimide, in accordance with standard aseptic protocols to prevent contamination [18]. The patient continued to receive comprehensive rehabilitation, including joint mobilization and muscular strengthening exercises, progressing from isotonic, isometric, and isokinetic modalities to closed kinetic chain exercises and a gradual reintroduction of load.
The patient adhered to a structured physiotherapy, attending sessions five days a week, with treatment omitted only on days when laboratory tests indicated thrombocytopenia or when hemorrhagic discharge was observed at the site of VAC therapy application. On non-therapy days, the patient exhibited a notable decline in mood, characterized by increased anxiety regarding her health status. She reported symptoms including nausea, loss of appetite, and localized pain in the coccygeal region, which was also the site of a stage II sacral pressure ulcer.
Since the healing of the wound deiscence was encountering many difficulties, with no granulation tissue formation and the occurrence of profuse bleeding, requiring even transfusion therapy, NPWT was discontinued, and a surgical consultation was requested. After excluding the presence of active bleeding and confirming the normalization of the platelet count from a laboratory standpoint (PLT 115 x103/µL). After a comprehensive multidimensional assessment and a collaborative clinical decision-making process between geriatricians and surgeons, an ambulatory approach was chosen with local anesthetic administration to perform a layered suture and place two drains between the subcutaneous layer and the underlying layer, where blood had accumulated. During the following three days the patient reported slight pain in the drainage site, without evidence of flogosis, infection or active bleeding. About 500 cc of fluid (predominantly serum) were drained in the collecting bulbs, and we documented improvement in the swelling of the sutured area and in the pain. The patient subsequently initiated a new cycle of physical therapy focusing on passive
mobilization. Given the sufficient social support (Social Support Scale score: 5/17), the patient was discharged in stable clinical condition. Throughout the hospital stay, the patient was encouraged to adhere to regular repositioning protocols and for a state of chronic hypoalbuminemia was administered intravenous albumin replacement which led to marked improvement of a stage II pressure ulcer. Adequate serum albumin levels are considered a key factor in supporting tissue repair, maintaining oncotic pressure, and enhancing the overall wound healing process [19]. Despite experiencing nausea, likely a side effect of the antibiotic therapy, the patient maintained adequate nutritional intake with the support of family caregivers and the administration of high-calorie, palatable protein supplements.
Conclusions
In the context of preoperative evaluation in older adults, it is crucial to adopt a comprehensive geriatric approach that considers intrinsic capacity and functional status. Examining key domains such as cognition, mobility, nutritional status, sensory function, mood, and social support provides a holistic understanding of the patient’s overall health. This multidimensional perspective enables the healthcare team to identify vulnerabilities that may not be evident in standard preoperative evaluations, supporting individualized risk stratification, optimization of perioperative care, and potentially improved surgical outcomes and recovery trajectories.
References
- Kalan Farmanfarma K, Yarmohammadi S, Fakharian E, Gobbens RJ, Mahdian M, et al (2024) Prognostic Factors of Hip Fracture in Elderly: A Systematic Review. Int J Prev Med. 15:42.
- Veronese N, Maggi S. (2018) Epidemiology and social costs of hip fracture. Injury. 49:1458–60.
- Zuckerman JD. (1996) Hip fracture. N Engl J Med 334:1519–25.
- Napoli N, Schwartz AV, Palermo L, Jin JJ, Wustrack R, et al. (2013) Risk factors for subtrochanteric and diaphyseal fractures: the study of osteoporotic fractures. J Clin Endocrinol Metab 98:659–67.
- Mears SC (2014) Classification and surgical approaches to hip fractures for nonsurgeons. Clin Geriatr Med 30: 229–241.
- Valverde JA, Alonso MG, Porro JG, Rueda D, Larrauri PM, et al (1998) Use of the Gamma nail in the treatment of fractures of the proximal femur. Clin Orthop Relat Res. 1998:56-61.
- Lee J, Singletary R, Schmader K, Anderson DJ, Bolognesi M, et al (2006) Surgical Site Infection in the Elderly Following Orthopaedic Surgery: Risk Factors and Outcomes. The Journal of Bone & Joint Surgery 88:1705- 1712.
- Nishimizu S, Shiota S, Oshiumi T, Takakura T, Miyazaki E. (2021) A case of community-onset Acinetobacter pneumonia in a healthy person. IDCases. 24:e01133.
- Bartal C, Rolston KVI, Nesher L. (2022) Carbapenem-resistant Acinetobacter baumannii: Colonization, Infection and Current Treatment Options. Infect Dis Ther. 11:683-694.
- Sunenshine RH, Wright MO, Maragakis LL, Harris AD, Song X, et al (2007) Multidrug-resistant Acinetobacter infection mortality rate and length of hospitalization. Emerg Infect Dis. 13:97-103.
- Finnerty CC, Mabvuure NT, Ali A, Kozar RA, Herndon DN. (2013) The surgically induced stress response. JPEN J Parenter Enteral Nutr. 37:21S-9S.
- Esquiroz Lizaur I, Zambom-Ferraresi F, Zambom-Ferraresi F, Ollo-Martínez I, De la Casa-Marín A, et al (2024) Postoperative physical rehabilitation in the elderly patient after emergency surgery. Influence on functional, cognitive and quality of live recovery: study protocol for a randomized clinical trial. Trials. 25:584.
- Liu K, Tronstad O, Flaws D, Churchill L, Jones AYM, et al (2024) From bedside to recovery: exercise therapy for prevention of post-intensive care syndrome. J Intensive Care. 12:11.
- Zeng Y, Wu Q, Chen Y, Cai S. (2024) Early comprehensive pulmonary rehabilitation for hospitalized patients with acute ex-acerbation of chronic obstructive pulmonary disease: a randomized controlled trial. J Rehabil Med. 56: jrm39953.
- Landi, G, Mottola, L, Braile, A, Pezzella, R, De Cicco, A, et al (2022) The application of negative pressure wound therapy in orthopedics: current concepts. Lo Scalpello - Journal. 36: 116-121.
- Agarwal P, Kukrele R, Sharma D. (2019) Vacuum assisted closure (VAC)/negative pressure wound therapy (NPWT) for difficult wounds: A review. J Clin Orthop Trauma. 10:845-848.
- Lee YJ, Sadigh S, Mankad K, Kapse N, Rajeswaran G. (2016) The imaging of osteomyelitis. Quant Imaging Med Surg. 6:184-98.
- Olutoye OO, Eriksson E, Menchaca AD, Kirsner RS, Tanaka R, et al (2024) Management of Acute Wounds-Expert Panel Consensus Statement. Adv Wound Care (New Rochelle). 13:553-583.
- Gillespie BM, Chaboyer WP, McInnes E, Kent B, Whitty JA, et al (2014) Repositioning for pressure ulcer prevention in adults. Cochrane Database Syst Rev. 2014:CD009958.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.