The Association Between Breastfeeding and Maternal Mortality
by Kelly Robinson1*, Kimberly D Gregory2, Ozlem Equils1
1MiOra Public Health and Research, USA
2Department of Obstetrics and Gynecology, Maternal Fetal Medicine, Cedars-Sinai Medical Center, USA
*Corresponding author: Kelly Robinson, MiOra Public Health and Research, USA
Received Date: 21 August, 2025
Accepted Date: 30 August, 2025
Published Date: 03 September, 2025
Citation: Robinson K, Gregory KD, Equils O (2025) The Association Between Breastfeeding and Maternal Mortality. J Community Med Public Health 9: 531. https://doi.org/10.29011/2577-2228.100531
Abstract
Breastfeeding is widely recognized for its benefits to infants and its long-term positive impact on maternal health; however, its influence on maternal morbidity in the early postpartum period has been less thoroughly investigated. In this pilot study, we explored the relationship between breastfeeding and maternal mortality using publicly available state-level data from the CDC. Our analysis revealed that states with lower breastfeeding rates tended to have higher maternal mortality rates, whereas states with higher breastfeeding rates showed lower maternal mortality. These findings suggest that breastfeeding may offer protective effects on maternal health in the immediate postpartum period. Proactive training, effective breastfeeding support, and access to lactation consultants may have a significant impact on both maternal and infant health. Further research is needed.
Keywords: Maternal mortality; Morbidity; Breast feeding; Lactation; Mental health; Bleeding; Post-partum recovery; Stigma; Health education; Social support networks; Lactation support; Day-care
Introduction
Breastfeeding has long been promoted for its benefits to infant health [1]; however, growing evidence suggests that it also confers significant health advantages for mothers, including a reduced risk of breast and ovarian cancers—particularly with longer durations of breastfeeding [2]. Additionally, successful breastfeeding has been associated with improved maternal mental health [3]. We hypothesized that successful breastfeeding, defined as sustained breastfeeding initiation and continuation, may be associated with a lower rate of maternal mortality.
Methods
In this pilot study, we utilized publicly available, state-level breastfeeding data from the National Immunization Survey–Child (NIS-Child), conducted by the Centers for Disease Control and Prevention (CDC) and the U.S. Department of Health and Human Services, for infants born in 2019 [4] and 2021 [5]. Breastfeeding indicators included the percentage of infants who were: ever breastfed; exclusively breastfed through 3 and 6 months; and any breastfeeding at 6 and 12 months. These percentages were calculated among all infants surveyed. Exclusive breastfeeding was defined as receiving only breast milk—no solids, water, or other liquids. The proportion of infants who received formula within the first two days of life was calculated among those who initiated breastfeeding. Data from U.S. territories were excluded to align with the analytic approach used for Healthy People 2030 breastfeeding benchmarks [4]. The 2021 data were collected as part of the NIS-Child survey, which samples U.S. households with children aged 19–35 months [5].
Maternal mortality data were obtained from the CDC’s National Center for Health Statistics, covering state-level maternal deaths and mortality rates from 39 states from 2018 to 2022 [6]. Rates were reported per 100,000 live births and tabulated by maternal residence. Maternal deaths were defined as the death of a woman while pregnant or within 42 days of the termination of pregnancy, regardless of the duration or site of pregnancy, from any cause related to or aggravated by the pregnancy or its management, but not from accidental or incidental causes. We examined the relationship between breastfeeding rates and maternal mortality rate by calculating the Pearson correlation coefficient.
Results
Between 2018 and 2022, there were a total of 18,484,949 live births in the United States. During this period, the overall maternal mortality rate was 23.2 per 100,000 live births (95% CI: 22.5– 23.9).
Most infants born in 2019 and 2021 were breastfed at some point, with initiation rates of 83.2% and 84.1%, respectively. In 2019, 19.2% of infants received formula before two days of age; comparable data for 2021 were not available. Exclusive breastfeeding rates declined over time in both cohorts: at three months, 45.3% (2019) and 46.5% (2021) of infants were exclusively breastfed, dropping to 24.9% and 27.2% at six months, respectively. Approximately half of the infants were breastfed “any” at six months (55.8% in 2019 and 59.8% in 2021); however, by 12 months, breastfeeding rates declined to 35.9% (2019) and 27.2% (2021).
A moderate and strong inverse correlation was observed between the percentage of infants ever breastfed and the maternal mortality rate in both 2019 (r = –0.569) and 2021 (r = –0.678) (Table 1). Similarly, there were strong and moderate inverse relationships between maternal mortality and the rate of exclusive breastfeeding through three months (r = –0.641 in 2019; r = –0.513 in 2021), and through six months (r = –0.622 in 2019; r = –0.438 in 2021) (Table 1). Breastfeeding at six months was also strongly inversely correlated with maternal mortality (r = –0.631 in 2019; r = –0.689 in 2021), as was breastfeeding at 12 months (r = –0.619 in 2019; r = –0.634 in 2021) (Table 1, Figure 1). There was no correlation between maternal mortality and formula feeding within the first two days of life in 2019 (r = 0.083) (Table 1, Figure 2).
|
Pearson correlation coefficient (r) |
2019 |
2021 |
|
Formula before 2 days of age |
0.083 |
N/A |
|
Exclusive Breast Feeding at 3 months |
-0.641 |
-0.513 |
|
Exclusive Breast Feeding at 6 months |
-0.622 |
-0.438 |
|
Breast feeding at 6 months |
-0.631 |
-0.689 |
|
Breast Feeding at 12 months |
-0.634 |
-0.634 |
|
Ever breastfed |
-0.569 |
-0.678 |
Table 1: Pearson correlation coefficient between breastfeeding rates and maternal mortality rate in 2019 and in 2021.
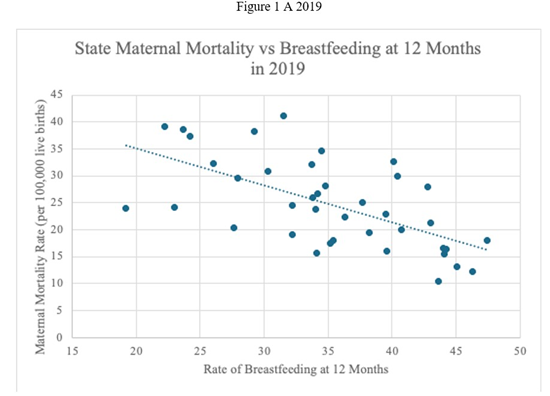
Figure 1A and 1B: Maternal mortality rate and breast feeding at 12 months in 2019 and in 2021.
States with the highest breastfeeding rates at six months and available maternal mortality data in 2019—Minnesota, Washington, Maryland, and Colorado—had lower maternal mortality rates. In contrast, states with the lowest breastfeeding rates at six months—West Virginia, Mississippi, Alabama, Florida, and Louisiana—had the highest maternal mortality rates in that year (Figure 2A). A similar pattern was observed in 2021, where states with high six-month breastfeeding rates, including Washington, Oregon, Colorado, and Maryland, had lower maternal mortality rates, while those with the lowest six-month breastfeeding rates— Nevada, Louisiana, Oklahoma, Mississippi, and West Virginia— had the highest maternal mortality rates (Figure 2B). The states with no published maternal mortality rate for 2018-2022 and were excluded from the study are Alaska, Delaware, District of Columbia, Hawaii, Maine, Montana, New Hampshire, North Dakota, Rhode Island, South Dakota, Vermont and Wyoming.
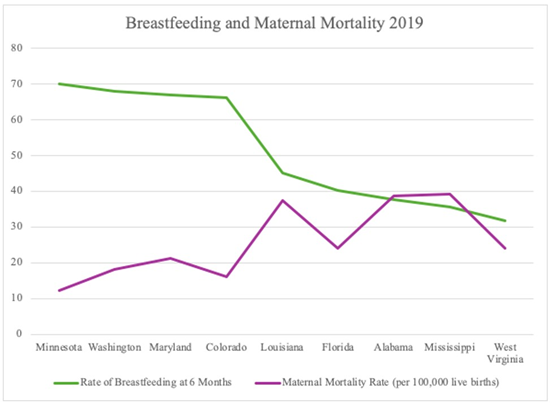
Figure 2A: Maternal mortality rate in states with highest and lowest breast-feeding rates in 2019.
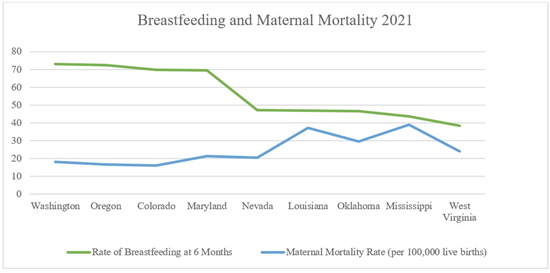
Figure 2B: Maternal mortality rate in states with highest and lowest breast-feeding rates in 2021.
Discussion
In this pilot study, we found that higher breastfeeding rates were associated with lower maternal mortality rates at the state level. Physiologically, breastfeeding induces the release of oxytocin, which promotes uterine involution and reduces the risk of postpartum hemorrhage—one of the leading preventable causes of maternal morbidity and mortality in 2019 [7]. In 2021, COVID-19 was a contributing factor to maternal mortality. Breastfeeding is unlikely to affect COVID-19 related maternal mortality; however, careful data analysis is necessary to fully understand these associations. In addition, breastfeeding has been associated with a reduced risk of type 2 diabetes [8], hypertension [9], cardiovascular disease [10], and improved mental health, particularly when mothers are able to meet their breastfeeding goals [10,11].
While breastfeeding rates in the United States have increased over time, disparities persist. Black mothers have significantly lower breastfeeding initiation rates compared to other racial and ethnic groups (73.6% for Black mothers vs. 90.3% for Asian mothers) [12]. In some states, such as North Dakota, the gap is particularly wide, with breastfeeding rates among Black mothers falling 37.6 percentage points below those of other groups [12]. Notably, maternal mortality is highest among Black mothers [13], where some of the leading causes of death include mental health conditions and haemorrhage—conditions that may be impacted by breastfeeding practices [13]. Mothers who breast feed may seek and get more attention and social support which may help identify early warning signs associated with late maternal mortality.
The American Academy of Pediatrics (AAP) recommends exclusive breastfeeding for about the first six months, with continued breastfeeding alongside the introduction of complementary foods for at least one year, and up to two years or longer if desired [14]. While many women are aware of the health benefits of breastfeeding, numerous barriers—such as workplace constraints, lack of social or partner support, and logistical challenges—make sustained breastfeeding difficult [15]. Approximately half of U.S. infants receive non-parental care, yet many childcare providers are hesitant to handle expressed breast milk [16], further compounding these challenges.
This study has several limitations. It is a retrospective, ecological analysis using state-level data, which limits causal inference and granularity. State demographics may contribute to these results. The dataset does not include individual-level demographic, socioeconomic, or clinical information, and breastfeeding metrics were self-reported. Larger, prospective studies are needed to further explore the relationship between breastfeeding and maternal health outcomes.
Conclusion
This pilot study suggests an inverse association between statelevel breastfeeding rates and maternal mortality, supporting the hypothesis that breastfeeding may serve as a protective factor against maternal mortality. These findings highlight the need for postpartum breastfeeding support, especially among populations at higher risk for adverse outcomes. Health professionals—including lactation consultants, nurses, doulas, midwives, paediatricians, and WIC counsellors—can serve as breastfeeding advocates. To fully realize the maternal health benefits of breastfeeding, efforts should prioritize culturally sensitive support, standardized definitions, and equity-centered public health policies.
Acknowledgements
The authors received no financial support for the publication of this manuscript.
Ethical Guidelines
This study uses publicly available data and does not involve human or animal subjects, therefore we did not seek ethical approval.
Conflict of Interest
The authors declare they have no conflict of interest.
References
- Victora CG, Bahl R, Barros AJD, França GVA, Horton S, et al. (2016) Breastfeeding in the 21st century: epidemiology, mechanisms, and Lifelong Effect. Lancet 387: 475-490.
- Chowdhury R, Sinha B, Sankar MJ, Taneja S, Bhandari N, et al. (2015) Breastfeeding and maternal health outcomes: A systematic review and meta-analysis. Acta Paediatr 104: 96-113.
- Brown CC, Adams CE, George KE, Moore JE (2021) Mental Health Conditions Increase Severe Maternal Morbidity By 50 Percent and Cost $102 Million Yearly In The United States. Health Aff (Millwood) 40: 1575-1584.
- CDC (2024) Breastfeeding Report Card. Breastfeeding Data.
- CDC. Rates of Breastfeeding by State: 2021. Breastfeeding Data.
- Maternal deaths and mortality rates: Each state, the District of Columbia, United States, 2018-2022. CDC.
- Association of Women’s Health, Obstetric and Neonatal Nurses (2021) Guidelines for Active Management of the Third Stage of Labor using Oxytocin: AWHONN Practice Brief Number 12. J Obstet Gynecol Neonatal Nurs 50: 499-502.
- Tarrant M, Chooniedass R, Fan HSL, Del Buono K, Masina S (2020) Breastfeeding and Postpartum Glucose Regulation Among Women With Prior Gestational Diabetes: A Systematic Review. J Hum Lact 36: 723-738.
- Bonifacino E, Schwartz EB, Jun H, Wessel CB, Corbelli JA (2018) Effect of Lactation on Maternal Hypertension: A Systematic Review. Breastfeed Med 13: 578-588.
- Perrine CG, Nelson JM, Corbelli J, Scanlon KS (2016) Lactation and Maternal Cardio-Metabolic Health. Annu Rev Nutr 36: 627-645.
- Wheeler A, Sweeting F, Mayers A, Brown A, Farrington S (2025) The Positive Cycle of Breastfeeding—Mental Health Outcomes of Breastfeeding Mothers Following Birth Trauma. Healthcare 13: 672.
- Chiang KV, Li R, Anstey EH, Perrine CG (2021) Racial and Ethnic Disparities in Breastfeeding Initiation - United States, 2019. MMWR Morb Mortal Wkly Rep 70: 769-774.
- Hoyert DL (2024) Health E-stat: Maternal mortality rates in the United States, 2022. Centers For Disease Control and Prevention.
- Meek JY, Noble L (2022) Policy statement: Breastfeeding and the use of human milk. Pediatrics 150: e2022057988.
- Office of the Surgeon General (US), Centers for Disease Control and Prevention (US), Office on Women’s Health (US). Barriers to Breastfeeding in the United States. Nih.gov. Published 2011.
- Schafer EJ, Livingston TA, Roig-Romero RM, Wachira M, LouisJacques AF, et al. (2021) “Breast Is Best, But…” According to Childcare Administrators, Not Best for the Childcare Environment. Breastfeed Med 16: 21-28.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.