Technical Feasibility of Revision and Elongation of Minimally Invasive Transforaminal Lumbar Interbody Fusion (MISS TLIF) for Adjacent Segment Disease: Case Report
by Iago Tsertsvadze1*, Giga Sulaberidze2
1Head of Neurosurgical Department at West Georgia Medical Center, Kutaisi, Georgia
2Neurosurgeon at West Georgia Medical Center, Kutaisi
*Corresponding author: Iago Tsertsvadze, Head of Neurosurgical Department at West Georgia Medical Center, Kutaisi, Georgia
Received Date: 30 October 2025
Accepted Date: 06 November 2025
Published Date: 08 November 2025
Citation: Tsertsvadze I, Sulaberidze G (2025) Technical Feasibility of Revision and Elongation of Minimally Invasive Transforaminal Lumbar Interbody Fusion (MISS TLIF) for Adjacent Segment Disease: Case Report. J Surg 10: 11482 https://doi.org/10.29011/2575-9760.011482
Abstract
Background: Minimally invasive transforaminal lumbar interbody fusion (MISS TLIF) has transformed lumbar spine surgery by achieving clinical and radiological outcomes comparable to conventional open TLIF while significantly reducing soft-tissue trauma, perioperative blood loss, and hospitalization time. Nevertheless, revision or elongation of prior minimally invasive fusions in patients presenting with Adjacent Segment Disease (ASD) is still perceived as technically demanding, especially in resource-limited healthcare environments.
Case Presentation: A 71-year-old male with a history of lumbar spinal stenosis and a low-grade (Meyerding Grade I) L4-L5 spondylolisthesis underwent minimally invasive transforaminal lumbar interbody fusion (MISS TLIF) due to severe low back pain radiating to both legs, more pronounced on the left side, in 2022. Before surgery, his pain was rated 8 on the Visual Analogue Scale (VAS), and his Oswestry Disability Index (ODI) was 82%. After the procedure, his symptoms improved dramatically, with VAS decreasing to 2-3 and ODI to 8%, and radiographic evaluation showed successful fusion graded as Bridwell Grade II. Two years later, he experienced a recurrence of bilateral leg pain and low back pain, which was especially aggravated when standing upright. Imaging revealed adjacent segment degeneration involving L2-L3 and L3-L4, characterized by Meyerding Grade I spondylolistheses and bilateral foraminal stenosis. A revision MISS TLIF was subsequently performed, successfully extending the previous construct up to L2, L2-L3 and L3-L4 discectomy and interbody cage placement. The surgery proceeded without complications. The patient was discharged on the 4th postoperative day and experienced rapid recovery, with VAS score reduced to 2 and significant functional improvement.
Conclusion: Revision and elongation of a previous MISS TLIF construct can be safely and effectively performed with appropriate surgical expertise, preserving the advantages of minimally invasive technique. This case demonstrates that, with meticulous planning and adequate surgical expertise, minimally invasive revision fusion remains feasible, with favorable outcomes and no increase in complication rates.
Keywords: Adjacent Segment Disease; Case Report; Minimally Invasive TLIF; Revision Spinal Fusion; Spondylolisthesis
Introduction
Lumbar fusion with instrumentation remains the standard surgical treatment for degenerative lumbar spinal disorders, including spinal stenosis, spondylolisthesis, and recurrent disc herniation. It provides neural decompression, sagittal alignment restoration, and spinal stabilization in patients unresponsive to conservative therapy. Several interbody fusion strategies are available, including Transforaminal (TLIF), Posterior Lumbar Interbody Fusion (PLIF), minimally invasive TLIF (MIS-TLIF), Oblique Lumbar Interbody Fusion (OLIF), and Anterior or Lateral Approaches (ALIF, LLIF, OLLIF, XLIF) [1-3]. Each technique offers distinct advantages, but there is no universal consensus regarding superiority, and surgical selection should be individualized. The conventional open TLIF, first described by Harms and Rollinger in 1982 [4], is widely adopted. However, extensive muscle dissection may lead to paravertebral muscle atrophy, increased postoperative pain, and delayed functional recovery [5,6]. Open TLIF may also be less effective in correcting coronal imbalance or restoring lumbar lordosis [7]. MIS-TLIF, introduced by Foley in 2003 [8], utilizes tubular retraction and percutaneous screw fixation, minimizing muscular trauma and reducing blood loss [6,9]. Concerns persist regarding limited visualization, adequacy of decompression, correction of coronal imbalance, elevated radiation exposure, and the steep learning curve [10-12]. Alamin et al. reported in a multicenter randomized study that MIS-TLIF significantly reduces paraspinal muscle injury compared with open TLIF as assessed by MRI [13-18].
These considerations motivated the present comparative study. Despite its advantages, Adjacent Segment Disease (ASD) remains a well-recognized long-term complication following spinal fusion, resulting from increased biomechanical stress and motion transfer to levels adjacent to a fused segment [19]. The reported incidence of radiographic ASD varies from 5.2 to 22.7%, depending on the duration of follow-up and surgical technique [20,21]. When ASD becomes symptomatic, revision surgery with extension of the fusion construct is indicated. However, performing revision or elongation MISS TLIF in previously fused patients is technically challenging.
Factors such as limited access, existing instrumentation, and altered anatomy increase the difficulty of exposure and instrumentation. Furthermore, scar tissue formation and disrupted tissue planes increase the risk of dural tears and neurological injury [20-22]. This report describes the management of a 71-year-old man who developed adjacent segment disease two years after a successful single-level L4-L5 MISS TLIF and subsequently underwent revision and elongation of the fusion construct to L2 level and L2-L3 and L3-L4 discectomy and interbody cage placement a minimally invasive approach. The case highlights the technical feasibility, safety, and clinical effectiveness of MISS TLIF revision.
Case Presentation
A 71-year-old man presented with a progressive chronic low back pain radiating to the left buttock, lateral thigh, leg, and leg in 2022. The pain was described as dull and aching in the lumbar region, with sharp radicular exacerbations, especially on the left side. Symptoms were aggravated by standing and lumbar extension and relieved by sitting or forward flexion. The patient reported numbness and tingling along the same distribution, causing difficulty in walking. Walking distance was progressively limited due to pain and heaviness in both lower limbs, improving with rest or forward bending, suggestive of neurogenic claudication. On examination, lumbar lordosis was reduced, with tenderness and at the L4-L5 level, and paraspinal muscle spasm. Lumbar motion was restricted, with painful arc and instability on extension. Straight leg raising was positive on the left at 40°, right at 45°. Neurological assessment revealed pain an paresthesia is both L5 myotomes (mostly in left), preserved deep tendon reflexes. His pre-operative Visual Analogue Scale (VAS) score was 8, and the Oswestry Disability Index (ODI) was 82 %. Pre-operative Magnetic Resonance Imaging (MRI) and CT Scans showed a lowgrade (Meyerding I) L4 spondylolisthesis with a mediolateral, predominantly left-sided L4-L5 disc herniation causing foraminal and central stenosis (Figure 1). L4-L5 Minimally Invasive Spine Surgery (MISS) Transforaminal Lumbar Interbody Fusion (TLIF) with modular percutaneous screws was performed at our institution, including L4 discectomy and the insertion of a PEEK cage filled with bone graft, Post-operatively his condition improved dramatically: at the moment of discharge at 3rd postoperative day his VAS was 2-3 and ODI 8 % at six-month follow-up, with Bridwell fusion grade II.

Figure 1: Shows spondylolisthesis and an L4 mediolateral disc herniation causing bilateral, mostly left sided foraminal stenosis.
Two years after the initial decompression and stabilization at the L4-L5 level, the patient presented with renewed low back pain of insidious onset, gradually increasing over several months. The pain was described as deep and aching, localized higher in the lumbar region than before, with occasional radiation to the anterior thigh, but without distal leg symptoms. The patient reported stiffness and fatigue in the lower back, aggravated by prolonged standing or walking, and relieved by rest or sitting. No bowel or bladder symptoms were noted. On examination, lumbar movements were globally restricted, particularly extension, which reproduced pain in the upper lumbar region. Palpation elicited tenderness over the L2-L3 interspinous space, with paraspinal tightness. No step-off deformity was palpable at the previous operative site. Neurological examination showed mild weakness in hip flexion and reduced sensation over the anterior thigh (L3 dermatome), with preserved knee and ankle reflexes. Pain distribution corresponded to L3-L4 dermatomes. At this admission his VAS was 8 and ODI 80 %. The patient’s pain remained refractory to conservative management, including epidural steroid injection. MRI and CT scans revealed adjacent segment degeneration with Meyerding I listhesis at L3-L4, right-sided L3 disc herniation, mediolateral L2 disc herniation, and bilateral foraminal stenosis. The previously fused L4-L5 level remained stable, with no hardware complications (Figure 2). Revision Minimally Invasive (MIS) TLIF was therefore performed, involving the elongation of the previous instrumentation to L3 and L2, included L2 and L3 discectomies with insertion of PEEK cages filled with bone graft.
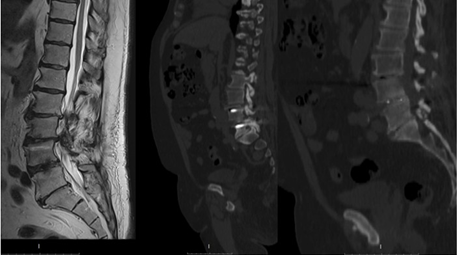
Figure 2: Showing Grade I spondylolisthesis at the L3-L4 level with severe spinal canal stenosis at the L2-L3 and L3-L4 levels, and radiological signs of fusion at the L4-L5 disc space.
Surgical Technique
The operative level was identified intraoperatively using C-arm fluoroscopy, and the pedicle midpoints were marked. A 1-2 cm incision was made approximately 1 cm lateral to the L2 and L3 pedicle projections. A Jamshidi needle was advanced into the medial pedicle cortex, and guidewires were placed bilaterally. Serial tubular dilators were advanced, and a 22-mm diameter tubular retractor of 5 cm length was positioned first over the L3 right facet joint and fixed to the table. Under microscopic visualization, the right facet joint was exposed, and an L3 right-sided facetectomy was performed using an osteotome, preserving bone for autograft; a high-speed burr was not used. The exiting and traversing nerve roots and dural sac were carefully identified. Over-the-top technique was performed for the contralateral side by tilting the tubular retractor and rotating the operating table. Complete L3 discectomy and end-plate preparation were performed using minimally invasive instruments, and a PEEK TLIF cage packed with local bone graft was inserted. The same technique from the left side at L2-L3 was performed, and percutaneous modular pedicle screws (6.1 × 45 mm) were inserted in L2 and L3 vertebrae over the previously placed guidewires. To extend fixation, small incisions were reopened over the previous L3-L4 pedicle levels. The transpedicular screws were visualized by intra-operative X-ray; serial tubular dilators were advanced, and 22-mmdiameter tubular retractors were positioned above the L3 and L4 pedicle screws simultaneously. Screws were exposed under microscopic visualization, and The rod was identified. A rod advancer was positioned on it through the tubular retractor. After the caps were removed, the old rod was withdrawn, and a new longer rod was advanced across L2-L5 screws under fluoroscopic control. Screw caps were then tightened (Figure 3).The same procedure was performed on the left side. The surgery lasted 380 minutes with a blood loss of 240cc and X-ray exposure 222 μGy. On postoperative Day 2 his VAS was 2; he was mobilized the day after surgery and discharged on the 4th postoperative day. A control CT scan performed on the first postoperative day was unremarkable, verifying the perfect alignment and position of the posterior instrumentation and the PEEK cages.
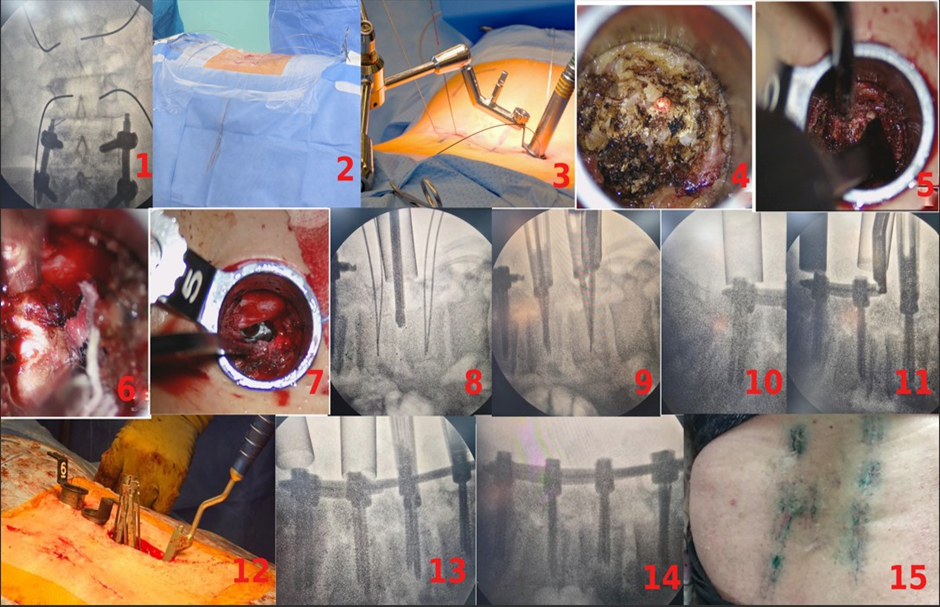
Figure 3: Surgical Technique After the operative level is marked and left and right pedicles are identified intraoperativelyusing a C-arm, 1-2 cm incision is made approximately 1 cm lateral to the pedicle projection and guidewires are placed bilaterally VIA Jamshidi needle (1,2). serial tubular dilators are advanced ipsilaterally and 22-mm diameter tubular retractor is positioned over the facet joint and rigidly fixed to the table (3). Under microscopic visualization, the facet joint is exposed (4), and a facetectomy is performed using an osteotome (5). (A high-speed burr is not used, as the removed bone is preserved for autografting). The exiting and traversing nerve roots and the dural sac are carefully identified (6). Complete discectomy and endplate preparation is performed with minimally invasiveinstruments and A PEEK TLIF cage filled with local bone graft is inserted into the disc space. (7, 8) percutaneous modular pedicle screws (6.1 × 45 mm) are inserted in L2 and L3 vertebrae over the previously placed guidewires (9) small incisions are reopened over the previous L3L4 pedicle levels. The transpedicular screws are visualized by intra-operative X-ray; serial tubular dilators are advanced, and 22-mmdiameter tubular retractor is positioned above the pedicle screw (10) The rod was identified. A rod advancer was positioned on it through the tubular retractor (11, 12), . After the caps were removed, the old rod was withdrawn, and a new longer rod was advanced across L2-L5 screws under fluoroscopic control (13, 14) Size of scar after 12 days of surgery (15) .
Discussion
Pathophysiology and Clinical Relevance
Adjacent Segment Disease (ASD) represents one of the most frequent long-term complications following lumbar fusion procedures. By eliminating motion at one vertebral level, fusion increases biomechanical stress on adjacent discs and facet joints, leading to accelerated degeneration and instability at neighboring levels [22]. Radiographic evidence of ASD has been reported in 5-27% of patients, although symptomatic cases are less common, typically emerging within two to five years after surgery [23,24]. The etiology of ASD remains controversial. One theory holds that adjacent segment pathologies are simply reflections of the natural history of lumbar degenerative disease, which is often characterized by desiccation of all lumbar segments, and are therefore inevitable. Others cite biomechanical findings to argue that LIF results in increased motion, intradiscal pressure, and strain adjacent to the fusion, leading to an increased risk of ASD [25,26]. In addition to altered biomechanics, pre-existing degeneration, surgical technique, sagittal balance, and patient-related factors such as age and body mass index contribute significantly. Despite efforts to minimize iatrogenic trauma through minimally invasive methods, fusion - regardless of approach - inevitably alters load transmission in the spinal column. In the present case, the patient developed symptomatic ASD two years following an initially successful single-level L4-L5 MISS TLIF. The degenerative process was confined to the cranial adjacent levels (L2-L3 and L3-L4), a pattern consistent with previous findings that cranial ASD occurs more frequently than caudal. Magnetic resonance and computed tomography imaging revealed Meyerding I spondylolisthesis and bilateral foraminal stenosis, while the original L4-L5 construct remained radiologically intact.
This clinical course underscores that even when an initial fusion is technically optimal, progressive degeneration at adjacent levels remains an intrinsic risk, necessitating careful long-term follow-up and patient counseling.
Technical Feasibility of Revision MISS TLIF
Revision MISS TLIF presents multiple challenges compared with primary minimally invasive procedures. The presence of prior instrumentation, altered anatomy, and epidural fibrosis complicates re-entry, raising the risk of dural injury and neural compromise. Regardless of its clinical relevance, there is a lack of publications dedicated to the revision or elongation of Minimally Invasive Surgery (MIS) TLIF. Despite these challenges, recent advances in tubular retractor design, fluoroscopic guidance, and surgical ergonomics have improved safety and efficiency. In the current case, the surgical team utilized the prior percutaneous access sites and screw trajectories to minimize additional softtissue damage. The previously fused L4-L5 level served as a stable foundation for extending the fixation cranially. A 22-mm tubular retractor provided sufficient exposure for decompression and interbody work. The over-the-top technique, performed by tilting the tubular retractor and rotating the operating table, permitted contralateral decompression without additional incisions. This preserved the minimally invasive character of the surgery while ensuring bilateral neural decompression. By employing serial tubular dilation and meticulous fluoroscopic control, exposurerelated morbidity was minimized. The new, longer rods spanning L2-L5 were inserted without extending the skin incisions beyond the prior scars. No intraoperative complications occurred, and estimated blood loss remained minimal (240 mL). The patient’s postoperative course was uneventful, demonstrating that with adequate surgical experience, MISS TLIF can be safely applied even in complex revision scenarios. The ability to extend fixation and decompress adjacent levels through previous incisions supports the adaptability of this technique for treating ASD.
Integration with Institutional Experience
Over the past decade, our institution has progressively transitioned from conventional open TLIF to MISS TLIF for lumbar degenerative disease. In a retrospective single-center analysis of 41 patients (22 open TLIF and 19 MISS TLIF), the minimally invasive approach demonstrated consistent perioperative and clinical advantages:
- Operative time: 267 ± 13.8 min (MISS) vs. 351 ± 11.9 min (open)
- Blood loss: 107 ± 3.9 mL (MISS) vs. 331 ± 25.4 mL (open)
- Hospital stay: 4.2 ± 0.3 days (MISS) vs. 6.7 ± 0.5 days (open)
- Fluoroscopy exposure: higher in MISS (137.8 ± 9.6 μGy vs. 53.2 ± 3.1 μGy)
At 6-month follow-up, ODI improved from 85.47 ± 6.21% → 6.10 ± 2.70% (MISS) and 85.63 ± 5.18% → 10.27 ± 2.66% (open). Fusion outcomes were comparable, with most patients achieving Bridwell I-II. No complications occurred in the MISS group; two occurred in the open group (one cage migration and one superficial wound infection). (Table 1)
|
Variable |
MIS TLIF |
Open TLIF |
P-value |
|
OP time (min) |
267 ± 13.8 |
351 ± 11.9 |
<0.0001 |
|
Intraoperative blood loss (cc) |
107 ± 3.9 |
331 ± 25.4 |
<0.0001 |
|
Hospital stay (days) |
4.2 ± 0.3 |
6.7 ± 0.5 |
<0.0001 |
|
Radiation exposure (μGy) |
137.8 ± 9.6 |
53.2 ± 3.1 |
<0.0001 |
|
Pre-OP VAS |
8.2 ± 0.2 |
8.9 ± 0.2 |
0.023 |
|
PreOp ODI (%) |
85.47 ± 6.21 |
85.63 ± 5.18 |
0.0001 |
|
Post-OP VAS 2nd day |
3.6 ± 0.3 |
6 ± 0.29 |
<0.0001 |
|
Post-OP VAS 5th day |
2.4 ± 0.2 |
4.8 ± 0.3 |
<0.0001 |
|
Post-OP VAS 12th day |
1.3 ± 0.1 |
2.2 ± 0.2 |
0.0007 |
|
Post-OP ODI ~6months (%) |
10.27 ± 2.66 |
6.1 ± 2.70 |
0.00012 |
|
Bridwell score: |
Number of Patients is MIS TLIF |
Number of Patients is Open TLIF |
|
|
I |
4 |
5 |
|
|
II |
11 |
13 |
|
|
III |
3 |
4 |
|
|
IV |
0 |
1 |
|
|
FollowUp Timing (months) |
MIS TLIF |
Open TLIF |
|
|
6.24 ± 0.34 |
6.4 ± 0.58 |
Table 1: Comparison of pre-, intra- and postoperative outcomes.
To ensure methodological consistency, strict selection criteria were applied:
Inclusion criteria
- Grade I-II spondylolisthesis
- Lumbar stenosis
- Recurrent herniated disc (≥ third recurrence)
- Large mediolateral protrusions requiring extensive decompression
- Significant coronal deformity
- Disease involving more than three levels
- Expected insufficient intraoperative visualization (for MISS TLIF only)
Exclusion criteria
Approximately 60 earlier open TLIF cases were excluded because they were performed without interbody cages, reflecting historical reimbursement restrictions. Only cases performed with interbody fusion and bilateral pedicle fixation were included for comparative analysis. This strict case selection ensured comparability between cohorts and strengthened the validity of the results. Furthermore, the efficiency of MISS TLIF reflected the lead surgeon’s extensive prior experience (over 500 tubular discectomies and ~400 percutaneous pedicle screw placements), effectively minimizing any learning-curve bias.
Challenges and Considerations
Revision and elongation of previously instrumented minimally invasive constructs remain among the most technically demanding spinal procedures. Limited visualization, dense scar tissue, and proximity of neural elements pose significant risks for dural tears or nerve root injury. The reuse of prior percutaneous screw trajectories requires precise alignment to avoid cortical breaches and hardware misplacement. In this case, re-exposure of prior pedicle screws through the same small incisions and reuse of screw channels allowed for safe elongation without the need for extensive dissection. Direct access using tubular retractors and fluoroscopic guidance ensured minimal additional trauma, and rod replacement was performed smoothly. Despite the complexity of reoperation, the procedure was completed without any intraoperative complications or neurological deficits, underscoring the technical feasibility and reproducibility of revision MISS TLIF when performed by experienced surgeons. Radiation exposure was higher than in primary MISS TLIF procedures but remained within acceptable safety thresholds. The operative duration, though prolonged, was consistent with previous studies reporting increased time requirements in revision MISS TLIF due to intraoperative precision demands. This experience reinforces that with adequate surgical expertise, appropriate patient selection, and careful intraoperative navigation, revision MISS TLIF can be performed safely even in limited-resource environments.
Conclusion
This case highlights that revision and elongation of prior minimally invasive lumbar fusions for adjacent segment disease are technically feasible and safe. MISS TLIF can provide excellent clinical and radiological outcomes when performed by experienced teams using standardized protocols. Reuse of prior incisions, precise trajectory alignment, and careful intraoperative planning allow for effective decompression and fusion with minimal morbidity.
References
- Wang MY, Grossman J, Mummaneni PV (2010) Minimally invasive transforaminal lumbar interbody fusion: review of techniques and outcomes. Neurosurg Focus 28: E10.
- Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ (2015) Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MIS-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg 1: 2-18.
- Parker SL, Mendenhall SK, Shau DN (2012) MIS-TLIF versus open TLIF: systematic review and meta-analysis. J Neurosurg Spine 17: 453-464.
- Harms J, Rolinger H (1982) A one-staged procedure in operative treatment of spondylolisthesis: dorsal traction-reposition and anterior fusion. Z Orthop 120: 343-347.
- Kim JS, Lee SH, Lee JH (2007) Effect of minimally invasive TLIF on paraspinal muscles and clinical outcomes. Spine (Phila Pa 1976) 32: 983-990.
- Wang H, Zhou Y, Zhang Z (2019) Comparative study of MIS-TLIF versus open TLIF: perioperative outcomes and complications. Clin Spine Surg 32: E271-E278.
- Mobbs RJ, Rao PJ, Phan K (2014) Correction of lumbar lordosis and coronal imbalance with TLIF: open vs minimally invasive. Eur Spine J 23: 196-204.
- Foley KT, Lefkowitz MA (2003) Advances in minimally invasive spine surgery. Clin Neurosurg 50: 1-12.
- Wang MY, Mummaneni PV (2010) Learning curve in minimally invasive spine surgery: implications for operative time and complications. Neurosurg Focus 28: E10.
- Rajpal S (2018) Fluoroscopic exposure and safety in MIS-TLIF. Spine J 18: 1417-1424.
- Phan K, Hogan JA, Mobbs RJ (2016) Learning curve for minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF): a systematic review. World Neurosurg 95: 179-188.
- Sulaiman WA, Singh M, Abdulrauf SI (2014) Minimally invasive versus open transforaminal lumbar interbody fusion: a comparative analysis of clinical and radiological outcomes. Neurosurg Focus 36: E9.
- Alamin TF (2015) Preliminary results of a multicenter randomized study to evaluate the effect of minimally invasive vs. open lumbar fusion on paraspinal musculature using MR imaging. Spine J 15: S45-S46.
- Bridwell KH (1995) Anterior cervical fusion assessment: a new classification. Spine (Phila Pa 1976) 20: 670-676.
- Lee KH, Yue WM, Yeo W, Soeharno H, Tan SB (2014) Learning curve of a complex surgical technique: minimally invasive transforaminal lumbar interbody fusion (MIS TLIF). J Spinal Disord Tech 27: E234-E240.
- Parker SL, Mendenhall SK, Shau DN (2011) Minimally invasive versus open transforaminal lumbar interbody fusion: economic analysis. J Neurosurg Spine 14: 537-543.
- Goldstein CL, Macwan K, Sundararajan K, Rampersaud YR (2016) Perioperative outcomes and adverse events of minimally invasive versus open posterior lumbar fusion: meta-analysis and systematic review. J Neurosurg Spine 24: 416-427.
- Villavicencio AT, Burneikiene S, Roeca C (2010) Minimally invasive versus open transforaminal lumbar interbody fusion. Surg Neurol Int 1: 12.
- Yuan C, Zhou J, Wang L, Deng Z (2022) Adjacent segment disease after minimally invasive transforaminal lumbar interbody fusion for degenerative lumbar diseases: incidence and risk factors. BMC Musculoskelet Disord 23: 982.
- Jiawen Y, Sizhen Y, Zihan W, Chenhui C, Ying Z, et al. (2021) Incidence and Risk Factors for Adjacent Segment Disease After Transforaminal Lumbar Interbody Fusion in Patients with Lumbar Degenerative Diseases. International Journal of General Medicine 14: 8185-8192.
- Parker SL, Adamson T, McGirt M, Deshmukh V (2014) 152 Rate of Symptomatic Adjacent Segment Disease After Minimally Invasive vs Open Transforaminal Lumbar Interbody Fusion. Neurosurgery 61: 210.
- Galetta MS, Lorentz NA, Lan R, Chan C, Zabat, Michelle MA (2023) Reoperation Rates Due to ASD following Primary 1-2 level MIS vs. Open TLIF. Spine 48: 1295-1299.
- Zhong ZM, Deviren V, Tay B, Burch S, Berven SH (2017) Adjacent segment disease after instrumented fusion for adult lumbar spondylolisthesis: incidence and risk factors. Clinical Neurology and Neurosurgery 156: 29-34.
- Sato S, Yagi M, Machida M, Yasuda A, Konomi T, Miyake A (2015) Reoperation rate and risk factors of elective spinal surgery for degenerative spondylolisthesis: minimum 5-year follow-up. The Spine Journal 15: 1536-1544.
- Radcliff KE, Kepler CK, Jakoi A, Sidhu GS, Rihn J, et al. (2013) Adjacent segment disease in the lumbar spine following different treatment interventions. Spine J 13: 1339-1349.
- Schlegel JD, Smith JA, Schleusener RL (1996) Lumbar motion segment pathology adjacent to thoracolumbar, lumbar, and lumbosacral fusions. Spine (Phila Pa 1976) 21: 970-981.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.