Symptomatic and Asymptomatic West Nile Fever Virus among Sudanese Population
by Sara Elsadig Elagib Eltahir1, Nasir Adam Ibrahim2*, Omer Hassan Mohamed3
1Faculty of Medical Laboratory Sciences, University of Gezira, Sudan
2Department of Biology, Imam Mohammad Ibn Saud Islamic University (IMSIU), Saudi Arabia
*Corresponding author: Nasir Adam Ibrahim, Department of Biology, College of Science, Imam Mohammad Ibn Saud Islamic University (IMSIU), Riyadh 13318, Saudi Arabia
Received Date: 06 July, 2025
Accepted Date: 16 July, 2025
Published Date: 18 July, 2025
Citation: Eltahir SEE, Ibrahim NA, Mohamed OH (2025) Symptomatic and Asymptomatic West Nile Fever Virus among Sudanese Population. J Med Biomed Discoveries 7: 140. https://doi.org/10.29011/2688-8718.100140.
Abstract
West Nile virus one of Flavivirus genus, Family Flaviviridae, West Nile virus (WNV) is a mosquito-borne flavivirus, it causes west Nile fever, it also, causes in less than 1% of infections a west Nile neuroinvasive disease (WNND) with an approximate 10% fatality. This cross-sectional study aims to detect WNV among citizens of Gezira State, Sudan. This study was done in 400 people during the period 2019 to 2022. Five ml of blood sample were collected in 2 ml in EDTA tube in 3 ml plain container, plasma and serum was collected after centrifugation of the blood. IgG and IgM of WNV were detected using ELISA method, then RT-PCR was performed to detect the virus in WNV-IgG positive samples. The serological detection by using WNV-IgG antibodies showed that 249 cases (62.25%) were positive, and 151 cases (37.75%) were negative. While all samples are negative for WNV-IgM antibodies. This study showed that there was no significant correlation between the risk factors and occurrence of WNV-IgG antibodies, P > 0.05, except for neck stiffness there was significant correlation with occurrence of WNV-IgG antibodies P < 0.05. In the diagnosis of WNV using WNV-IgM antibodies, all the study populations, 400 samples were negative (100%), this is due to status of the patients as most of them in chronic stage of infection. The study concluded that the study population were in chronic stage of infection with WNV. Recommended the necessity of continuous surveillance of WNV and other vector-borne diseases in the region, to find active WNV infections. Public health initiatives could focus on preventive measures, education about mosquito control, and awareness campaigns regarding the symptoms of WNV.
Keywords: WNV and symptoms, WNV and risk.
Introduction
West Nile virus (WNV) is a single-stranded RNA, a mosquito-borne flavivirus causing subclinical or mild infection to humans. It causes west Nile fever (WNF), it also, causes in less than 1% of infections a west Nile neuroinvasive disease (WNND) with an approximate 10% fatality [1-4].
The virus was discovered in Uganda in 1937 and was first detected in North America in 1999 [5-9]. West Nile Virus has occurred in Europe, Africa, Asia, Australia, and North America. In the United States thousands of cases are reported per a year, with most occurring in August and September. It can occur in outbreaks of disease [5,9].
West Nile fever is an infection caused by the West Nile virus, which is typically spread by mosquitoes. In about 80% of infections people have few or no symptoms 20% of people develop a fever, headache, vomiting, or a rash. In less than 1% of people, encephalitis or meningitis occurs, with associated neck stiffness, confusion, or seizures. Recovery may take weeks to months. The risk of death among those in whom the nervous system is affected is about 10 % [5]. West Nile virus (WNV) is usually spread by infected mosquitoes. Mosquitoes become infected when they feed on infected birds, which often carry the disease. Rarely the virus is spread through blood transfusions, organ transplants, or from mother to baby during pregnancy, delivery, or breastfeeding. It does not spread directly between people (WHO, 2011). Risks for severe disease include being over 60 years old and having other health problems. Diagnosis is typically based on symptoms and blood tests [5].
The disease's clinical presentation has changed since the mid‐1990s [2]. Earlier, WNV epidemics were mainly, although not exclusively, characterized by cases of fever, accompanied by rash and lymphadenopathy [6]. In contrast, during recent epidemics in Romania 1996 [8], Russia 1999 [7], the United States of America 1999 [1] and Israel 2000 [4], encephalitis has dominated the clinical presentation while rash or lymphadenopathy have rarely been observed.
Culex mosquito which play an important role in the transmission of many infectious agent including West Nile virus (WNV) have an epidemic prevalence in Sudan especially in Gezira state. This high epidemiology of Culex in such area may result in high incidence of that viral disease which may be misdiagnosed with disease shared many symptoms with these diseases. Moreover, WNV if not managed carefully may result in severe complications which could be neuralgic disorder such as encephalitis or meningitis. Despite the abovementioned facts very few data were available about the epidemiology of WNV in Sudan and most previous studies were focused on the prevalence of the WNV disease among blood donors.
Therefore, the current research aims to identify the epidemiology of the WNV disease among Sudanese participant in Gezira state by using WNV IgM and IgG antibodies to estimate the prevalence of WNV among Sudanese and to identify risk factors related to WNV.
Materials and Methods
Study design is a cross-sectional laboratory-based study. The study will be conducted in Sudan Gezira state, Localities of Gezira state. This study was done in the period from February (2022) to December (2022). This study was done in Sudan according to inclusion and exclusion criteria. Symptomatic and asymptomatic participant were included.
Blood samples (5ml) were aseptically withdrawn from each of the study participants 2 ml into EDTA and 3ml plain container. serum will be separated after ten minutes of collection while plasma immediately, by centrifuging the sample for 5 minutes at 3000 rpm, and then the serum will be transferred to labelled Eppendorf safe–lock tubes with cap. And was stored at -20ºC until used. The size of the sample used to study a proportion within a population is a critical factor to obtain reliable results about the proportion in the whole population. The reliability of the data is never absolute but is located within an interval of confidence. The smaller the interval must be, or the lower the error rate must be, the larger the sample size must be in order to get an accurate reflection of the proportion within the population as a whole. According to the formula the sample size was 384 patients from each locality of Gezira state.
Data was collected for clinical symptoms and risk factors. The collected data and results were entered in a high probability of being infected with analysed using the Statistical Package for Social Sciences (SPSS, Version 22) computer program. The ethical approval and permission were obtained from the Faculty of Medical Laboratory Sciences, University of Gezira. Gezira State Ministry of health authorities and consent obtain from the participation, under privacy and confidentiality and did not used for any purposes rather than this study.
The test kit provides a semiquantitative in vitro assay for human antibodies of the IgM/IgG class against West Nile virus in serum or plasm break-off reagent wells coated with West Nile virus antigens, in the first reaction step, diluted patient samples are incubated in the wells, in the case of positive sample, specific IgM /IgG antibodies bind to the antigen. To detect the bound antibodies, a second incubation is carried out using an enzyme – labelled anti-human IgM/IgG (enzyme conjugate) catalysing colour reaction. Sample dilution and test performance are carried out fully automatically using the analysis device.
The extinction value of the calibrator defines the upper limit of the reference range of non-infected person (cut-off) recommended by EUROIMMUM. Values above the indicated cut-off are to be considered as positive, those below as negative. Semiquantitative: Results can be evaluated by calculating a ratio of the extinction value of the control or patient sample over the extinction value of calibrator. Interpretation of Result of IgG/IgM, according to EUROIMMUM recommended interpreting results as follows: Ratio > 0.8 = negative, Ratio >/=0.8 to < 1.1= borderline and Ratio >/= 1.1= positive
Results
The serological detection by using WNV-IgG antibodies showed that 249 cases (62.25%) were positive, and 151 cases (37.75%) were negative. While all samples are negative for WNV-IgM antibodies 12 of them were borderline. The pooled IgG seroprevalence of West Nile Virus was high (62.3%) of samples (table 1).
|
WNV antibodies (n=400) |
Frequency |
Percent |
|
|
IgG antibodies |
Negative |
151 |
37.7 |
|
Positive |
249 |
62.3 |
|
|
Borderline |
0 |
0 |
|
|
IgM antibodies |
Negative |
388 |
97 |
|
Positive |
0 |
0 |
|
|
Borderline |
12 |
3 |
|
Table 1: The characteristics and patterns of WNV IgG and IgM antibodies in the study population.
The distribution of symptoms among the 400 participants is as follows: Fever was reported by 13.5% (54 participants), while 86.5% (346 participants) did not experience it. Vomiting was reported by 6.8% (27 participants), with 93.3% (373 participants) not experiencing it. Rash was present in 5.5% (22 participants), while 94.5% (378 participants) did not report it. Headache was experienced by 16.3% (65 participants), while 83.8% (335 participants) did not report it. Neck stiffness was reported by 2.5% (10 participants), and 97.5% (390 participants) did not have this symptom. Flu-like symptoms were present in 13.8% (55 participants), while 86.3% (345 participants) did not experience them in Table 2 and figure 1.
|
Symptoms (n=400) |
No |
Yes |
||
|
Frequency |
Percent |
Frequency |
Percent |
|
|
Fever |
346 |
86.5 |
54 |
13.5 |
|
Vomiting |
373 |
93.3 |
27 |
6.8 |
|
Rash |
378 |
94.5 |
22 |
5.5 |
|
Headache |
335 |
83.8 |
65 |
16.3 |
|
Neck stiffness |
390 |
97.5 |
10 |
2.5 |
|
Flue like |
345 |
86.3 |
55 |
13.8 |
Table 2: The distribution of symptoms among the study Population.
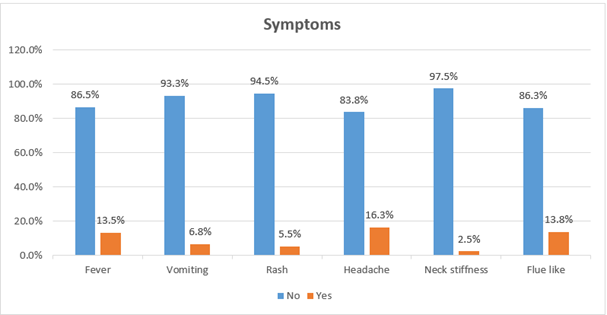
Figure 1: Symptoms distribution of the study Population.
The medical background of the participants is as follows: 95.3% (381 participants) did not report a chronic disease, while 4.8% (19 participants) did. Regarding blood transfusions, 98.8% (395 participants) did not have a history of blood transfusion, while 1.3% (5 participants) had undergone one. All participants (100%) reported no history of organ transplantation (Table 3 and figure 2).
|
Medical History (n=400) |
No |
Yes |
||
|
Frequency |
Percent |
Frequency |
Percent |
|
|
Chronic disease |
381 |
95.3 |
19 |
4.8 |
|
Blood transfusion |
395 |
98.8 |
5 |
1.3 |
|
Organ transplantation |
400 |
100 |
0 |
0 |
Table 3: The medical background of the study population.
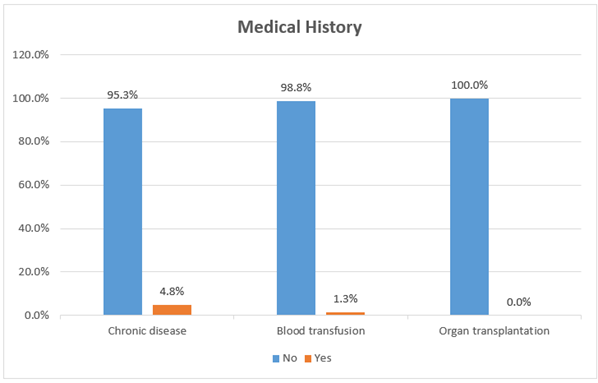
Figure 2: The medical background of the study population.
|
WNV-IgG antibodies |
Chi-Square |
P. value |
|||||
|
Negative (n=151) |
Positive (n=249) |
||||||
|
n |
% |
N |
% |
||||
|
Fever |
No (n=346) |
136 |
90.10% |
210 |
84.30% |
2.642 |
0.104 |
|
Yes (n=54) |
15 |
9.90% |
39 |
15.70% |
|||
|
Vomiting |
No (n=373) |
139 |
92.10% |
234 |
94.00% |
0.552 |
0.457 |
|
Yes (n=27) |
12 |
7.90% |
15 |
6.00% |
|||
|
Rash |
No (n=378) |
146 |
96.70% |
232 |
93.20% |
2.236 |
0.135 |
|
Yes (n=22) |
5 |
3.30% |
17 |
6.80% |
|||
|
Headache |
No (n=335) |
128 |
84.80% |
207 |
83.10% |
0.185 |
0.667 |
|
Yes (n=65) |
23 |
15.20% |
42 |
16.90% |
|||
|
Neck stiffness |
No (n=390) |
143 |
94.70% |
247 |
99.20% |
7.791 |
0.005* |
|
Yes (n=10) |
8 |
5.30% |
2 |
0.80% |
|||
|
Flue like |
No (n=345) |
134 |
88.70% |
211 |
84.70% |
1.27 |
0.26 |
|
Yes (n=55) |
17 |
11.30% |
38 |
15.30% |
|||
Table 4: Correlation between WNV-IgG antibodies and clinical symptoms.
Table (4) presents the correlation between WNV-IgG antibodies and various symptoms. Most symptoms, including fever, vomiting, rash, headache, and flu-like symptoms, showed no significant association with WNV-IgG positivity, as their P-values were above 0.05. However, Table (5) present the correlation between WNV-IgM antibodies and various symptoms. None of the symptoms, including fever, vomiting, rash, headache, neck stiffness, and flu-like symptoms, showed a statistically significant association with WNV-IgM status (P > 0.05).
The table examines the association between WNV-IgG antibodies and medical history. The analysis showed no significant association between WNV-IgG antibodies and medical history variables, as both chronic disease (P = 0.688) and blood transfusion history (P = 0.080), neck stiffness was significantly associated with WNV-IgG antibodies (P = 0.005), with 5.3% of IgG-negative participants reporting neck stiffness compared to only 0.8% of IgG-positive participants.
|
WNV-IgM antibodies |
Chi-Square |
P. value |
|||||
|
Negative (n=388) |
Borderline (n=12) |
||||||
|
n |
% |
n |
% |
||||
|
Fever |
No (n=346) |
335 |
86.30% |
11 |
91.70% |
0.283 |
0.595 |
|
Yes (n=54) |
53 |
13.70% |
1 |
8.30% |
|||
|
Vomiting |
No (n=373) |
361 |
93.00% |
12 |
100.00% |
0.895 |
0.344 |
|
Yes (n=27) |
27 |
7.00% |
0 |
0.00% |
|||
|
Rash |
No (n=378) |
367 |
94.60% |
11 |
91.70% |
0.191 |
0.662 |
|
Yes (n=22) |
21 |
5.40% |
1 |
8.30% |
|||
|
Headache |
No (n=335) |
323 |
83.20% |
12 |
100.00% |
2.4 |
0.121 |
|
Yes (n=65) |
65 |
16.80% |
0 |
0.00% |
|||
|
Neck stiffness |
No (n=390) |
378 |
97.40% |
12 |
100.00% |
0.317 |
0.573 |
|
Yes (n=10) |
10 |
2.60% |
0 |
0.00% |
|||
|
Flue like |
No (n=345) |
334 |
86.10% |
11 |
91.70% |
0.306 |
0.58 |
|
Yes (n=55) |
54 |
13.90% |
1 |
8.30% |
|||
Table 5: Correlation between WNV-IgM antibodies and clinical symptoms.
|
WNV-IgM antibodies |
Chi-Square |
P. value |
|||||
|
Negative (n=388) |
Borderline (n=12) |
||||||
|
n |
% |
n |
% |
||||
|
Chronic disease |
No (n=381) |
143 |
94.70% |
238 |
95.60% |
0.161 |
0.688 |
|
Yes (n=19) |
8 |
5.30% |
11 |
4.40% |
|||
|
Blood transfusion |
No (n=395) |
151 |
100.00% |
244 |
98.00% |
3.071 |
0.08 |
|
Yes (n=5) |
0 |
0.00% |
5 |
2.00% |
|||
Table 6: Correlation between WNV-IgG antibodies and medical history.
Table (6) present the correlation between WNV-IgG antibodies and medical history. The analysis showed no significant association between WNV-IgG antibodies and medical history variables, as both chronic disease (P = 0.688) and blood transfusion history (P = 0.08).
|
WNV-IgM antibodies |
Chi-Square |
P. value |
|||||
|
Negative (n=388) |
Borderline (n=12) |
||||||
|
n |
% |
n |
% |
||||
|
Chronic disease |
No (n=381) |
369 |
95.10% |
12 |
100.00% |
0.617 |
0.432 |
|
Yes (n=19) |
19 |
4.90% |
0 |
0.00% |
|||
|
Blood transfusion |
No (n=395) |
383 |
98.70% |
12 |
100.00% |
0.157 |
0.692 |
|
Yes (n= 5) |
5 |
1.30% |
0 |
0.00% |
|||
Table 7: Correlation between WNV-IgM antibodies and medical history.
Table (7) present the correlation between WNV-IgM antibodies and medical history. The analysis showed no significant association between WNV-IgM antibodies and medical history variables, as both chronic disease (P = 0.432) and blood transfusion history (P = 0.692).
|
Factors |
P. value |
Odds ratio |
95% confidence interval |
|
|
Lower |
Upper |
|||
|
Fever |
0.278 |
1.527 |
0.711 |
3.283 |
|
Vomiting |
0.14 |
0.499 |
19.80% |
1.256 |
|
Rash |
0.628 |
1.355 |
39.70% |
4.632 |
|
Headache |
0.846 |
1.071 |
53.40% |
2.151 |
|
Neck stiffness |
0.006* |
0.082 |
1.40% |
0.486 |
|
Flue like |
0.314 |
1.466 |
0.696 |
3.087 |
|
Chronic disease |
0.365 |
1.818 |
0.499 |
6.63 |
|
Blood transfusion |
0.999 |
0 |
0 |
. |
|
*. significant at the 0.05 level |
||||
Table 8: Logistic regression analysis of factors associated with WNV-IgG seropositivity.
Table (8) presents the logistic regression analysis of factors associated with WNV-IgG positivity. Significant associations were observed for gender (P = 0.017, OR = 1.815, 95% CI: 1.113–2.961), educational level (P = 0.004, OR = 1.417, 95% CI: 1.119–1.795), marital status (P = 0.004, OR = 0.325, 95% CI: 0.151–0.699), and neck stiffness (P = 0.006, OR = 0.082, 95% CI: 0.014–0.486). Other variables, including age, fever, vomiting, rash, headache, flu-like symptoms, chronic disease, and blood transfusion history, did not show statistically significant associations with WNV-IgG positivity.
|
Factors |
P. value |
Odds ratio |
95% confidence interval |
|
|
Lower |
Upper |
|||
|
Fever |
0.806 |
0.731 |
0.06 |
8.841 |
|
Vomiting |
0.998 |
0 |
0 |
. |
|
Rash |
0.295 |
4.088 |
0.293 |
56.939 |
|
Headache |
0.997 |
0 |
0 |
. |
|
Neck stiffness |
0.999 |
0 |
0 |
. |
|
Flue like |
0.96 |
0.939 |
0.084 |
10.498 |
|
Chronic disease |
0.998 |
0 |
0 |
. |
|
Blood transfusion |
0.999 |
0 |
0 |
. |
Table 9: Logistic regression analysis of factors associated with WNV-IgM seropositivity.
Table (9) presents the logistic regression analysis of factors associated with WNV-IgM borderline results. No significant associations were observed for age, gender, educational level, marital status, number of children, fever, vomiting, rash, headache, neck stiffness, flu-like symptoms, chronic disease, or blood transfusion history.
Discussion
Although the West Nile Virus is increasingly widespread in SUDAN, particularly in Gezira state, there is still a lack of clarity regarding its extent and distribution due to limited surveillance and inadequate diagnostic tests. As it knows the diagnosis of WNV depends on serological and molecular methods by using WNV-IgG or WNV-IgM antibodies, so we use ELISA technique. The sample population included 400 samples to study the relationship between symptoms, fever, vomiting, rash, headache, neck stiffness, flu-like symptoms, and medical history that include chronic disease and blood transfusion, and the present of WNV-IgG or WNV-IgM antibodies.
The serological detection by using WNV-IgG antibodies showed that 249 cases (62.25%) were positive, and 151 cases (37.75%) were negative. While all samples were negative for WNV-IgM antibodies 12 of them were borderline. The high rate of IgG positivity suggests a significant portion of the sampled population has been exposed to the West Nile Virus at some point in their lives. IgG antibodies indicate a past infection or vaccination response.
This study showed that there was no significant correlation between the symptoms and occurrence of WNV-IgG antibodies, P>0.05, except for neck stiffness there was significant correlation with occurrence of WNV-IgG antibodies P<0.05. The finding in this study differs from those reported in previous study conducted in Africa which indicated pooled seroprevalences of 70.3% for West Nile virus IgG in Sudan, and like another study in blood doner in Sudan 2022 which showed 67(74.4%) of participants had positive WNV IgG. Other variables, including age, fever, vomiting, rash, headache, flu-like symptoms, chronic disease, and blood transfusion history, did not show statistically significant associations with WNV-IgG positivity. Although the West Nile Virus is increasingly widespread in Sudan, particularly in Gezira state, there is still a lack of clarity regarding its extent and distribution due to limited surveillance and inadequate diagnostic tests.
However, this study has several limitations, factors such as the time of sampling relative to potential exposure, limitations in testing methods, and geographical coverage should be considered. The study only reflects the situation during the sampling period and may not fully capture the dynamics of WNV transmission in Gezira State.
Various factors contribute to this variability. These factors include differences in study period, heterogeneity of study populations, sample size and study design. Additionally, other factors, such as ecological environment, climate, vector abundance and diagnostic and surveillance capabilities of West Nile virus, may significantly contribute to the observed variability. Investigating mosquitoes can help in understanding the spread of the virus, identifying areas at high risk, and guiding control efforts to reduce the incidence of infection in the population.
According to previous research in blood donor in Sudan WNV screening test should be part of blood transfusion screening tests in Sudan as the blood transfusion is one of the routes that lead to WNV distribution. These findings underline the necessity for continuous surveillance of WNV and other vector-borne diseases in the region, to find active WNV infections. Public health initiatives could focus on preventive measures, education about mosquito control, and awareness campaigns regarding the symptoms of WNV. The results obtained from this study may help the physician to save more lives of patients who are misdiagnosed with malaria or other fever induced disease and they were treated incorrectly.
References
- Anonymous (MMWR) (1999) Outbreak of West Nile-like viral encephalitis--New York, 1999. MMWR Morb Mortal Wkly Rep 48: 845-849.
- Campbell GL, Marfin AA, Lanciotti RS, Gubler DJ (2002) West Nile virus. Lancet Infect Dis 2: 519-529.
- CDC (2019) Symptoms, Diagnosis, & Treatment.
- Chowers MY, Lang R, Nassar F, D Ben-David, M Giladi, et al. (2001) Clinical characteristics of the West Nile fever outbreak, Israel, 2000. Emerging Infectious Diseases 7: 675-678.
- (2017) General Questions About West Nile Virus.
- Marberg K, Goldblum N, Sterk VV, Jasinska-Klingberg W, Klingberg MA (1956) The natural history of West Nile fever. Clinical observations during an epidemic in Israel. Am J Hyg 64: 259-269.
- Platonov AE, Shipulin GA, Shipulina OY, E N Tyutyunnik, T I Frolochkina (2001) Outbreak of West Nile virus infection, Volgograd region, Russia, 1999. Emerging Infectious Diseases 7: 128-132.
- Tsai TF, Popovici F, Cernescu C, Campbell GL, Nedelcu NI (1998) West Nile encephalitis in south-eastern Romania. Lancet 352: 767–771.
- World Health Organization (2011) West Nile virus.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.