Surgical Management of Hematometra and Hematosalpinx Following Endometrial Ablation in Patients with Endometriosis
by Ahmed Ghareeb Mahmoud, Randa Eliwa
Obstetrics and Gynecology, Specialty Doctor, Glangwili General hospital , UK
*Corresponding author: Ahmed Ghareeb Mahmoud, Obstetrics and Gynecology, Specialty Doctor, Glangwili General hospital, UK
Received Date: 30 June 2025
Accepted Date: 09 July 2025
Published Date: 14 July 2025
Citation: Mahmoud AG, Eliwa R (2025) Surgical Management of Hematometra and Hematosalpinx Following Endometrial Ablation in Patients with Endometriosis. Gynecol Obstet Open Acc 9: 239. https://doi.org/10.29011/2577-2236.100239.
Abstract
Background: Endometrial ablation is a widely used minimally invasive treatment for menorrhagia. Although generally safe, it can lead to rare but serious complications such as cervical stenosis and hematometra. In some cases, obstruction of the cervical canal may result in retrograde menstrual flow, leading to hematosalpinges.
Case Presentation: We report the case of a 48-year-old woman who underwent endometrial ablation for refractory menorrhagia. The patient subsequently developed secondary amenorrhea and cyclic pelvic pain. Imaging revealed hematometra and bilateral hematosalpinx secondary to cervical stenosis. Surgical management included cervical dilation and drainage of the hematometra, with eventual resolution of symptoms.
Discussion: This case highlights a rare but important complication of endometrial ablation. Cervical stenosis can lead to outflow obstruction, resulting in hematometra. Similar cases in the literature have demonstrated the need for prompt diagnosis and surgical intervention to prevent further complications. Various management strategies—including cervical dilation, hysteroscopic intervention, or hysterectomy—may be employed depending on the severity and patient’s reproductive goals.
Conclusion: Clinicians should maintain a high index of suspicion for hematometra in postablation patients presenting with secondary amenorrhea and pelvic pain. Early imaging and appropriate surgical intervention are key to successful management.
Keywords: Hematometra, Endometrial ablation, Cervical stenosis, Hematosalpinx, Menorrhagia, Surgical management
Introduction
Hematometra, the accumulation of blood within the uterine cavity, is a rare but significant complication following endometrial ablation—a procedure commonly used to treat menorrhagia. One of the primary causes is cervical stenosis, which obstructs menstrual blood flow, potentially leading to retrograde blood accumulation and subsequent complications such as hematosalpinx. Although often under-recognized, these conditions can present with secondary amenorrhea and pelvic pain. Prompt diagnosis and appropriate surgical management are essential to prevent longterm morbidity [1,2].
The clinical presentation of hematometra can vary, with patients often experiencing symptoms such as secondary amenorrhea, cyclic pelvic pain, and abdominal distension. In severe cases, the accumulation of blood can lead to significant uterine enlargement, mimicking a gravid uterus. Diagnosis is typically confirmed through imaging modalities like ultrasound or MRI, which reveal the presence of blood within the uterine cavity and may also show associated conditions like hematosalpinx [2].
Objectives of the Case Report:
To present a rare complication of endometrial ablation— hematometra and hematosalpinx—resulting from post-procedural cervical stenosis.
- To highlight the clinical presentation of hematometra, including secondary amenorrhea and cyclic pelvic pain, in the context of a previously ablated endometrium.
- To emphasize the importance of early diagnosis using appropriate imaging modalities (e.g., transvaginal ultrasound, MRI) in identifying retained intrauterine and adnexal blood collections.
- To discuss surgical management strategies, including cervical dilation and drainage, and explore alternatives such as hysterectomy for cases unresponsive to conservative approaches.
- To compare and contextualize the case with similar
reports in the literature, reinforcing the need for awareness of postablation complications among clinicians.
Case presentation
A 48-year-old para 3 woman (two normal vaginal deliveries and one Caesarean section) presented with constant lower abdominal pain and secondary amenorrhea. Her initial complaint was localized right iliac fossa pain, which was managed with appendicectomy under a provisional diagnosis of appendicitis. Despite the procedure, the patient continued to experience chronic lower pelvic pain.
Her medical history was notable for endometriosis, previously well-controlled with Zoladex (goserelin), which was later discontinued with a transition to patient-initiated follow-up under the assumption of an upcoming laparoscopy. She had undergone endometrial ablation three years prior, which eliminated her menstrual bleeding but did not resolve her cyclical pelvic pain. Additional symptoms included severe dyschezia, dyspareunia (with post-coital pain lasting several days), and persistent pelvic discomfort.
Surgical history included appendicectomy, Caesarean section, and cholecystectomy
Investigations
CT Abdomen and Pelvis
- Revealed complex bilateral multiloculated ovarian cysts, a distended endometrial cavity (73 mm AP × 93 mm transverse), and thickened pelvic tissues.
- A new right iliac fossa cystic lesion measuring 64 mm raised concerns for chronic or superinfected pathology.
- Free pelvic fluid and tissue thickening suggested endometriosis or pelvic inflammatory disease.
- Noted prior cholecystectomy and a small hiatus hernia.
- Demonstrated a retroflexed, anteverted uterus with a distended endometrial cavity (13 mm), filled with haemorrhagic material (hematometra).
- Posterior uterine wall exhibited diffuse adenomyosis (20 mm depth, 3.7 cm length).
- Bilateral adnexal cystic structures were consistent with hematosalpinx (up to 4.3 cm on the left).
- Multiple low-signal endometriotic nodules were identified in the pelvic sidewalls and pouch of Douglas.
- Overall findings confirmed hematometra with bilateral hematosalpinx in the context of advanced endometriosis.
MRI Pelvis
Management: Initial management included:
- Hormonal suppression using Zoladex followed by
Ryeqo (relugolix, estradiol, norethisterone acetate).
- Drainage of hematometra under general anaesthesia was performed through cervical dilatation under ultrasound guidance, due to worsening pelvic pressure symptoms and progressive distension seen on imaging. See pic [1,2]
- The patient was referred to a tertiary endometriosis center for multidisciplinary evaluation and surgical planning.
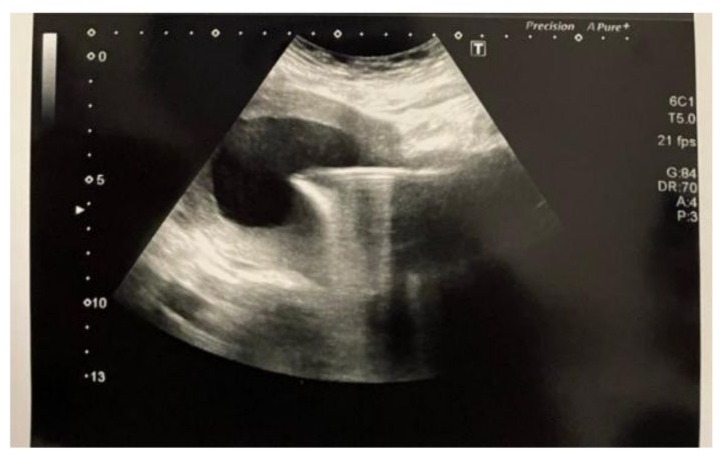
Figure 1: Abdominal Ultrasound Showing Hematometra, Before Operation.

Figure 2: Abdominal Ultrasound Post Drainage of Hematometra Showing Empty Uterus.
Literature Review: Hematometra Following Endometrial Ablation
Hematometra, the accumulation of blood within the uterine cavity, is a rare but significant complication following endometrial ablation procedures. This condition can result from cervical stenosis or scarring, which obstructs the normal outflow of menstrual blood, leading to symptoms such as secondary amenorrhea, cyclic pelvic pain, and abdominal distension.
A retrospective study involving 50 patients who underwent total rollerball endometrial ablation for dysfunctional uterine bleeding reported an incidence of symptomatic cornual hematometra or post-ablation tubal sterilization syndrome (PATSS) in 10% of cases. These patients experienced symptoms ranging from 4 to 90 months post-procedure. Management strategies included gonadotropin-releasing hormone agonist treatment, hysteroscopic decompression, and, in some cases, hysterectomy with salpingectomy. The study emphasized the importance of early diagnosis and intervention to prevent recurrence and alleviate symptoms [4,3].
Another study highlighted that the incidence of PATSS is approximately 6–8% and usually develops 2–3 years after endometrial ablation. The pathophysiology involves retrograde menstruation of cornual hematometra against an obstructed fallopian tube, causing visceral distention and pain. The definitive treatment for PATSS is typically hysterectomy, although laparoscopic tubal occlusion can be performed concurrently with the ablation procedure to prevent this complication [5].
A case report described a patient who developed cervical occlusion and hematometra following thermal balloon endometrial ablation. The patient had a history of cervical incompetence during pregnancy, which may have predisposed her to cervical scarring and subsequent stenosis. Management involved cervical dilation and temporary placement of a catheter as a stent, leading to resolution of the condition [6].
These cases underscore the importance of considering cervical stenosis as a potential complication following endometrial ablation. Early recognition and appropriate management are crucial to prevent long-term morbidity. Management strategies may include cervical dilation, hysteroscopic intervention, or, in severe cases, hysterectomy. Preventive measures, such as careful technique during the ablation procedure to minimize cervical trauma and the use of partial rollerball ablation to avoid extensive scarring, have been suggested to reduce the risk of hematometra [7].
In conclusion, hematometra following endometrial ablation is a significant complication that requires prompt recognition and appropriate management. A multidisciplinary approach involving gynecologists, radiologists, and, when necessary, surgical intervention, is crucial in addressing this condition effectively [3].
Case Discussion
Hematometra, the accumulation of blood within the uterine cavity, is a recognized complication following endometrial ablation procedures. This condition can result from cervical stenosis or scarring, which obstructs the normal outflow of menstrual blood, leading to symptoms such as secondary amenorrhea, cyclic pelvic pain, and abdominal distension [8].
In the presented case, a 48-year-old woman developed hematometra and hematosalpinx following endometrial ablation for menorrhagia. The onset of secondary amenorrhea due to cervical stenosis led to the accumulation of blood within the uterine cavity and fallopian tubes. This scenario underscores the importance of considering cervical stenosis as a potential complication following endometrial ablation and highlights the need for prompt diagnosis and intervention [2].
Management strategies for hematometra secondary to cervical stenosis often involve surgical intervention. Cervical dilation procedures, sometimes guided by ultrasound, are commonly performed to relieve the obstruction and allow for the drainage of accumulated blood. In cases where dilation is unsuccessful or the stenosis is severe, more invasive surgical options, including hysterectomy, may be considered.
It is essential to recognize that the risk of developing hematometra increases in patients who have undergone concurrent endometrial ablation and tubal sterilization. This combination can lead to postablation tubal sterilization syndrome (PATSS), characterized by unilateral or bilateral pelvic pain and vaginal spotting, resulting from obstructed fallopian tubes and retained menstrual blood. The incidence of PATSS has been reported to be approximately 8–33%.
Preventive measures include careful technique during the ablation procedure to minimize cervical trauma and the use of partial rollerball ablation to avoid extensive scarring. Additionally, regular follow-up and imaging can aid in the early detection of complications, allowing for timely intervention and preservation of fertility when possible.
In conclusion, hematometra following endometrial ablation is a significant complication that requires prompt recognition and appropriate management. A multidisciplinary approach involving gynecologists, radiologists, and, when necessary, surgical intervention, is crucial in addressing this condition effectively.
Conclusion
Hematometra and hematosalpinx are rare but serious complications that can occur following endometrial ablation, particularly in the presence of cervical stenosis. This case highlights the importance of maintaining clinical vigilance in patients who present with secondary amenorrhea and pelvic pain after ablation procedures. Early imaging and timely surgical intervention—such as cervical dilation or, in severe cases, hysterectomy—are critical to effective management and symptom resolution. Increased awareness and prompt recognition of these complications can improve outcomes and reduce the risk of long-term reproductive and gynecological sequelae.
References
- Agrawal S, Sahu R, Thakur P, Singh V, Chandramohan PB (2019). Recurrent hematometra with endometriosis in an adolescent girl: a case report. International Journal of Reproduction, Contraception, Obstetrics and Gynecology 8: 4567–4569.
- Hill DJ (1994) Hematometra-A Complication of Endometrial Ablation/ Resection. J Am Assoc Gynecol Laparosc 1: 4.
- McCausland AM, McCausland VM (2002) Frequency of symptomatic cornual hematometra and postablation tubal sterilization syndrome after total rollerball endometrial ablation: a 10-year follow-up. Am J Obstet Gynecol 186: 1274-80.
- Sharp HT (2012) Endometrial ablation following postoperative complications 207: 242-7.
- Hubert SR, Marcus PS, Rothenberg JM, Schilder JM, Hurd WW (2001) Hematometra after thermal balloon endometrial ablation in a patient with cervical incompetence. J Laparoendosc Adv Surg Tech A 11: 311-3.
- Shatry N, Alexander M, Eskandar O (2021) Chronic pelvic pain due to post-ablation tubal sterilization syndrome: A case report. J Case Rep Images Obstet Gynecol 7: 100093Z08NS2021
- Thomas S, Roy P, Biswas B, Jose R (2012) Complete Cervical Stenosis Following Cesarean Section & VVF Repair. J Obstet Gynaecol India 62: 49-51.
- Curlin HL, Anderson TL (2022) Endometrial Cryoablation for the Treatment of Heavy Menstrual Bleeding: 36-Month Outcomes from the CLARITY Study 14: 1083-1092.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.