Successful Management of A Giant Splenic Cyst. Diagnostic, Surgical and Follow-Up Approach
by Manuel Israel Vela Martinez1*, Rafael Alejandro Espinosa Campos2,5, Alberto Rafael Zarate Rico2, Adriana Itzel Galván Barraza3, Emiliano De La Torre Pacheco4, Valeria Garay Ruiz5
1General Hospital Zone #21 IMSS, San Pedro Coahuila, Mexico
2General Hospital , Torreon Coahuila, Mexico
3General Hospital Zone # 92 IMSS, Acuña Coahuila, Mexico
4General Hospital Zone # 46 IMSS, Gomez Palacio, Durango, Mexico
5Facultad de Medicina Unidad Torreon, Universidad Autonoma de Coahuila
*Corresponding author: Manuel Israel Vela Martinez, General Hospital Zone #21 IMSS, San Pedro Coahuila, Mexico
Received Date: 12 December 2024
Accepted Date: 17 December 2024
Published Date: 19 December 2024
Citation: Vela MMI, Espinoza CRA, Barraza AIG, et al. (2024) Successful Management of A Giant Splenic Cyst. Diagnostic, Surgical and Follow-Up Approach. J Surg 9: 11213 https://doi.org/10.29011/2575-9760.011213
Abstract
We present the clinical case of a giant splenic cyst in a young female patient that was successfully treated surgically. This condition is extremely rare and presents unique challenges regarding its diagnosis and treatment. This case illustrates the role of imaging techniques in the accurate diagnosis and surgical planning, describes the intraoperative findings and surgical procedures [tumor removal and total splenectomy]. The case highlights the need for meticulous adhesiolysis, the prevention of complications and long-term follow-up after splenectomy.
Keywords: Approach; Giant; Imaging techniques; Splenectomy; Splenic cyst; Surgery
Introduction
Giant splenic cysts are rare pathological entities, with a reported incidence of less than 0.07% in autopsy series [1]. Their clinical presentation is often nonspecific, posing significant diagnostic challenges for healthcare professionals [2]. This case report describes the presentation, diagnosis and surgical management of a giant splenic cyst in a young patient, highlighting the complexity of the therapeutic approach and postoperative considerations.
Splenic cysts are generally classified as parasitic and nonparasitic, the latter being subdivided into true (primary) and pseudocysts (secondary) [3]. True cysts represent only 10% of cases and are characterized by the presence of an epithelial lining [4]. The management of these cysts, especially when they reach considerable dimensions, remains a matter of debate, with options ranging from percutaneous aspiration to total splenectomy [5]. The case we present is notable for the exceptional size of the cyst, which occupied a large part of the abdominal cavity and generated symptoms due to mass effect. The complexity of the case was increased by the adhesions to adjacent structures and the associated hematological complications, requiring a multidisciplinary approach [6]. This report aims to contribute to the existing medical literature on the management of giant splenic cysts by emphasizing the importance of accurate diagnosis, meticulous surgical planning, and careful postoperative follow-up. In addition, the long-term implications of splenectomy in young patients and the considerations for the management of potential postoperative complications are discussed [7,8].
Clinical Case
A 22-year-old female patient was admitted to the emergency room on November 8, 2023 due to pain in the left hypochondrium, fever of 39°C, and wet cough. The condition began on September 13 with pain in the right scapular area that radiated to the left hypochondrium. She was initially treated with analgesics and antibiotics without improvement. The initial ultrasound was inconclusive, so an abdominal computed tomography (CT) scan was performed, which revealed a complex cystic lesion dependent on the spleen measuring 240x171x190 mm, with smooth edges and some calcifications. Loss of the usual morphology of the spleen and displacement of adjacent structures were observed, accompanied by left laminar pleural effusion. CA 19-9 levels were 25.5 U/mL. The initial diagnosis was a giant splenic cyst. During the preoperative evaluation, the patient was classified as having ASA III anesthetic risk. Preoperative examinations showed anemia (Hb: 9.6 g/dL) and coagulation disorders (INR: 1.57), so she was given a preoperative transfusion of packed red blood cells and fresh frozen plasma to correct the anemia and coagulation disorders. An exploratory laparotomy was scheduled for November 14, a procedure that lasted approximately 4 hours and revealed the following findings: (1) a giant 40x30 cm splenic cyst with greenish contents, (2) firm adhesions to the tail of the pancreas, stomach, colon, and omentum, (3) an ovarian cyst, and (4) no visible or palpable liver lesions.
The surgical procedure performed included: (1) careful detumorization to separate adhesions, (2) total splenectomy due to the size of the cyst and the involvement of the splenic parenchyma, (3) placement of two biobag-type drains in the tumor bed and in the pelvic cavity, and (4) prophylactic appendectomy. The surgery was classified as R1 (resection with positive microscopic margins). Intraoperative bleeding was significant, reaching 2400 cc, which required intensive hemodynamic management. The patient was admitted to the ICU immediately after surgery. Close monitoring of hemodynamic parameters was performed, and postoperative anemia was managed. Histopathology confirmed giant splenic cysts with a collagenous wall and reactive epithelial lining. Hematopoietic collection and coagulative necrosis were observed in the adjacent parenchyma. The appendix presented acute peritonitis. Hematological controls two weeks after surgery showed persistent anemia (Hb 10.5 g/dL) and reactive thrombocytosis (630,000 platelets/mm³), common after splenectomy. Twenty days after surgery, a follow-up CT scan was performed, which showed the absence of a spleen with free fluid and inflammatory changes in the surgical bed, persistence of pleural effusion, a probable residual cyst in the gastric fundus measuring 33x58 mm, and retroperitoneal lymphadenopathy (up to 17 mm). After this consultation, follow-up was continued, and at 6 months, a new CT scan showed resolution of the inflammatory changes and lymphadenopathy, as well as the absence of a residual cyst. The patient was referred for an appropriate vaccination regimen against encapsulated organisms (Figure 1).
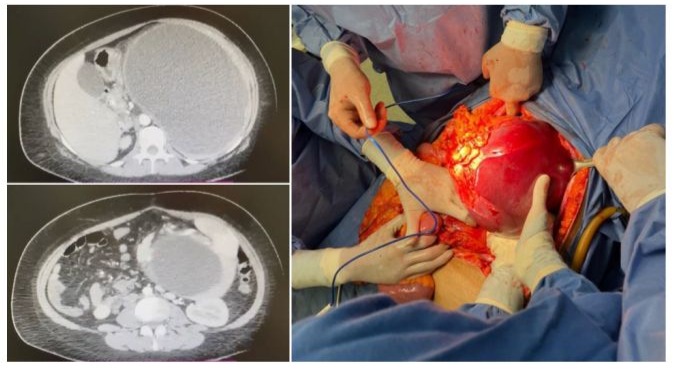
Figure 1: Giant splenic cyst successfully removed.
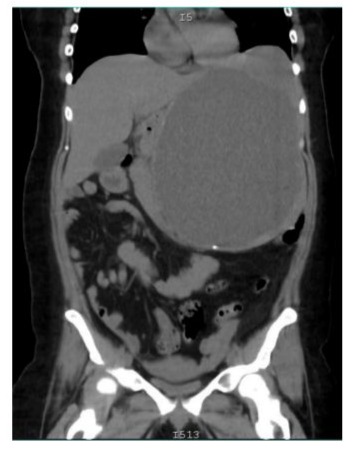
Figure 2: The initial ultrasound was inconclusive, so an abdominal tomography (CT) was performed, which revealed a complex cystic lesion dependent on the spleen measuring 240x171x190 with smooth edges and some calcifications
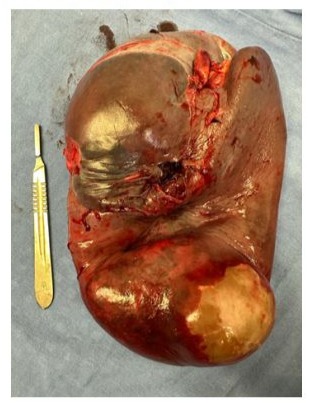
Figure 3: Total splenectomy due to the size of the spleen, the decision to perform a total splenectomy in this case was based on the exceptional size of the cyst (40x30 cm)
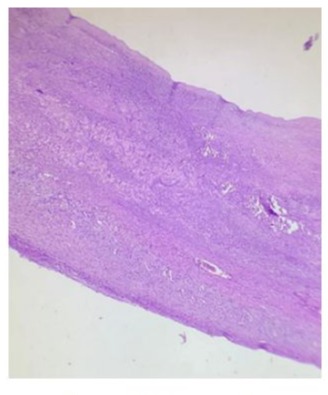
Figure 4: spleen tissue 10 x
Connective tissue wall with collagenized areas as well as sparse remnants of splenic tissue and areas of coagulative necrosis with simple flat epithelium
Pathology images by Dra. Maria Elena Murguia Bañuelos
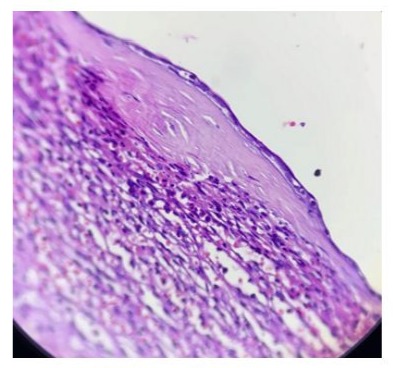
Figure 5: spleen tissue 40x
Connective tissue wall with collagenized areas as well as sparse remnants of splenic tissue and areas of coagulative necrosis with simple flat epithelium Pathology images by Dra. Maria Elena
Murguía Bañuelos

Figure 6: TC Follow up 1 year after surgery. calcified hematoma
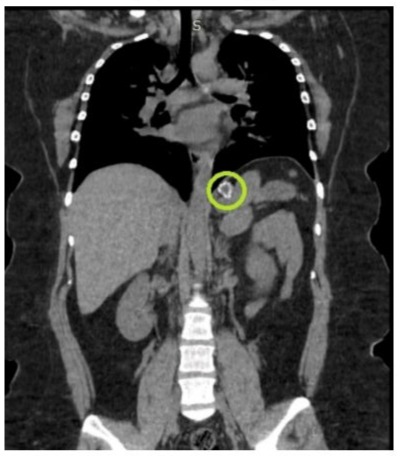
Figure 6: Follow-up CT scan performed 1 year after surgery a remaining calcification is shown.
Discussion
The presented case of a giant splenic cyst in a young patient offers an opportunity to discuss important aspects of the diagnosis, management and follow-up of this rare condition. The clinical presentation of this case, with abdominal pain, fever, and cough, is consistent with the existing literature on giant splenic cysts. According to Ingle et al. (2014), the most common symptoms include left upper quadrant pain, nausea, and vomiting, which are attributed to the mass effect of the cyst [9]. However, the initial presentation with left shoulder pain is an interesting finding that could be attributed to diaphragmatic irritation, a phenomenon described by Farhangi et al. (2016) in cases of large splenic cysts [10]. The use of an ultrasound followed by a CT scan for diagnosis follows the approach recommended by Geraghty et al. (2009) [11]. The CT scan not only confirmed the presence of the cyst, but it also provided crucial information about its size (240x171x190 mm) and anatomical relationships, essential for surgical planning.
The decision to perform a total splenectomy in this case was based on the exceptional size of the cyst (40x30 cm) and its extensive involvement of the splenic parenchyma. Although the current trend favors spleen-sparing procedures, such as laparoscopic fenestration or partial splenectomy [12], the size of the cyst in this case justified a more radical approach. Mertens et al. (2007) reported good long-term results with total splenectomy for nonparasitic splenic cysts, with a recurrence rate of 0%, compared to 25% with conservative procedures [13]. However, it is important to consider the possible long-term complications of splenectomy, especially in young patients. The significant intraoperative bleeding (2400 cc) observed in this case is common in surgeries for giant splenic cysts due to increased vascularity and adhesions. Madhok et al. (2014) emphasize the importance of careful hemostasis and the possibility of requiring blood transfusions in these cases [14]. Postoperative anemia and reactive thrombocytosis observed in hematological controls are expected findings after splenectomy. Di Sabatino et al. (2011) described post-splenectomy thrombocytosis as a common phenomenon that usually resolves within 6-12 months [15]. However, it is crucial to monitor these parameters due to the increased risk of thromboembolic events in the early postoperative period.
The follow-up CT scan performed 20 days after surgery revealed important findings that require follow-up. First, the probable residual cyst in the gastric fundus (33x58 mm) could represent an early recurrence or a separate cyst not initially detected; in this regard, Pang et al. (2019) suggest regular imaging follow-up to detect early recurrences [16]. Second, the observed retroperitoneal lymphadenopathy could be a postoperative inflammatory response or indicate an unrelated underlying pathology; close follow-up and possibly a biopsy are recommended if they persist or increase in size. Third, the left ovarian cyst, although probably incidental, warrants gynecologic follow-up, especially considering the patient’s age. Splenectomy in young patients carries long-term risks that need to be considered. Kristinsson et al. (2014) reported an increased risk of infections, thromboembolic events and certain malignancies in post-splenectomy patients [17]. Therefore, it is crucial to: (a) implement an adequate vaccination regimen against encapsulated organisms (S. pneumoniae, H. influenzae type b, N. meningitidis) [18]; (b) educate the patient about the increased risk of Post-Splenectomy Sepsis (OPSI) and the need to seek immediate medical attention in case of fever or signs of infection [19]; (c) consider long-term antibiotic prophylaxis, especially in the first few years post-splenectomy [20]; (d) regularly monitor hematological parameters and consider prophylactic anticoagulation in high thromboembolic risk situations [21].
Conclusion
This case illustrates the diagnostic and therapeutic challenges associated with giant splenic cysts. Although total splenectomy was necessary due to the exceptional size of the cyst, it is important to consider more conservative approaches when possible. Longterm follow-up is crucial to manage potential complications of splenectomy and detect possible recurrences. This case underscores the importance of a multidisciplinary approach in the management of rare and complex conditions such as giant splenic cysts.
Acknowledgements
To my colleague Alejandro Espinosa for contributing to the surgical growth in the lagoon.
To the Doctors María Elena Murguía Bañuelos and Luis Miguel Vitienez González of Hospital Ángeles Torreón, for the availability and facilities provided for the use of histopathology images.
References
- Lukman K, Sulthana BAAS, Budiman D, Nugraha P (2023) Giant splenic cyst: A case series of rare and challenging cases from the last 22 years. International Journal of Surgery Case Reports 106: 108263.
- Hajjar R, Plasse M, Vandenbroucke -Menu F, Schwenter F, Sebajang H (2020) Giant splenic cyst and solid pseudopapillary tumor of the pancreas managed with distal pancreatectomy and splenectomy. Annals of the Royal College of Surgeons of England 2020: 102.
- Termos S, Othman F, Aljewaied A, Alkhalil AM, Alhunaidi M, et al. (2020) Symptomatic giant primary nonparasitic splenic cyst treated with laparoscopic decapsulation: A case report and literature review. American Journal of Case Reports 21.
- Soo WT, Lau KS, Yong SG, Soon KC (2021) Giant epithelial nonparasitic splenic cyst a pre-operative diagnosis dilemma: A case report. The Medical Journal of Malaysia 76: 597-599.
- Soo WT, Lau KS, Yong SG, Soon KC (2021) Giant epithelial nonparasitic splenic cyst: A pre-operative diagnosis dilemma. The Medical Journal of Malaysia 76: 597-599.
- Hashemzadeh S, Rezabakhsh A, Rahbarghazi R, Amini H (2020) A giant splenic hydatid cyst: Why calcified cysts should not be considered as a dead cyst. Clinical Case Reports 9: 269-273.
- Koirala DP, Yadav M, Shah NA, Yadav D, Neupane S, et al. (2024) Giant isolated splenic hydatid cyst in a pediatric patient: A rare case report. International Journal of Surgery Case Reports 120: 109768
- Abu Sabha MR, Thalji M, Abu Laila K, Alhashlamoun M, Abu Rumaila A, et al. (2024) A giant non-traumatic splenic pseudocyst successfully treated with cyst aspiration and partial cystectomy: A case report and review of literature. Cureus 16.
- Ingle SB, Hinge Ingle CR, Patrike S (2014) Epithelial cysts of the spleen: a minireview. World J Gastroenterol 20: 13899-13903.
- Farhangi B, Farhangi A, Firouzjahi A, Jahed B (2016) Huge epithelial nonparasitic splenic cyst: a case report and a review of treatment methods. Caspian J Intern Med 7: 146-149.
- Geraghty M, Khan IZ, Conlon KC (2009) Large primary splenic cyst: A laparoscopic technique. J Minim Access Surg 5: 14-16.
- Vakili K, Braun A, Fauza DO, Fishman SJ (2009) Spontaneous resolution of a traumatic splenic cyst: case report and review of the literature. J Pediatr Surg 44: e9-e12.
- Mertens J, Penninckx F, DeWever I, Topal B (2007) Long-term outcome after surgical treatment of nonparasitic splenic cysts. Surg Endosc 21: 206-208.
- Madhok R, Kumar N, Bhatnagar A, Rana P, Bhatia A (2014) Giant primary epithelial splenic cyst - a rare encounter. J Clin Diagn Res 8: ND03-ND04.
- Di Sabatino A, Carsetti R, Corazza GR (2011) Post-splenectomy and hyposplenic states. Lancet 378: 86-97.
- Pang P, Yang Z, Zhang H, Gao C, Xu X (2019) Laparoscopic splenectomy for a giant splenic epidermoid cyst in a child: A case report. Medicine (Baltimore) 98: e15443.
- Kristinsson SY, Gridley G, Hoover RN, Check D, Landgren O (2014) Long-term risks after splenectomy among 8,149 cancer-free American veterans: a cohort study with up to 27 years follow-up. Haematology 99: 392-398.
- Bonanni P, Grazzini M, Niccolai G, et al. (2017) Recommended vaccinations for asplenic and hyposplenic adult patients. Hum Vaccine Immunother 13: 359-368.
- Rubin LG, Schaffner W (2014) Clinical practice. Care of the asplenic patient. N Engl J Med 371: 349-356.
- Buzelé R, Barbier L, Sauvanet A, Fantin B (2016) Medical complications following splenectomy. J Visc Surg 153: 277-286.
- Rottenstreich A, Kleinstern G, Specter G, Da’as N, Ziv E, et al. (2018) Thromboembolic Events Following Splenectomy: Risk Factors, Prevention, Management and Outcomes. World J Surg 42: 675-681.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.