Subsidence Analysis of the Metaphyseal Fixed Shorter Cementless CoreHip Stem
by Mohamed Morgan1, Mevluet Sungu2,3, Philipp Schuster1,4, Bernd Fink1,5*
1Department of Joint Replacement, General and Rheumatic Orthopaedics, Orthopaedic Clinic Markgröningen gGmbH, Kurt-LindemannWeg 10, 71706 Markgröningen, Germany
2Ludwig Maximilians University Munich, Musculoskeletal University Center Munich (MUM), Campus Grosshadern, Munich, Germany
3Aesculap AG Research & Development, Am Aesculap-Platz, 78532 Tuttlingen, Germany
4Paracelsus Medical Private University, Clinic Nuremberg, Department of Orthopedics and Traumatology, Nuremberg, Germany
5Orthopaedic Department, University Hospital Hamburg-Eppendorf, Martinistrasse 52, 20246 Hamburg, Germany
*Corresponding author: Prof. Dr. med. Bernd Fink, Department for Joint Replacement, Rheumatoid and General Orthopaedics, Orthopaedic Clinic Markgröningen, Kurt-Lindemann-Weg 10, 71706 Markgröningen, Germany. Email: bernd.fink@rkh-gesundheit.de
Received Date: 28 August 2025
Accepted Date: 09 September 2025
Published Date: 11 September 2025
Citation: Morgan M, Sungu M, Schuster P, Fink B (2025) Subsidence Analysis of the Metaphyseal Fixed Shorter Cementless CoreHip Stem J Surg 10: 11437 https://doi.org/10.29011/2575-9760.011437
Abstract
Background: Stem subsidence is a predictive factor for early aseptic loosening of hip implants. This study aimed to analyze the subsidence of the metaphyseal-anchored shorter CoreHip stem and investigate possible influencing factors.
Methods: A total of 100 patients (61 female, 39 male; mean age 65.4±9.8 years) undergoing primary THA with CoreHip stems (2020–2025) were analyzed. Radiographic migration was assessed with FXA software at 5 days, 3 months, and 24 months postop. Clinical variables (age, BMI, weight, gender) and radiographic parameters (Dorr type, Canal Fill Ratio, Canal Flare Index, stem angulation, stem size) were evaluated.
Results: Mean subsidence was 1.03±1.56 mm at 3 months and 1.39±1.87 mm at 2 years. Subsidence >2 mm occurred in 14% of cases. Higher BMI was significantly associated with greater subsidence, while weight was not. Dorr type A femora were more frequent in the ≤2 mm subsidence group. No radiolucencies >2 mm or aseptic loosening were observed. No intraoperative or postoperative complications occurred. Subsidence did not significantly differ between stem sizes.
Conclusion: The CoreHip stem demonstrated comparable or lower subsidence than other short stems. Higher BMI was linked to increased subsidence, whereas weight was not. The small Dorr C sample size remains a limitation.
Keywords: CoreHip; Prosthetic Stem; Subsidence; Total Hip Replacement
Introduction
Aseptic loosening is the most common cause of failure of Total Hip Arthroplasty (THA) and for cementless THA it is already the case 6 months after implantation [1-3]. Subsidence (distal migration of the femoral stem) has shown to be a good predictive factor for early aseptic loosening of this implant [4-7]. Krismer et al. [6] determined a threshold of 1.5 mm subsidence for cementless and cemented stems within the first two years as a well-established risk factor for early implant failure and Streit et al. [4] rated a limit of 2.7 mm as critical for the cementless CLSstem (ZimmerBiomet, Winterthur, Switzerland). The maximum of subsidence occurs within the first 6 - 12 weeks postoperatively [8-12] as bony ingrowth takes place up to 4 – 12 weeks [13,14]. After 24 months stabilization of subsidence is observed in several studies [11,14,15]. The risk of subsidence of a femoral stem is reported to be between 5 and 61.5 % [17]. Femoral stem design and type as well as anatomical properties play relevant roles for the occurrence of subsidence [8,10,18]. A close proximal fit of the femoral stem in the femoral canal is important for initial torsional stability of the stem [18-20], which improve bony ingrowth of the implant [21-24]. The Canal Fill Ratio (CFR) and Canal Flare Index (CFI) are common parameters to describe the stem anchorage in the femoral canal [8,25].
The CoreHip (Aesculap AG, Tuttlingen, Germany) is a new cementless tapered titanium-stem with metaphyseal anchorage and shorter stem length compared to traditional stems. The CoreHip system is a prosthetic stem system in which each size has three different femoral neck-shaft angles (Varus 122°, Standard 132°, Valgus 142°) (Figure 1). These can all be implanted with one rasp of the corresponding size. The aim of the current study was to analyze the quality of the proximal fixation of this shorter stem using subsidence analysis and to evaluate which factors influence a possible subsidence.
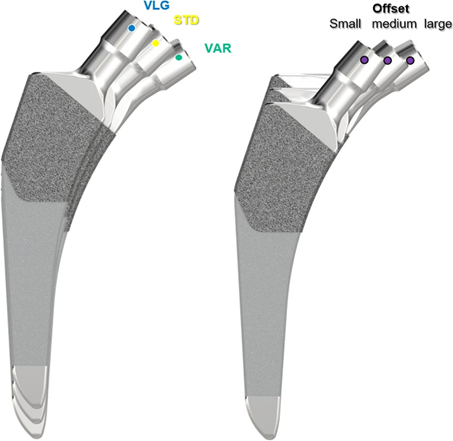
Figure 1: Setting of three different offsets for the same stem size and leg length in the CoreHip-System
Materials and Methods
100 Patients (61 female, 39male) with unilateral CoreHip cementless stems (performed in 2021) were followed prospectively for 2 years. Exclusion criteria were revision cases, infection and bilateral implantations. The age of the patients was 65.4 ± 9.8 years (24 – 84 years) and the BMI 27.3 ± 3.8 (20.5 – 38.5). All surgeries were performed at a single institution by three experienced surgeons using a posterolateral approach. Postoperative full weight-bearing was allowed from day one. Stem size distribution is shown in Table 1.
|
Stem size |
Number of cases (n) |
|
1 |
6 |
|
2 |
6 |
|
3 |
14 |
|
4 |
21 |
|
5 |
23 |
|
6 |
20 |
|
7 |
6 |
|
8 |
3 |
|
9 |
1 |
|
Total |
100 |
Table 1: Distribution of stem sizes
Hip stem migration (subsidence) was evaluated on anteriorposterior radiographs of the pelvic in a standing position with a film-focus-distance of 115 cm performed 5 days, 3 months and two years postoperative. The validated software “FXA” of the independent imaging core lab (RAYLYTIC, Leipzig, Germany) was used [26-28]. The software matches two images (24 months and 3 months vs. 5 days postop) using a normalized 2D grayscale cross-correlation algorithm in an iterative process using the evolutionary optimization algorithm CMA-ES [29]. Moreover, the radiographs were analyzed for radiolucent lines around the stem. The radiographs were analyzed retrospectively. The following parameters were measured on the postoperative radiographs (Figure 2,3): The Canal Flare Index (CFI), the Canal Fill Ratio (CFR), the Stem Angulation (SA) and calculated as potential influencing factors for subsidence as well as the clinical parameters: gender, weight, BMI, age and stem size.
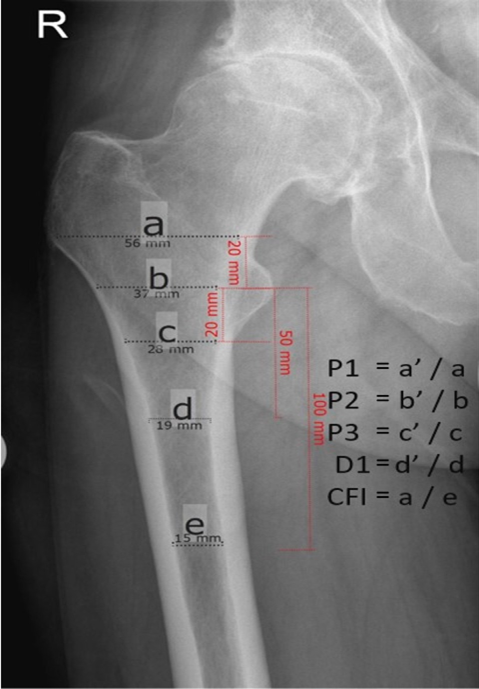
Figure 2a: Description of the different measurements for calculating the Canal Fill Index (CFI) and Canal Fill Ratio (CFR). Fig 2a: preoperative x-ray, Fig 2b: postoperative x-ray. Canal Flare Index (CFI = a/e), Canal-Calcar Ratio (CCR = e/b); Canal Fill Ratios (CFR P1) at 2 cm above the lesser trochanter (P1 = a’/a), CFR P2 at the lesser trochanter (P2 = b’/b), CFR P3 at 2 cm below the lesser trochanter (P3 = c’/c), CFR D1 at 5 cm below the lesser trochanter (D1 = d’/d).
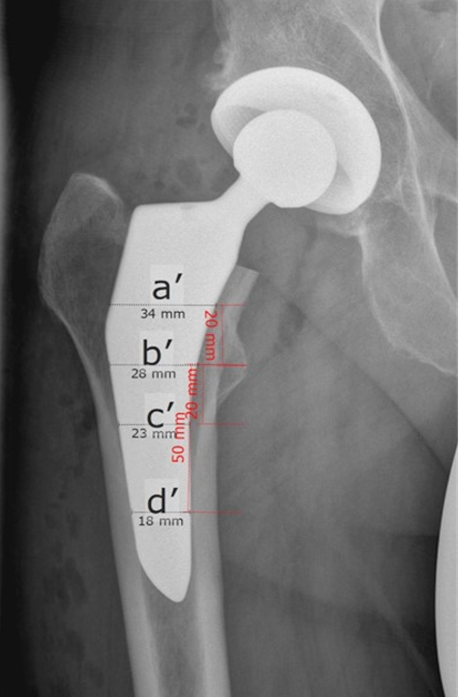
Figure 2b: Description of the different measurements for calculating the Canal Fill Index (CFI) and Canal Fill Ratio (CFR). Fig 2a: preoperative x-ray, Fig 2b: postoperative x-ray. Canal Flare Index (CFI = a/e), Canal-Calcar Ratio (CCR = e/b); Canal Fill Ratios (CFR P1) at 2 cm above the lesser trochanter (P1 = a’/a), CFR P2 at the lesser trochanter (P2 = b’/b), CFR P3 at 2 cm below the lesser trochanter (P3 = c’/c), CFR D1 at 5 cm below the lesser trochanter (D1 = d’/d).
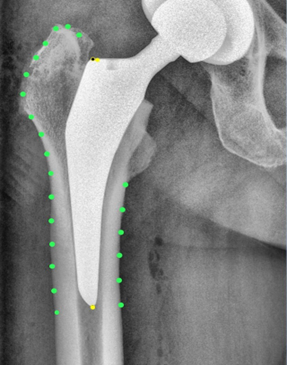
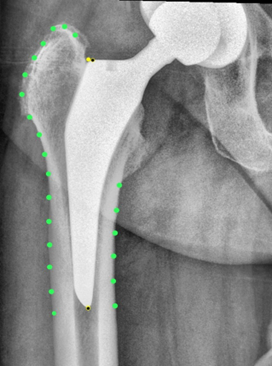
Figure 3b: Case example with FXA software to analyze the subsidence. Fig. 3a: five days postoperative, Fig. 3b: two years postoperative
Statistical analysis:
Statistical analysis was performed using IBM SPSS Statistics for Windows (version 24, IBM Crop., Armonk, NY). For statistical evaluation of categorial variables and group comparisons, Chisquare and Fisher’s exact test were used. For statistical evaluation of parametric data, a Student t-test was used; for nonparametric data, a Mann-Whitney U-test was used. All reported p-values are two-tailed, with an alpha level < 0.05 considered as significant. All values are either given as mean ± standard deviation or median and interquartile range.
Results
The average subsidence was 1.03 ± 1.56 mm at 3 months and 1.39 ± 1.87 mm at 2 years follow-up. In 14 % there was a subsidence of more than 2 mm. Of the possible influencing parameters only BMI and Dorr-type showed a significant difference between stems with less or more than 2 mm subsidence (higher BMI in patients with more than 2 mm subsidence and higher amount of Dorr-type A femurs in the group of femurs with less than 2 mm subsidence) (Table 2,3). All other clinical and radiological parameters showed no difference between the two groups (less and more of 2 mm subsidence) (Table 2,3) We did not observe any early aseptic loosening nor radiolucency of more than 2 mm in the follow-up of this study. No revision was performed in the follow-up.
|
Subsidence ≤ 2mm |
Subsidence > 2mm |
p-value |
Test |
|
|
Side |
||||
|
Left |
34 |
3 |
0.265 |
Fisher’s exact test |
|
Right |
53 |
10 |
||
|
Gender |
||||
|
female |
50 |
11 |
0.61 |
Fisher’s exact test |
|
male |
37 |
2 |
||
|
Dorr-Type |
||||
|
A |
9 |
0 |
< 0.001 |
Chi-square |
|
B |
72 |
7 |
||
|
C |
6 |
6 |
Table 2: Categorical variables
|
Subsidence ≤ 2mm |
Subsidence > 2mm |
p-value |
Test |
|
|
BMI |
27.0 ± 4.0 |
29.2 ± 2.2 |
0.009 |
T-test |
|
Age |
65.4 ± 10.0 |
65.2 ± 9.3 |
0.911 |
T-test |
|
Weight |
79.5 ± 14.1 |
82.2 ± 10.7 |
0.43 |
T-test |
|
Axis [varus: positive, valgus: negaitve] |
0.6° ± 1.0° |
0.3° ± 0.7° |
0.156 |
T-test |
|
CFI |
3.2 ± 0.6 |
3.2 ± 0.9 |
0.92 |
T-test |
|
CFR P1 |
0.71 ± 0.06 |
0.73 ± 0.06 |
0.285 |
Mann-Whitney-U |
|
CFR P2 |
0.78 ± 0.08 |
0.79 ± 0.05 |
0.685 |
Mann-Whitney-U |
|
CFR P3 |
0.80 ± 0.08 |
0.80 ± 0.05 |
0.785 |
Mann-Whitney-U |
|
CFR D1 |
0.80 ± 0.08 |
0.80 ± 0.05 |
0.787 |
T-test |
Table 3: Interval scaled variables
Discussion
Different thresholds of subsidence for prediction of aseptic loosening have been described in the literature [4,6]. Krismer et al. [6] determined a threshold of 1.5 mm subsidence for cementless and cemented stems within the first two years as a well-established risk factor for early implant failure with a sensitivity of 69 % and a specificity of 80 % and Streit et al. [4]. rated a limit of 2.7 mm as critical for the cementless CLS-stem (ZimmerBiomet, Winterthur, Switzerland). Freeman and Plante-Bordeneuve [30] described a threshold subsidence of 1.2 mm per year during the first 2 years for the prediction of aseptic failure with a specificity of 86% and a sensitivity of 78%. Stihlsen et al. [31] found a highly significant correlation of subsidence > 2 mm at 2 years and subsequent aseptic loosening for the proximally fixed cementless Vision 2000 stem (DePuy Orthopaedics Inc., Warsaw, IN, USA). Because of that and because several other studies set the threshold of subsidence at 2 mm [12,32], we calculated the amount of patients with subsidence of more than 2 mm. For other cementless stems with comparable stem lengths similar subsidence were found as in the current study. Freitag et al. [14] reported an average subsidence of 1.1 mm (range: -5mm to 1.5 mm) up to 5 years follow-up for the Fitmore stem (ZimmerBiomet, Winterthur, Switzerland), Schader et al. [33] of 1.6 ± 1.6 mm and Wanner et al. [34] of 1.4 ± 1.4 mm for the same stem after one year follow-up. Hasler et al. [12] observed an average stem subsidence of 1.98 ± 1.2 mm at a minimum follow-up of 5 years for the AMIStem (Medacta International, Switzerland). Dammerer et al. [35] found a mean subsidence of 1.4 mm (range 0.0-12.0 mm) after 2 year-follow-up of the metaphyseal-anchored press-fit stem Accolate II (Stryker, Kalamazoo, MI, USA) and Migliorini et al. [36] a mean subsidence of 2.8 ± 0.7 mm after 14.1 ± 10.8 months for the collarless Corail stem.
14 % of the CoreHip stems in the current study had a subsidence > 2mm at the follow-up of 2 years. In the study of Hasler et al. [12] 48% of the AMIStems had a subsidence of more than 2 mm at the latest follow-up. Gustke [32] observed a subsidence > 2 mm in 34 % of 100 Fitmore stems (ZimmerBiomet, Warsaw, IN, USA) after a mean follow-up of 1.3 years and Dammerer et al. [35] a subsidence of > 1.5 mm in 28.2% and of > 2.7 mm in 14.1 % of 64 Accolate II stems (Stryker, Kalamazoo, MI, USA) after two years follow-up. Radiolucency of more than 2 mm was not seen in the current study. In the study of Hasler et al. [12] 26% of the AMIStems (Medacta Intrnational, Switzerland) had a radiolucency of more than 2 mm at the latest follow-up of 5 years and Schader et al. [33] in 17.5% for the Fitmore Stem (ZimmerBiomet, Wintherthur, Switzerland) at 10 year-follow-up.
One influencing factor for subsidence is the press-fit of the stem [37,38]. However, in the current study the Canal Fill Ration (CFR) and Canal Flare Index (CFI) as parameters for describing the stem anchorage in the femoral canal [8,25] differed not between the stems with and without subsidence of more than 2 mm. Onio et al. [39] found a significant greater subsidence in Dorr type C femurs compared to the other types for the Fitmore stem. This was not seen in our study, maybe because the sample size for Dorr type C femura was limited. However, it was seen, that stems in Dorr type A femurs were more often in the group of subsidence < 2 mm. Additionally we found a significant higher BMI in the group of more than 2 mm subsidence. BMI was identified as an influencing factor for subsidence in the study of Dammerer et al. [35], Stihlsen et al. [31] and Migliorini et al. [40], whereas Schaer et al. [11] and Hasler et al. [12] did not find clinical parameters (weight, BMI, gender, age) influencing subsidence.
This study has some limitations, including the absence of a control group and the retrospective methodology. Therefore, some selection bias cannot be ruled out completely. However, the number of patients is sufficient, similar or even larger as some other cited studies [11,12,32,33,35,39,41,42]. While RSA is considered to be the gold standard for subsidence analysis, EBRA-FCA as well as Realytics offers the advantage of being a non-invasive method with high accuracy that can be used in a retrospective study design [6,41]. Therefore, valid results can be assumed. Another limitation is the follow-up period of 24 months. The maximum of subsidence is reported to occur between 6 and 12 weeks in studies [8-12] and within the first six months in other studies [16,42]. After 24 months stabilization of subsidence is observed in several studies [11,14,15,35]. Moreover, other studies concerning stem subsidence had the same follow-up [9,43,44].
Conclusion
The examined CoreHip stem showed comparable or even lower subsidence to other stems on the market with higher BMI in the patients with subsidence of more than 2 mm and more often Dorr A types in the femora with less than 2 mm subsidence.
Acknowledgments
We thank the radiology team of Orthopaedic Clinic Markgröningen for their support.
Ethical Considerations
This study was approved by the Ethics Committee of the Landesärztekammer Baden-Württemberg (Ref. F-2017-085). All patients provided informed consent. Consent for publication of radiographic images was obtained.
Conflict of Interest
B.F. is a consultant of Aesculap, Tuttlingen, Germany. M.S. is an employee of Aesculap, Tuttlingen, Germany. Other authors declare no conflicts of interest.
Funding
This research was funded by Aesculap, Tuttlingen, Germany.
Authors’ Contributions
BF and MM contributed equally as first authors. BF and MM analyzed and interpreted the data, wrote the article. BF supervised the study. MM was responsible for sample analysis. PS performed statistical analysis. All authors approved the final manuscript.
References
- Johnsen SP, Sorenson HT, Lucht U, Soballe K, Overgaard S, et al. (2006) Patient-related predictors of implant failure after primary total hip replacement in the initial, short- and long-terms. A nationwide Danish follow-up study including 36,984 patients. J Bone Joint Surg Br 88:1303-1308.
- Ulrich SD, Seyler TM, Bennett D, Delanois RE, Saleh KJ, et al. (2008) Total hip arthroplasies: what are the reasons for revision? Int Orthop 32: 597-604.
- Sadoghi P, Liebensteiner M, Agreiter M, Leithner A, Böhler N, et al. (2013) Revision surgery after total joint arthroplasty: a complicationbased analysis using worldwide arthroplasty registers. J Arthroplasty 28:1329-1332.
- Streit MR, Haeussler D, Bruckner T, Protor T, Innmann MM, et al. (2016) Early migration predicts aseptic loosening of cementless femoral stems: a long-term study. Clin Orthop Relat Res 474: 16971706.
- Kroell A, Beaule P, Krismer M, Behensky H, Stoeckl B, et al. (2009) Aseptic stem loosening in primary THA: migration analysis of cemented and cementless fixation. Int Orthop 33:1501-1505.
- Krismer M, Biedermann R, Stöckl B, Fischer M, Bauer R et al. (1999) The prediction of failure of the stem in THR by measurement of early migration using EBRA-FCA. Einzel-Bild-Roentgen-Analyse-femoral component analysis. J Bone Joint Surg Br 81-Br:81: 273-280.
- Van der Voort P, Pijls BG, Nieuwenhuisjse MJ, Jasper J, Fiocco M, et al. (2015) Nelissen RGHH. Early subsidence of shape-closed hip arthroplasty stems is associated with late revision. A systemic review and meta-analysis of 24 RSA studies and 56 survival studies. Acta Orthopaedica 86: 575-585.
- Al-Najjim M, Khattak U, Sim J, Chambers I. (2016) Differences in subsidence rate between alternativ designs of a commonly used uncemented femoral stem. J Orthop 13: 322-326.
- Selvaratnam V, Shetty V, Sahni V. (2015) Subsidence in collarless corail hip replacement. Open Orthop J 9: 194-197.
- Ström H, Nilsson O, Milbrink J, Mallmin H, Larsson S (2007) Early migration pattern of the uncemented CLS stem in total hip arthroplasties. Clin Orthop Relat Res 454: 127-132.
- Schaer MO, Finsterwald M, Holweg I, Dimitriou D, Antoniadis A, et al. (2019) Migration analysis of a metaphyseal-anchored short femoral stem in cementless THA and factors affecting the stem subsidence. BMC Musculoskelet Disord 20: 604.
- Hasler J, Flury A, Dimitriou D, Holweg I, Helmy N, et al. (2021) Midterm subsidence and periprosthetic radiolucency of the AMIStem: a 5-year EBRA-FCA analysis. J Orthop Surg Res 16: 19.
- Alberktsson T, Branemark PI, Hansson HA, Lindström J. (1981) Osseointegrated titanium implants. Requirements for ensuring a longlasting, direct bone-to-implant anchorage in man. Acta Orthop Scand 52: 155-170.
- Freitag T, Fuchs M, Woelfle-Roos JV, Reichel H, Bieger R (2019) Midterm migration analysis of a femoral short-stem prosthesis: a five-year EBRA-FCA study. Hip Int 29: 128-133.
- Acklin YP, Jenni R, Bereiter H, Thalmann C, Stoffel K. (2016) Prospective clinical and radiostereometric analysis of the Fitmore short-stem total hip arthroplasty. Arch Orthop Traum Surg 136: 277284.
- Galante J, Rostoker W, Lueck R, Ray RD (1971) Sintered fiber medatl composites as a basis for attachment of implants to bone. J Bone Joint Surg Am 53-A: 101-114.
- Froimson MI, Garino J, Machenaud A, Vidalain JP. (2007) Minimum 10-year results of tapered, titanium, hydroxylapatite-coated hip stem: an independent review. J Arthroplasty 22: 1-7.
- Campbell D, Mercer G, Nilsson KG, Wells V, Field JR et al. (2011) Eary migration characteristics of a hydroxyapatite-coated femoral stem: an RSA study. Int Orthop 35: 483-488.
- Burke DW, O’Connor DO, Zalenski EB, Jasty M, Harris WH (1991) Micromotion of cemented and uncemented femoral components. J Bone Joint Surg Br 73-Br: 33-37.
- Callaghan JJ, Fulghum CS, Gilsson RR, Stranne SK (1992) The effect of femoral stem geometry on interface motion in uncemented porouscoated total hip prostheses. Comparison of straight-stem and curvedstem designs. J Bone Joint Surg Am 74-A: 839-848.
- Hua J, Walker PS. (1994) Relative motion of hip stems under load. An in vitro study of symmetrical, asymmetrical, and custom asymmetrical designs. J Bone Joint Surg AM 76-A: 95-103.
- Cameron HU, Pilliar RM, MacNab I (1973) The effect of movement on the bonding of prous metal to bone. J Biomed Mater Res 1973;7: 301-311.
- Haddad RJJR, Cook SD, Thomas KA. (1987) Biological fixation of porous-coated implants. J Bone Joint Surg Am 69-A: 1459-1466.
- Pilliar RM, Lee JM, Maniatopoulos C (1986) Observation on the effect of movement on bone ingrowth into porous-surfaced implants. Clin Orthrop Relat Res 208: 108-113.
- Noble PC, Alexander JW, Lindahl LJ, Yew DT, Granberry WM, et al. (1988) The anatomic basis of femoral component design. Clin Orthop relat Res 235: 148-165.
- Brodt S, Jacob B, Nowack D, Zippelius T, Strube P, et al. (2021) An isoelastic monoblock cup retains more acetabular and femoral bone than a modular press-fit cup. A prospective randomized controlled trial. J Bone Joint Surg Am 103-A: 992-999.
- Schulze M, Trautwein F, Vordemvenne T, Raschke M, Heuer F (2011) A method to perform spinal motion analysis from functional X-ray images. J Biomech 44: 1740-1746.
- Hansen N, Ostermeier A (2001) Completely derandomized selfadaptation in evolution strategies. Evol Comput 9: 159-195.
- Busch A, Jäger M, Klegingat S, Baghdadi J, Flörkemeier T, et al. (2020) Vitamin E-blended highly cross-linked polythylene liners in total hip arthroplasty: a randomized, multicenter trial using virtual CADbased wear analysis at 5-year follow-up. Arch Orthop Trauma Surg 140: 1859-1866.
- Freeman MA, Plante-Bordeneuve P (1994) Early migration and late aseptic failure of proximal femoral prostheses. J Bone Joint Surg Br 76-B: 432-438.
- Stihlsen C, Radl R, Keshmiri A, Rehak P, Windhager R (2012) Subsidence of a cementless femoral component influenced by body weight and body mass index. Int Orthop 36: 941-947.
- Gustke K (2012) Short stems for total hip arthroplasty. Initial experience with the Fitmore stem. J Bone Joint Surg Br 94-B(11 Suppl A): 47-51.
- Schader JF, Thalmann C, Maier KS, Schiener T, Stoffel K, et al. (2023) Prospective evaluation of clinical and radiographic 10-year results of Fitmore short-stem total hip arthroplasty. J Orthop Surg Res 18: 893.
- Wanner R, Ransohoff CB, Wyss T, Nötzli H (2024) Ten-year results of the Fitmore hip stem with a focus on varus/valgus alignment and subsidence – a retrospective monocentric analysis. J Clin Med 13: 5570.
- Dammerer D, Blum P, Putzer D, Krappinger D, Liebensteiner MC, et al. (2022) Subsidence of a metaphyseal-anchored press-fit stem after 4-year follow-up: an EBRA-FCA analysis. Archiv Orthop Trauma Surg 142: 2075-2082.
- Migliorini F, Maffulli N, Pilone M, Kämmer D, Hofmann UK, et al. (2024) Subsidence of the Corail stem in total hip arthroplasty: no influence of bony contact. J Orthop Traumatol 25: 53.
- Viceconti M, Brusi G, Pancanti A, Cristofolini L (2006) Primary stability of an anatomical cementless hip stem: a statistical analysis. J Biomech 39: 1169-1179.
- Gabarr S, Herrera A, Ibarz F, Mateo J, Gil-Albarova J, et al. (2016) Comparative analysis of the biomechanical behaviour of two cementless short stems for hip replacement. Linea Anatomic and Minihip. PLoS One 11.
- Onio Y, Hayashi S, Fujishiro T, Kuroda Y, Nakano N, et al. (2024) The medullary cavity morphology of the proximal femur influences the fixation pattern of the rectangular tapered short stem in total hip arthroplasty. Arch Orthop Trauma Surg 144: 3857-3864.
- Migliorini F, Maffulli N, Pilone M, Velaj E, Hofmann UK, et al. (2024) Demographic characteristics influencing the stem subsidence in total hip arthroplasty: an imaging study. Archiv Orthop Trauma Surg 144: 887-894.
- Schmidutz F, Graf T, Mazoochian F, Fottner A, Bauer-Melnyk A, et al. (2012) Migration analysis of a metaphyseal anchored short-stem hip prosthesis. Acta Orthop 83: 360-365.
- Jahnke A, Wiesmar AK, Ulloa CAF, Ahmed GA, Rickert M, et al. (2020) Outcome of short- to medium-term migration analysis of a cementless short stem total hip arthroplasty using EBRA-FCA: a radiological and clinical study. Arch Orthop Trauma Surg 140: 247-253.
- Leiss F, Götz JS, Meyer M, Maderbacher G, Reinhard J, et al. (2022) Differences in femoral component subsidence rate after THA using an uncemented collarless femoral stem: full weight-bearing with an enhanced recovery rehabilitation versus partial weight-bearing. Arch Orthop Traum Surg 142: 673-680.
- Klebingat S, Bien T, Hürtgen J, Grover P, Dreischarf M, et al. (2023) Accurate determination of hip implant wear, cup anteversion and inclination through AI automated 2D-3D registration. J Orthop Res. Sep;41: 1985-1995.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.