Subconjunctival Fat Prolapse In Left Eye–Diagnosed by Ultrasound - Case Report
by Abdelrahman Shehata1*, Benzil Binu1, Mohammed Isham Shiju1, Nazia Akhtar1, Haya Saffarini1, Pankaj Lamba2
1College of Medicine, Gulf Medical University, Ajman, UAE.
2Ophthalmology Department, Thumbay University Hospital, Ajman, UAE.
*Corresponding author: Abdelrahman Shehata, College of Medicine, Gulf Medical University, Ajman, UAE.
Received Date: 31 July 2025
Accepted Date: 13 August 2025
Published Date: 15 August 2025
Citation: Shehata A, Binu B, Shiju MI, Akhtar N, Saffarini H, et al. (2025) Sub-conjunctival Fat Prolapse In Left Eye–Diagnosed by Ultrasound - Case Report. Ophthalmol Res Rep 9: 170. https://doi.org/10.29011/2689-7407.100170
Abstract
This case report details a 35-year-old male patient’s uncommon presentation of subconjunctival fat prolapse, which was identified using ultrasound imaging. The patient had a slowly growing bulge close to the left eye’s lateral canthus when they first arrived. A soft, yellowish, movable lesion behind the conjunctiva was discovered during the clinical examination. A well-defined hyperechoic lesion with interior cystic alterations and peripheral vascularity was confirmed by ultrasound. The results were most consistent with subconjunctival fat prolapse because of its continuity with intraorbital fat and mobility. This syndrome was thought to have been trauma-induced in this younger person because of occupational microtrauma from repeated eye rubbing, even though it is more typical in older men. The case highlights how crucial imaging is in distinguishing subconjunctival fat prolapse from related disorders like dermolipoma.
Objectives: Documenting and analyzing a case of subconjunctival fat prolapse in a reasonably young adult male is the main goal of this case study. The purpose of this case is to illustrate the salient clinical characteristics and sonographic results linked to this uncommon eye ailment. Examining the pathophysiological significance of persistent microtrauma, especially in patients with occupational risk factors, is another objective. This research also highlights the use of ultrasound as a diagnostic tool for ambiguous conjunctival masses and aims to distinguish subconjunctival fat prolapse from other benign orbital lesions such
dermolipomas.
Patient demographic information Age: 35 years
Gender: Male
Ethnicity: Indian Occupation: Works in a chemical factory.
Clinical history
Symptoms: The patient’s main complaint when he first arrived was a steadily growing swelling near his left eye’s lateral canthus. The edema had been apparent for about three weeks prior to the clinical assessment. He reported no discharge, pain, or changes in his vision. A systemic check found no anomalies in other body parts, and there were no concomitant systemic complaints, and no usage of cosmetic lens. The patient denied having had any previous eye surgery or trauma. He did, however, describe scratching his eyes a lot because he was irritated at work, which would have contributed to the lesion’s genesis by causing recurrent small conjuctivital trauma.
Family history and lifestyle factors
No notable family history of systemic or ocular disorders was found. The patient’s lifestyle, which included working in a chemical factory, may have indirectly exacerbated the disease by causing repeated eye rubbing, which weakened the Tenon’s capsule, a crucial structural structure that stops orbital fat prolapse.
Previous treatments
Prior to his appointment, the patient had not been treated for this disease. For this problem, no past ophthalmic exams, topical eye drops, or pharmaceutical use were reported.
Presentation
There were no proptosis, diplopia, or extraocular muscle limitation. Bilateral visual acuity was maintained, and there were no abnormalities in the right eye.
Clinical examination revealed a yellowish tumor near the left eye’s lateral canthus with scattered edges. Under the conjunctiva, the lesion was readily movable and seemed to have a soft consistency. It did not stick to the deeper parts of the eye. On the surface of the lesion, engorged superficial arteries were observed. The inferior and lateral extents of the lesion were difficult to distinguish, but the superior and medial margins were clearly defined. There were no symptoms of inflammation or infection, and the lesion was not painful. Examining the contralateral eye and other ocular components revealed no anomalies.

Figure 1: Sub-conjunctival Fat Prolapse in Left Eye.
The lesion was assessed by ultrasound imaging, which included color Doppler investigations. From the inferior and lateral portions of the left eyeball, a distinct 17 x 21 × 15 mm hyperechoic lesion was seen. The lesion moved in tandem with the eyeball’s movements, suggesting that it was superficial and unattached to deeper orbital structures. Color Doppler imaging revealed peripheral vascularity and internal cystic regions within the lesion. Within the lesion, a 7 × 3 mm calcified region was also found. The diagnosis of subconjunctival fat prolapse was supported by the discovery that the lesion was continuous with intraorbital fat.
Dermolipoma with internal cystic alterations (less likely) and subconjunctival ocular fat prolapse (more likely) were added in the differential diagnosis. To further evaluate the lesion and validate the diagnosis, further orbital MRI evaluation was advised. Nonetheless, subconjunctival fat prolapse was the most likely diagnosis based on the clinical and sonographic characteristics, including mobility, softness, vascular pattern, and anatomical continuity.
B-scan ultrasonography has showed the inferolateral aspect of the left globe, a well-defined hyperechoic lesion of 17 × 21 × 15 mm. It had a calcified component (7 × 3 mm) and internal cystic alterations. Subconjunctival fat prolapse was strongly suggested by the lesion’s mobility with eye movement and its continuity with intraconal fat.
Predominant peripheral vascularity was confirmed by Color Doppler, which is consistent with a benign lesion.
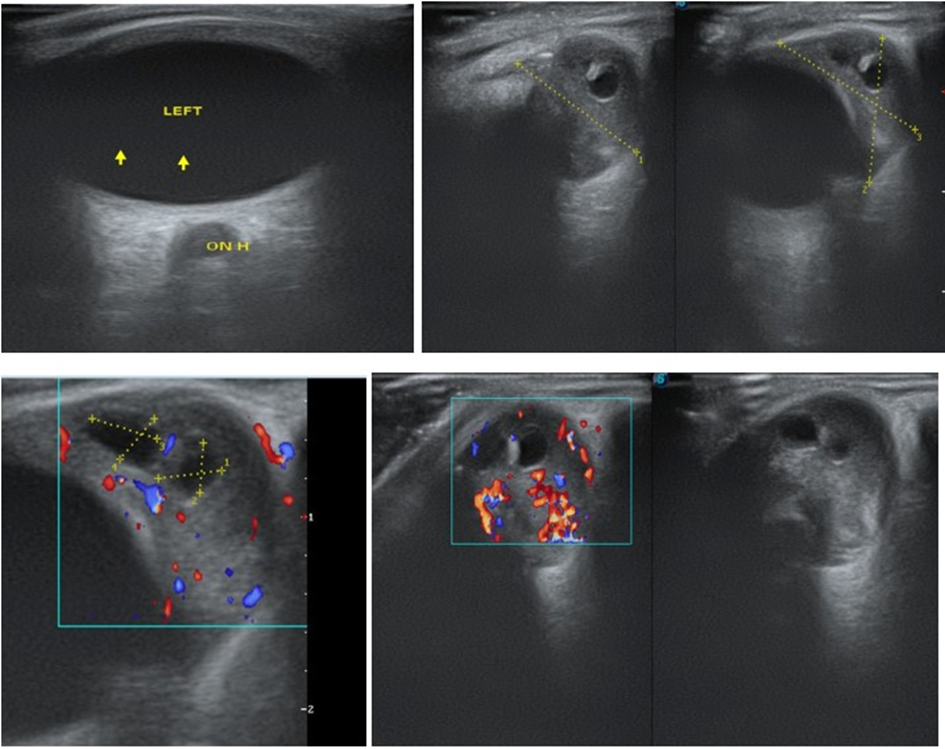
Figure 2: Ultrasound imaging, which included color Doppler investigations.
Because neither the intraocular nor the posterior segment structures were involved, other ophthalmic tests, including OCT, gonioscopy, fluorescein angiography, and visual field testing, were not carried out. A diagnosis of subconjunctival orbital fat prolapse was supported by the imaging results and the clinical presentation; orbital MRI was advised for additional anatomical clarity if necessary.
Diagnostic assessment
The lesion was assessed by ultrasound imaging, which included color Doppler investigations. From the inferior and lateral portions of the left eyeball, a distinct 17 × 21 × 15 mm hyperechoic lesion was seen. The lesion moved in tandem with the eyeball’s movements, suggesting that it was superficial and unattached to deeper orbital structures. Color Doppler imaging revealed peripheral vascularity and internal cystic regions within the lesion. Within the lesion, a 7 × 3 mm calcified region was also found. The diagnosis of subconjunctival fat prolapse was supported by the discovery that the lesion was continuous with intraorbital fat.
Dermolipoma with internal cystic alterations (less likely) and subconjunctival ocular fat prolapse (more likely) were added in the differential diagnosis. To further evaluate the lesion and validate the diagnosis, further orbital MRI evaluation was advised. Nonetheless, subconjunctival fat prolapse was the most likely diagnosis based on the clinical and sonographic characteristics, including mobility, softness, vascular pattern, and anatomical continuity.
Therapeutic intervention
No active medical or surgical treatment had been started at the time of presentation. The lesion was benign and did not result in enough discomfort or vision impairment to need quick treatment. In addition to being informed about the type of lesion, the patient was counseled not to rub his eyes. For additional confirmation, MRI imaging was advised, and routine follow-up was advised to keep an eye out for any problems or developments. In the future, if the lesion becomes bothersome or unattractive, surgical excision might be considered.
Outcomes, prognosis, and follow up
Regular follow-up was recommended to the patient in order to evaluate the size and features of the lesion. The appearance and symptoms of the lesion did not significantly change as of the first follow-up. Subconjunctival fat prolapse typically has a very good prognosis, particularly when the lesion is stable and asymptomatic. It can continue or gradually grow if treatment is not received. When required, surgical excision is a curative procedure with a minimal chance of recurrence. No acute issues or decline in eye health were observed in this instance.
Discussion
A rare but unique clinical syndrome known as subconjunctival fat prolapse is caused by orbital fat herniating through a weaker Tenon’s capsule, usually into the superotemporal or lateral canthal region of the eye. Tenon’s capsule, sometimes referred to as the eyeball’s fascial sheath, is essential for preserving the orbital fat’s anatomical location. This fascial support may deteriorate with time, trauma, surgery, or elevated intraorbital pressure, allowing fat to bulge into the subconjunctival region [1-2].
Because of age-related degradation of connective tissues, the disorder mainly affects older, obese males, who are often in their sixth or seventh decade of life. The patient in this instance, however, was a 35-year-old man who was relatively young and had no past medical or traumatizing history, indicating an unusual presentation. This departure from the norm led to a closer examination of other possible causes. One of the main contributing factors was thought to be the patient’s work environment at a chemical factory, which caused frequent eye rubbing because of irritation from exposure. Tenon’s capsule may have gradually weakened due to chronic mechanical microtrauma from frequent rubbing, which would have allowed the fat prolapse to happen earlier [3].
A soft, yellowish lesion near the lateral canthus that was freely movable, non-adherent to deep tissues, and connected to engorged superficial arteries was the patient’s clinical presentation [4]. These characteristics help distinguish subconjunctival fat prolapse from other conditions like dermolipoma, which is more likely to be congenital, stiffer, less mobile, and frequently contains surface hair follicles [5].
Color Doppler and ultrasound were crucial diagnostic tools. A well-defined hyperechoic lesion with interior cystic alterations and calcification was seen on imaging. Important signs of subconjunctival fat prolapse included the lesion’s continuity with intraorbital fat and its movement with ocular movements. Peripheral vascularity, rather than central vascularity, also supported this diagnosis. The capacity to use high-resolution imaging to noninvasively evaluate the lesion’s consistency, mobility, and anatomical linkages was essential for reducing the number of possible diagnoses [6].
Despite dermolipoma being mentioned in the differential diagnosis, subconjunctival fat prolapse was preferred due to a number of distinctive features. Dermolipomas typically appear earlier in childhood, are congenital, and are more common in females. Usually immobile, they frequently affect the superotemporal quadrant without interacting with the intraconal fat. Together with the sonographic results, these differences lend credence to the diagnosis in this instance [7].
Differentiating between these lesions is crucial in clinical practice since different therapeutic approaches are used. Since subconjunctival fat prolapse is benign and frequently asymptomatic, surgery is only performed when there is considerable enlargement or cosmetic issues. On the other hand, because dermolipomas are close to significant ocular structures and may involve more tissue, they need to be surgically planned more carefully [8].
In order to evaluate conjunctival masses, this case highlights the significance of a comprehensive history, occupational risk assessment, and high-resolution imaging. Additionally, it draws attention to non-traditional risk factors for subconjunctival fat prolapse, which are frequently disregarded, such as microtrauma in younger populations.
Conclusion
The rare case of subconjunctival fat prolapse in a 35-year-old man highlights the fact that, despite being more common in the elderly, this condition can also develop in younger patients with risk factors such chronic microtrauma. The protrusion of orbital fat into the subconjunctival region was probably caused by Tenon’s capsule deteriorating as a result of the patient’s occupational exposure and frequent eye rubbing. The diagnosis was supported by high-resolution ultrasound and color Doppler imaging, which showed a hyperechoic lesion with internal cystic changes and peripheral vascularity, continuous with intraorbital fat. The diagnosis was made based on distinctive clinical features, such as a soft, yellowish, mobile mass at the lateral canthus.
For proper treatment, it was essential to distinguish subconjunctival fat prolapse from disorders that looked similar, like dermolipoma. Since the lesion in this instance was benign and asymptomatic, conservative treatment with frequent monitoring was necessary. In the future, if the lesion becomes symptomatic or cosmetically problematic, surgery is still an option. In addition to highlighting the necessity of taking into account less prevalent etiologies in atypical age groups, this case emphasizes the importance of thorough clinical examination, occupational history, and imaging in the diagnosis of ocular surface lesions.
References
- Rose GE, Wright JE (1992) Subconjunctival orbital fat prolapse: diagnosis and management. Eye 6: 460-464.
- Maruko I, Iida T, Sugano Y, Ojima A, Sekiryu T (2010) Subconjunctival herniation of orbital fat: ultrasonographic and MRI features. Clin Ophthalmol 4: 663-666.
- Shields JA, Shields CL (2011) Orbital fat prolapse and dermolipoma: Differentiation by clinical features. Middle East Afr J Ophthalmol 18: 193-195.
- Rootman J (2003) Diseases of the Orbit: A Multidisciplinary Approach.
- McNab AA (2005) Subconjunctival orbital fat prolapse: a review. Orbit 24: 239-244.
- Kikkawa DO, Lemke BN, Dortzbach RK (1996) Clinical and histologic features of conjunctival dermolipoma. Ophthalmic Plast Reconstr Surg 12: 108-113.
- Yanoff M, Duker JS (2019) Ophthalmology.
- American Academy of Ophthalmology. Basic and Clinical Science Course: Orbit, Eyelids, and Lacrimal System. San Francisco: AAO 2022-2023.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.