Spontaneous Oesophageal Perforation treated with Oesophageal Stent
by Linda Tang*, Francis Lee, Rafael Gaszynski, Sebastionus Kwon, Michael Devadas
Upper Gastrointestinal Surgery Unit, Nepean Hospital, NSW, Australia
*Corresponding author: Linda Tang, Upper Gastrointestinal Surgery Unit, Nepean Hospital, NSW, Australia
Received Date: 13 October, 2024
Accepted Date: 21 October, 2024
Published Date: 23 October, 2024
Citation: Tang L, Lee F, Gaszynski R, Kwon S, Devadas M (2024) Spontaneous Oesophageal Perforation treated with Oesophageal Stent. J Surg 9: 1633. https://doi.org/10.29011/2575-9760.001633
We present the case of a 66-year-old male with Spontaneous Oesophageal Perforation treated with Oesophageal Stenting. This patient reports sudden onset severe anterior chest pain after coughing and haematemesis. He has a background medical history of Type II Diabetes Mellitus, End Stage Renal Failure on Haemodialysis, Hypertension, Obstructive Sleep Apnoea and takes prophylactic Aspirin. Computed Tomography demonstrated pneumomediastinum with contamination (Figure 1). Endoscopic investigation was undertaken. This revealed multiple areas of oesophageal perforation including mucosal tears in the proximal, middle, and distal oesophagus of varying size as well as a haematoma extending the entire length of the oesophagus to the cardio-oesophageal junction (Figure 2). This endoscopy was abandoned due to respiratory compromise secondary to bilateral pneumothoraxes requiring immediate decompression with bilateral chest drains. The patient was not suitable for an oesophagectomy due to their multiple comorbidities and physiological status. The decision was made to use a WallFlex™ Fully Covered Oesophageal Stent (Boston Scientific, Mascot, NSW Australia). This stent was removed three weeks later, and gastroscopy revealed re-epithelialisation of the entire oesophagus along with complete resolution of the perforation at the mid-oesophagus (Figure 3). The patient’s dysphagia continued to improve, and his diet was progressed and discharged home.
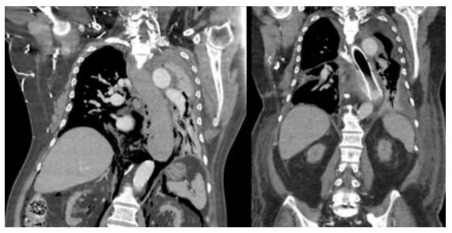
Figure 1: Computed tomography image a) pneumomediastinum consistent with Boerrhave’s b) oesophageal stent in situ with interval improvement of pneumomediastinum.
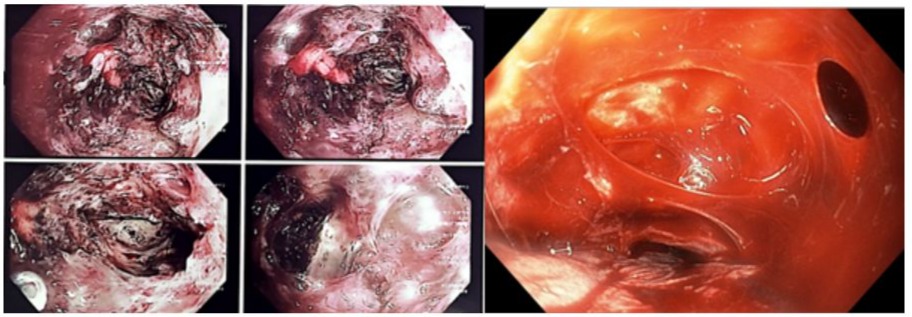
Figure 2: Endoscopic image demonstrating a) extensive oesophageal haematoma and b) multiple full thickness perforations.
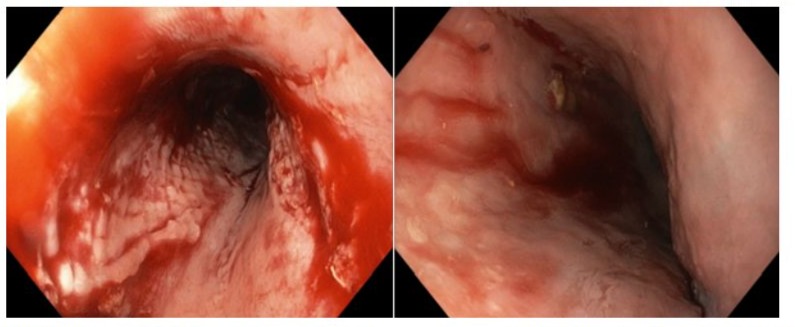
Figure 3: Endoscopic image taken following oesophageal stent removal; complete epithelialisation of oesophagus evident.
Dutch physician Boerhaave first described spontaneous oesophageal perforation in 1724. It is a syndrome which is usually associated with rapid increases in intra-oesophageal pressure with forceful vomiting, defecation, seizures, or coughing as demonstrated in our case [1,2]. Commonly, oesophageal perforations are treated with surgical intervention with high morbidity and mortality. However, advances in endoscopic technology as well as stent technology has given clinicians a greater armamentarium to treat patients especially in the frail end elderly population. Oesophageal stenting is often reserved for palliative measures but can also be utilised for treatment of a variety of pathologies including malignancy, stenoses and fistulas [3]. Advances in oesophageal stent technology include choices such as stent covers, biodegradable stents, removable stents, and, recently, anti-reflux valves [4]. The choice of a fully covered oesophageal stent in our case provided reconstitution of oesophageal lumen and minimisation of mediastinal sepsis. The authors’ intention for dissemination of these images is to provide other surgeons a reference for Boerhaave’s Syndrome that may be amenable to endoscopic treatment with oesophageal stenting.
Endoscopic oesophageal stenting for oesophageal perforations bridges the gap between operative and non-operative management. Complications with oesophageal stents such as fistula formation, stent migration and retrosternal pain are often associated with the length of placement. Therefore, the use of retrievable oesophageal stents, as the authors have used, are paramount to minimising these risks [4]. The patient’s oesophageal stent was removed at three weeks at which point, the oesophageal wall demonstrably was restored. This is in keeping with the literature; re-epithelialisation rates following oesophageal stent for perforations range from 3-7 weeks [5,6].
Nevertheless, it remains clear that oesophageal perforation and its treatment options alike are fraught with considerable risks. The authors believe that oesophageal stent for treatment of spontaneous oesophageal perforation is a valuable treatment option in the appropriate patient.
References
- Jones WG, Ginsberg RJ (1992) Esophageal perforation: a continuing challenge. Ann Thorac Surg 53: 534-543.
- Michel LH, Grillo C, Malt RA (1982) Esophageal perforation. Ann Thorac Surg 33: 203-210.
- Radecke K, Gerken G, Treichel U (2005) Impact of a self-expanding, plastic esophageal stent on various esophageal stenoses, fistulas, and leakages: A single-center experience in 39 patients. Gastrointestinal Endoscopy 61: 812-818.
- Kaltsidis H (2018) Oesophageal stenting: Status quo and future challenges. Br J Radiol 91: 20170935.
- Zhu C, Castrodad A, Santos AP (2021) Alternative management of delayed spontaneous oesophageal perforation by endoscopic stenting. BMJ Case Reports 14.
- Amrani L (2009) From iatrogenic digestive perforation to complete anastomotic disunion: endoscopic stenting as a new concept of “stent-guided regeneration and re-epithelialization”. Gastrointestinal endoscopy 69: 1282-1287.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.