Spontaneous Bilateral Femoral Neck Fractures in an Elderly Male Without Risk Factors: A Case Report
by Mohammed S Alshehri1,3, Adel A Alfozan2, Yazan Almagrabi3, Mohammed A Altorki1, Hashim B Albar1
1King Saud Bin Abdulaziz University for Health Sciences, Saudi Arabia
2Orthopedic Department, King Fahad General Hospital - Ministry of Health, Saudi Arabia
3Orthopedic Department, King Abdulaziz Medical City, Saudi Arabia
*Corresponding author: Mohammed S Alshehri, Orthopedic Department, King Saud Bin Abdulaziz University for Health Sciences, King Abdulaziz Medical City, Ministry of National Guard- Health Affairs, Jeddah, Saudi Arabia.
Received Date: 23 September, 2025
Accepted Date: 13 October, 2025
Published Date: 15 October, 2025
Citation: Alshehri MS, Alfozan AA, Almagrabi Y, Altorki MA, Albar HB (2025) Spontaneous Bilateral Femoral Neck Fractures in an Elderly Male Without Risk Factors: A Case Report. J Orthop Res Ther 10: 1405. https://doi.org/10.29011/2575-8241.001405
Abstract
Introduction: Spontaneous bilateral femoral neck fractures are exceedingly rare and typically linked to high-energy trauma or underlying metabolic bone disorders. This case report presents an uncommon instance of bilateral femoral neck fractures in a 75-year-old male with no prior history of trauma, comorbidities, or recognized risk factors. Case Presentation: A 75-year-old male, previously considered medically well, presented with acute bilateral hip pain and an inability to walk following what appeared to be a spontaneous event during sleep. Imaging revealed bilateral displaced femoral neck fractures (Garden Type IV) with associated osteopenia. The patient underwent successful bilateral hip hemiarthroplasty and was started on romosozumab for severe osteoporosis post-operatively. No perioperative complications were noted, and the patient was discharged in stable condition with a plan for follow-up care. Discussion: This case highlights the insidious nature of osteoporosis in elderly individuals and emphasizes the need for routine screening, even in the absence of apparent risk factors. The rarity of spontaneous bilateral femoral neck fractures underscores the challenge in diagnosing such fractures early, particularly when patients present without significant trauma. Surgical intervention, anabolic therapy with romosozumab, and a comprehensive multidisciplinary approach contributed to the patient’s favorable outcome.
Conclusion: Spontaneous bilateral femoral neck fractures in otherwise healthy elderly individuals are a rare but serious occurrence that requires timely diagnosis and treatment. Routine screening for osteoporosis, early surgical management, and targeted osteoporosis therapy are essential in preventing such fractures and ensuring optimal recovery. This case serves as a valuable reminder of the importance of vigilance in the elderly population and the silent progression of osteoporosis.
Keywords: Femoral Neck Fracture; Osteoporosis; Bilateral Hip; Hemiarthroplasty; Case Report
Introduction
Femoral neck fractures are a common orthopedic emergency in the elderly, often resulting from low-energy trauma in the context of osteoporosis or metabolic bone conditions [1,2]. While unilateral fractures are routinely diagnosed, simultaneous bilateral femoral neck fractures in the absence of trauma are extremely rare and pose diagnostic and therapeutic challenges, especially in patients without prior risk factors or comorbidities [3]. These cases account for less than 0.1% of all hip fractures and are typically linked to high-energy trauma, seizures, or underlying metabolic bone disease [3,6].
Such spontaneous fractures are typically associated with underlying bone fragility due to chronic illnesses, including chronic kidney disease, renal osteodystrophy, or long-term corticosteroid use [4,5]. Nevertheless, cases occurring in otherwise healthy elderly individuals, without evident trauma or systemic disease, are exceptionally uncommon and may be overlooked initially due to their rarity.
Here, we present the case of a 75-year-old male, previously reported as medically well, who developed sudden, spontaneous bilateral Garden type IV femoral neck fractures during sleep, in the absence of trauma, prior hip pathology, or recognized secondary causes. This case highlights the silent yet severe progression of osteoporosis and emphasizes the importance of maintaining a high index of suspicion for spontaneous fractures in elderly patients presenting with acute bilateral hip pain and immobility. We also discuss relevant literature and management considerations in similar cases [1,2,5].
Case Presentation
A 75-year-old male with no known prior comorbidities presented with a sudden inability to walk following severe bilateral hip pain that developed overnight. He denied any recent trauma, falls, or previous history of hip or joint complaints. Notably, two weeks before the onset, he had experienced a brief febrile illness accompanied by generalized weakness, which had resolved following empirical treatment as a presumed viral infection.
Upon arrival, the patient was alert and oriented. Vital signs were stable: blood pressure 118/76 mmHg, heart rate 83 bpm, and oxygen saturation 95% on room air. Physical examination revealed bilateral hip tenderness and a restricted range of motion in both lower extremities, though neurological evaluation was unremarkable.
Initial imaging with a pelvic X-ray revealed bilateral displaced femoral neck fractures (Garden Type IV), with evident osteopenia (Figure 1). Degenerative changes in the knees were also noted. Brain CT ruled out acute intracranial pathology, showing only age-related atrophy. Spinal imaging demonstrated grade 1 L5-S1 retrolisthesis with severe disc narrowing and endplate sclerosis.
Laboratory investigations were significant for leukocytosis (WBC 19.7 ×10³/µL), elevated CRP (11.4 mg/L), and ESR (42 mm/hr). Electrolyte analysis showed hyponatremia (Na⁺ 129 mmol/L) and hyperkalemia (K⁺ 5.4 mmol/L). Hemoglobin was mildly reduced (10.2 g/dL). Although the inflammatory markers were elevated, there was no clinical or microbiological evidence suggestive of any underlying infection, and no source of infection was found.
The patient was evaluated and cleared for surgery by the anesthesia team, with no contraindications noted for proceeding under general anesthesia. The patient underwent bilateral hip hemiarthroplasty on December 26, 2023. For the right hip, under general anesthesia, the patient was positioned in the left lateral decubitus position and secured with a hip positioner. A modified Hardinge approach was utilized. The anterior one-third of the abductor muscle was released from its insertion and reflected anteriorly. The joint capsule was incised, and a standard femoral neck osteotomy was performed. The femoral head was removed, and the medullary canal was prepared using sequential broaching up to size 13. Following canal preparation, a cemented Synergy femoral stem size 13 was implanted. A Pinnacle bipolar head (+5 mm, 47 mm diameter) was used, and the hip was reduced and found stable. The capsule and abductor were repaired, and closure was completed in layers using skin staples. Estimated blood loss was approximately 500 cc, and one unit of blood was transfused intraoperatively. The patient was then repositioned for the left hip procedure. Again, a modified Hardinge approach was utilized with similar surgical steps. The femoral neck osteotomy was performed after releasing the anterior third of the abductor. The medullary canal was prepared and broached to size 13. A femoral stem size 13 was cemented, and a bipolar head (+5 mm, 28 mm diameter) was implanted. Following reduction, the hip was stable. The soft tissue repair and closure were performed in layers with skin staples.
The patient tolerated both procedures well and was extubated postoperatively without complications. He was transferred to the recovery room in stable condition. post-operative radiographs confirmed proper implant positioning (Figure 2). He was managed with pain control, deep vein thrombosis (DVT) prophylaxis, and nutritional optimization, including a potassium-restricted diet. Endocrinology consultation post-operatively revealed severe osteoporosis, and the patient was initiated on romosozumab alongside high-dose vitamin D.
There were no perioperative complications such as infection or hardware failure. The patient was mobilized with a walker and discharged on December 31, 2023, in stable condition. Follow-up appointments were scheduled with both endocrinology and orthopedic services.
|
Test |
Result |
Reference Range |
Flag |
|
WBC |
19.7 ×10³/µL |
4.0–11.0 ×10³/µL |
H |
|
CRP |
11.4 mg/L |
<5.0 mg/L |
H |
|
ESR |
42 mm/hr |
<20 mm/hr |
H |
|
Hemoglobin (Hgb) |
10.2 g/dL |
13.5–17.5 g/dL |
L |
|
Potassium (K⁺) |
5.4 mmol/L |
3.5–5.0 mmol/L |
H |
|
Sodium (Na⁺) |
129 mmol/L |
135–145 mmol/L |
L |
|
Lactate (LAC) |
2.4 mmol/L |
0.5–2.2 mmol/L |
H |
|
eGFR |
52 mL/min/1.73m² |
≥60 mL/min/1.73m² |
L |
|
Troponin I |
10.00 ng/L |
<16 ng/L (normal) |
— |
Table 1: Laboratory values upon admission.
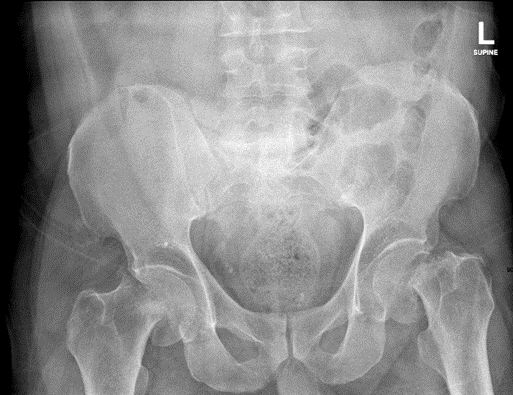
Figure 1: Pelvic X-ray showing bilateral displaced femoral neck fractures.
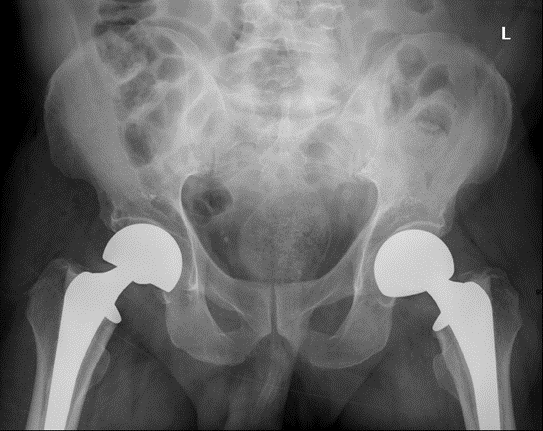
Figure 2: Postoperative X-ray showing bilateral hip hemiarthroplasty with aligned implants.
Discussion
This case of a 75-year-old male with spontaneous bilateral Garden type IV femoral neck fractures underscores the critical interplay between severe osteoporosis and fragility fractures, even in patients perceived as medically healthy. Bilateral femoral neck fractures in the absence of trauma are exceedingly rare, accounting for less than 2% of all hip fractures, and typically occur in patients with profound bone fragility due to systemic conditions such as chronic kidney disease, hyperparathyroidism, or prolonged corticosteroid use [3,4]. However, this patient had no documented comorbidities, highlighting the insidious nature of osteoporosis and its potential to manifest catastrophically without warning.
Pathophysiology and Diagnostic Challenges
The patient’s fractures were attributed to severe osteoporosis, as evidenced by a FRAX score indicating a 3.8% 10-year risk of major osteoporotic fractures. Despite being initially labelled as “medically free,” his advanced age, osteopenia on imaging, and lack of prior bone density assessment (e.g., DXA scan) likely masked an undiagnosed skeletal vulnerability. The absence of trauma and acute presentation during sleep further aligns with the concept of “spontaneous fractures,” where minimal mechanical stress overwhelms osteoporotic bone [1]. Elevated inflammatory markers (WBC 19.7 ×10³/µL, CRP 11.4 mg/L, ESR 42 mm/hr) likely reflected systemic inflammation secondary to fracture-induced tissue damage rather than infection, as post-operative cultures and imaging ruled out septic complications.
Management Considerations
Bilateral hip hemiarthroplasty was prioritized to restore mobility and mitigate risks of prolonged immobilization, such as pneumonia or thromboembolism. The procedure’s success, confirmed by post-operative imaging and uneventful recovery, aligns with literature advocating early surgical intervention for displaced femoral neck fractures in the elderly [2]. Multidisciplinary care, including endocrinology input, was pivotal. Romosozumab, an anabolic agent that stimulates bone formation while inhibiting resorption, was initiated to address severe osteoporosis, reflecting current guidelines that favour anabolic therapy over traditional bisphosphonates in high-risk patients due to its dual mechanism and rapid efficacy [5]. Nutritional optimization, particularly potassium restriction for transient hyperkalemia and vitamin D repletion, further underscores the holistic approach required in such cases.
While the standard approach for femoral neck fractures often involves unilateral surgical repair, particularly in staged fashion for bilateral injuries, our case demonstrates the feasibility and advantages of simultaneous bilateral hip hemiarthroplasty. Several reports suggest that staged procedures may be preferred to minimize perioperative risks such as hemodynamic instability, prolonged anesthesia exposure, or increased blood loss in elderly patients with significant comorbidities [8,9]. For example, Restrepo et al. [10] performed staged bilateral hemiarthroplasties for displaced femoral neck fractures, spacing the procedures to reduce cumulative anesthesia and physiological stress, particularly in more fragile patients. However, in our patient—who was otherwise medically stable—simultaneous bilateral intervention allowed for early mobilization, reduced total anesthesia time, and a shorter overall hospitalization. Performing both procedures during a single anesthetic session may also decrease thromboembolic risk associated with delayed weight-bearing between staged operations.
Notably, our surgical approach also differed from that described by Rednah et al. [13], who managed a similar bilateral presentation in a patient with end-stage renal disease using bilateral total hip arthroplasty (THA) via a posterolateral approach, incorporating cement less stems and acetabular components to address long-term concerns of acetabular erosion in the context of renal osteodystrophy. In contrast, we performed cemented hemiarthroplasty without acetabular replacement, given the patient’s preserved cartilage and absence of systemic conditions such as chronic kidney disease. These differences underscore how implant choice and surgical technique must be tailored to individual patient factors, including systemic health, bone quality, and anticipated joint demands.
Prior studies have reported that, when appropriate patient selection is performed, simultaneous bilateral hip arthroplasty can be carried out safely without significantly increasing perioperative complications, while offering better functional outcomes and lower overall healthcare resource utilization [11,12]. Our successful outcome adds to this evidence, demonstrating that simultaneous bilateral arthroplasty may be safely performed in carefully selected patients, offering both functional and logistical benefits when perioperative risks are adequately managed.
Clinical Implications
This case emphasizes the necessity of routine osteoporosis screening in elderly patients, even those without overt risk factors. The patient’s lack of prior diagnosis highlights a gap in preventive care, as early detection via DXA scans and FRAX assessment could have prompted pre-emptive therapy. Additionally, the brief febrile illness two weeks prior raises questions about whether systemic inflammation or transient immobilization exacerbated bone fragility, though this remains speculative. Pro-inflammatory cytokines such as interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α), which are elevated during acute infections, have been implicated in promoting osteoclast genesis and increasing bone resorption [7]. This transient inflammatory state may have contributed to a tipping point in an already compromised skeletal system.
Limitations and Future Directions
The single-case nature limits generalizability, and the absence of pre-fracture bone density data restricts etiological clarity. Furthermore, while romosozumab’s role is well-supported, long-term outcomes of its use in elderly patients with spontaneous fractures warrant further investigation. Clinically, this case advocates for heightened suspicion of fragility fractures in elderly patients presenting with acute bilateral hip pain, even without trauma. Fall prevention programs, home safety assessments, and patient education on bone health should be integrated into post-discharge care to reduce recurrence.
In conclusion, spontaneous bilateral femoral neck fractures, though rare, serve as a stark reminder of osteoporosis’s silent progression. A multidisciplinary approach combining timely surgery, aggressive osteoporosis management, and preventive strategies is essential to optimize outcomes in this vulnerable population.
Conclusion
This case highlights the rarity of spontaneous bilateral femoral neck fractures in an elderly individual without prior trauma, comorbidities, or secondary causes of bone fragility. It underscores the critical importance of considering osteoporosis as a silent, progressive condition that can result in catastrophic fractures, even in seemingly healthy individuals. Early recognition of fragility fractures and the implementation of preventive measures, such as routine osteoporosis screening and timely pharmacologic intervention, are essential to reduce the risk of such events. In this case, a multidisciplinary approach combining surgical intervention, osteoporosis management with romosozumab, and nutritional optimization contributed to the patient’s successful recovery. The case serves as a reminder that even in the absence of overt risk factors, elderly patients remain vulnerable to severe fractures, necessitating vigilance in both clinical evaluation and preventive care.
Ethics Statement
Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Conflict of Interest
The authors declare no conflicts of interest.
Acknowledgments
The authors thank the surgical and endocrinology teams for their contribution to patient care.
References
- Wick JY (2009) Spontaneous fracture: multiple causes. Consultant Pharmacist 24: 100–102, 105–108, 110–112.
- Wong SK, Chin KY, Suhaimi FH, Ahmad F, Ima-Nirwana S (2016) The relationship between metabolic syndrome and osteoporosis: A review. Nutrients 8: 347.
- Pimentel A, Ureña-Torres P, Zillikens MC, Bover J, Cohen-Solal M (2017) Fractures in patients with CKD: diagnosis, treatment, and prevention: A review by members of the European Calcified Tissue Society and the European Renal Association of Nephrology Dialysis and Transplantation. Kidney International 92: 1343-1355.
- Alem AM, Sherrard DJ, Gillen DL (2000) Increased risk of hip fracture among patients with end-stage renal disease. Kidney International 58: 396-401.
- Nickolas TL, Leonard MB, Shane E (2008) Chronic kidney disease and bone fracture: A growing concern. Kidney International 74: 721-731.
- Lin JT, Wang TC, Tsai CH (2005) Simultaneous bilateral femoral neck fractures in a young adult with epilepsy: A case report and review of the literature. Injury Extra 36(11): 477–480.
- Redlich K, Smolen JS (2012) Inflammatory bone loss: Pathogenesis and therapeutic intervention. Nature Reviews Drug Discovery 11(3): 234-250.
- Parvizi J, Tarity TD, Sheikh E, Sharkey PF, Hozack WJ, et al. (2006) Bilateral total hip arthroplasty: One-stage versus two-stage procedures. Clinical Orthopaedics and Related Research 453: 137–141.
- Demos HA, Rorabeck CH, Bourne RB, MacDonald SJ, McCalden RW (2004) Outcome of staged bilateral total hip arthroplasty: A matched control study. Clinical Orthopaedics and Related Research 418: 139-145.
- Restrepo C, Maltenfort MG, Parvizi J, Rothman RH, Hozack WJ (2013) Hemiarthroplasty for displaced femoral neck fractures: Single-stage bilateral versus staged bilateral procedures. Journal of Arthroplasty 28(1): 94-97.
- Garland A, Jørgensen CC, Gromov K, Kjærsgaard-Andersen P, Kehlet H (2020) Outcomes of simultaneous and staged bilateral hip arthroplasty in a fast-track setting: 4,874 patients from the Danish Hip Arthroplasty Register. Acta Orthopaedica 91(2): 211–217.
- White SM, Rashid TG, Chakladar A, Hunt LP, Eastaugh-Waring SJ (2021) Mortality and morbidity of simultaneous bilateral hip arthroplasty: Systematic review and meta-analysis. Journal of Bone and Joint Surgery. American Volume, 103(9): 782–789.
- Rednah D, Brinji OS, Aldakhil M, Alshareef E, Alshehri M (2023) Surgical Challenge in the Management of Spontaneous, Bilateral, Nontraumatic, Neglected Femoral Neck Fractures in a Patient with End-Stage Renal Disease: A Case Report and Literature Review. Cureus 15(5): e38633.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.