Simplified Shunt for Thoracoabdominal Aortic Repair
by Kim Daenens1*, Toon Kuypers1, Lotte Bruyninckx1, Layth Al Tmimi2
1Department of Vascular Surgery, University Hospitals Leuven, Leuven, Belgium
2Department of Anesthesiology, University Hospitals Leuven, Leuven, Belgium
*Corresponding author: Kim Daenens, Department of Vascular Surgery, University Hospitals Leuven, Herestraat 49, 3000 Leuven, Belgium
Received Date: 20 February 2025
Accepted Date: 24 February 2025
Published Date: 27 February 2025
Citation: Daenens K, Kuypers T, Bruyninckx L, Al Tmimi L (2025) Simplified Shunt for Thoracoabdominal Aortic Repair. Ann Case Report. 10: 2198. https://doi.org/10.29011/2574-7754.102198
Abstract
Introduction: Open repair of the thoracoabdominal aorta (TAA) remains a challenging intervention due to the possible issues with the supra-celiac aortic cross-clamping. To preserve visceral and renal perfusion during clamping, passive arterial shunts or pumps with extra-corporal shunts can be used. Nevertheless, it remains a major procedure in which complications are not inconceivable, and patient’s recovery is highly demanding. To reduce this impact, we introduced a simplified passive arterial shunt (SPAS).
Cases: Debranching was performed with a bypass from the distal descending aorta to the distal infrarenal aorta and a side-branch to connect an octopus-cannula. Visceral and renal perfusion was obtained through four Pruitt catheters. After reconstruction of the aorta, this shunt can be used as a bypass or easily broken down. This technique was used in three different indications: coral reef sub-occlusion, elective aneurysm, and ruptured mycotic aneurysm.
Results: Despite the important comorbidities within the three patients, operations went well without hemodynamic instability. They all experienced quick recovery, only requiring a short stay in the intensive care unit.
Conclusions: This simplified passive arterial shunt minimizes the negative impact of aortic cross-clamping. Therefore, it can be a better alternative to the extra-corporal shunt in selected cases of open repair of the thoracoabdominal aorta.
Keywords: Aortic Clamping; Visceral Perfusion; reperfusion can result in metabolic disturbances, coagulopathy, Thoracoabdominal Aorta. systemic inflammatory reaction, and, with further deterioration, multiple organ failure [1].
Introduction
Open repair of the thoracoabdominal aorta remains a challenging operation. One reason could be the lower exposure to this kind of surgery. It is certainly less common than infrarenal aortic repair, and the experience is decreasing due to the introduction of endovascular solutions (F-BEVAR). A more important reason is the supra-celiac aortic cross-clamping. Proximal to the clamp, we can have cardiopulmonary and cerebral dysfunction due to hemodynamic instability. Distally, we can have hypoperfusion of the spinal cord, viscera, kidneys, and legs. Ischemia and reperfusion can result in metabolic disturbances, coagulopathy, systemic inflammatory reaction, and, with further deterioration, multiple organ failure [1].
In order to reduce the negative impact of this aortic cross-clamping, passive arterial shunts were introduced [2]. Nowadays, they are replaced mainly by a pump for an extra-corporal shunt to the legs and selective perfusion of the visceral and renal arteries [3] (Figure 1a). Such a pump, like the Bio-Medicus pump, has the advantage of having continuous control of the distal inflow through the selective catheters. This makes it possible to react promptly in order to restore flow in one of the catheters or to control blood pressure. However, there are also disadvantages. A minor one is that you need a perfusionist to operate the pump and good communication between the perfusionist, anesthesiologist, and surgeon to maintain a perfect balance in the arterial blood pressure proximal and distal to the clamp. A technical issue is that closing the 22 French holes of the cannulation sites can be difficult due to the bad quality of the aortic wall. A total tube length of at least 500 cm (Figure 2a) can potentially cause problems concerning hemolysate most important disadvantage seems to be the laminar flow from the pump. This is not a physiological pulsatile flow, and therefore, despite perfusion, tissue damage can occur, leading to renal dysfunction, a rise of lactate, and an increasing inflammatory reaction.
Consequently, despite using a pump, we still can have major complications. These complications can be too much for some patients with already serious comorbidities. Therefore, we were looking for a better distal perfusion during aortic cross-clamping.
Cases
The first patient developed a sub-occlusive coral reef stenosis in the thoracoabdominal aorta (Figure 3). Symptoms were invalidating claudication, deteriorating renal function, renovascular hypertension and increasing pulmonary edema with severe oxygen-dependent dispended to generalized edema, she gained 15 kg of weight. An aortic repair was necessary. However, she was rejected for surgery in two university hospitals in France. The operative risk was considered too high, and palliative support was prescribed in order to die at home. Her daughter lives in Belgium and asked for a second opinion. A simplified passive arterial shunt was proposed to minimize acute intraoperative hemodynamic changes and ensure adequate and stable anesthesia management. Its benefit was discussed in advance with the anesthesiologist in charge (Figure 1b).
The operation was performed through left lumbotomy for a retroperitoneal approach with a split of the diaphragm pillars to access the aorta from the distal descending aorta to the aortic bifurcation. A Maquet Intergard 8 mm Dacron graft from the descending aorta to the aortic bifurcation was attached with a side branch for the octopus’ cannula and four Pruitt catheters. Heparin (40 U/kg) was administered, and the aorta was clamped distally from this graft. After the aortotomy, we canalized the visceral and renal arteries to provide pulsatile flow through a total tube length of only 66 cm (Figure 2b). Endarterectomy was performed, and the aorta was repaired with a primary suture. After the removal of all catheters, aortic circulation was restored. Since the distal aorta was relatively small, we maintained the assisting bypass without the side branch to avoid a more extended operation with an additional Dacron interposition. Blood pressure was easy to control during the operation, with minimal blood loss and pulsatile flow in the visceral arteries and legs. Recovery was straightforward, with discharge from the intensive care unit after two days. At the ward, she improved quickly with no more dyspnea and feeling well for the first time in years. She went to a revalidation center and after one week, she returned to France. Six weeks later, during control consultation, she was delighted to feel well and to walk again.
We used the same technique with two other patients (Table 1). The second patient was referred with a thoracoabdominal aneurysm extending to the iliac arteries with a maximal diameter of 60 mm (Figure 4). Endovascular repair was not feasible due to the small diameters and kinking of the iliac arteries. We performed an aortobi-iliac bypass (Terumo Gelweave 20 mm + Gelsoft 18x9 mm) with reimplantation of an aortic cuff with the ostia of the celiac trunk (CT), superior mesenteric artery (SMA) and right renal artery (RRA) and separate reimplantation of the left renal artery (LRA). The operation went well, and the patient experienced the same quick recovery despite his pneumonia. The third patient was referred with pain, gastritis, and dysphagia due to a ruptured mycotic aneurysm at the origin of the celiac trunk (Figure 5 and Figure 6). Again, endovascular repair was not desirable. We resected the diseased aortic wall and closed it with a Dacron patch (from a Gelweave 20 mm). He received intravenous wide-spectrum antibiotics for a fortnight. Since the evidence of a Streptococcus agalactiae surinfection, he was discharged with amoxicillin (1g, four times a day) for another four weeks. Both patients were doing well during the consultation after six weeks.
|
Patient |
#1 |
#2 |
#3 |
|
|
Disease |
coral reef stenosis |
elective aneurysm |
ruptured mycotic aneurysm |
|
|
Age (years) |
79 |
63 |
67 |
|
|
Weight (kg) |
75 |
113.5 |
88 |
|
|
BMI |
30.0 |
39.3 |
26.8 |
|
|
Comorbidities |
Nicotine abuse Hyperlipidemia COPD Gold 2 |
Nicotine abuse Hyperlipidemia COPD Gold 3 CABG in March 2024 |
Nicotine abuse Hyperlipidemia Diabetes type 2 CAD |
|
|
LV EF (%) |
51 |
55 |
65 |
|
|
ASA Score |
4 |
3 |
4 |
|
|
Duration of operation (h:mm) |
4:37 |
6:39 |
3:56 |
|
|
Blood Loss (ml) |
2200 |
2300 |
1400 |
|
|
Transfusions (ml) |
||||
|
- Cell saver |
656 |
970 |
350 |
|
|
- Packed cells |
496 |
0 |
0 |
|
|
- Plasma |
577 |
486 |
219 |
|
|
Hemoglobin (g/dL) |
||||
|
- Preoperative |
10.3 |
14.9 |
15.0 |
|
|
- Peroperative |
9.2 |
11.5 |
13.4 |
|
|
- Postoperative D1 |
8.9 |
12.5 |
14.4 |
|
|
- Reference |
(12-16) |
(14-18) |
(14-18) |
|
|
Lactate (mmol/L) |
||||
|
- Preoperative |
0.4 |
1.5 |
1.5 |
|
|
- Peroperative peak |
1.2 |
3.8 |
3.1 |
|
|
- Postoperative D1 |
0.4 |
1.3 |
0.8 |
|
|
- Reference |
(0.5-2.2) |
(0.5-2.2) |
(0.5-2.2) |
|
|
Creatinine (mg/dL) |
||||
|
- Preoperative |
1.32 |
1.02 |
0.85 |
|
|
- Postoperative D1 |
0.81 |
2.02 |
1.08 |
|
|
- At discharge |
0.69 |
1.23 |
0.65 |
|
|
- Reference |
(0.5-0.95) |
(0.7-1.17) |
(0.7-1.17) |
|
|
eGFR (ml/min) |
||||
|
- Preoperative |
45 |
78 |
90 |
|
|
- Postoperative D1 |
69 |
34 |
77 |
|
|
- At discharge |
83 |
66 |
101 |
|
|
- Reference |
(≥90) |
(≥90) |
(≥90) |
|
|
Length of Stay (days) |
||||
|
- Intensice Care Unit |
2 |
4 |
3 |
|
|
- Hospital |
10 |
13 |
13 |
|
BMI: Body Mass Index, COPD: Chronic Obstructive Pulmonary Disease, CABG: Coronary Artery Bypass Grafting, CAD: Coronary Artery
Disease, LV EF: Left Ventricular Ejection Fraction, ASA Score: American Society of Anesthesiologists Physical Status Classification, D1: day 1, eGFR: Estimated Glomerular Filtration Rate
Table 1: Perioperative Characteristics of the Three Patients.
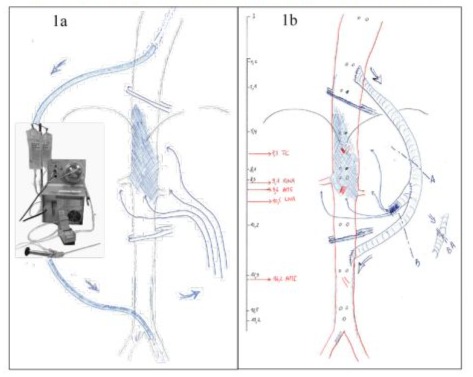
Figure 1: a: Traditional extracorporeal shunt utilizing a Bio-Medicus pump. 1b: Schematic representation of the proposed shunt based on a preoperative CT reconstruction.
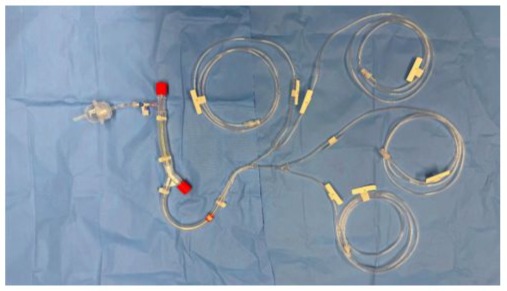
Figure 2a: Eurosets vascular octopus set, made for an extra-corporal shunt with Bio-Medicus pump.
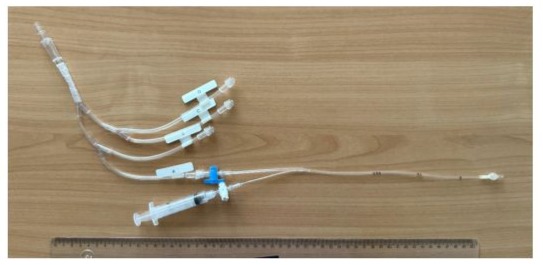
Figure 2b: A shortened version of the Simplified Passive Arterial Shunt with one Pruitt catheter connected.
Figure 3: Case #1: coral reef aorta; sub-occlusive at the thoracoabdominal level (CT-scan).
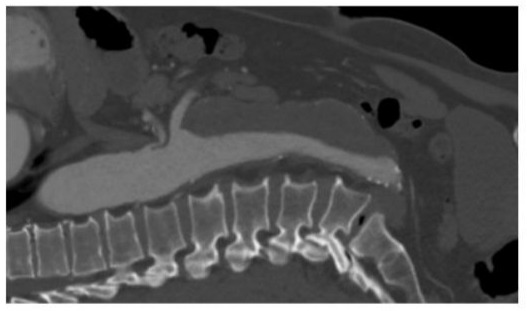
Figure 4: Case #2: thoracoabdominal aorta aneurysm of 60mm diameter (CT-scan).
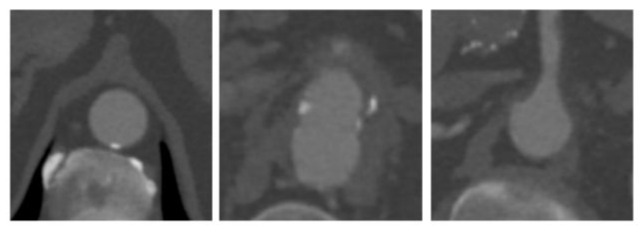
Figure 5: Case #3: ruptured mycotic aneurysm: supra-celiac, celiac trunk, superior mesenteric artery (CT-scan).

Figure 6: Case #3: the hole in the aorta, the dacron graft, and three Pruitt catheters already in place.
Discussion
In order to reduce the severity of open thoracoabdominal aortic repair and to improve surgical results, a lot of adjunctive techniques were developed [3,4]: selective digestive decontamination, avoidance of nephrotoxic drugs, systemic hypothermia, left heart bypass with extra-corporal pump providing selective visceral and renal perfusion or cold crystalloid renal perfusion, reattachment of intercostal arteries guided by motor-evoked potentials, drainage of cerebrospinal fluid, sequential aortic clamping, and avoidance of hemodynamic instability. This article focuses on the perfusion distal to the supra-celiac aortic cross-clamping. This is most frequently obtained by an extra-corporal shunt with a centrifugal pump [3]. Before this mechanical circulatory support was introduced, there were other solutions to achieve distal aortic perfusion.
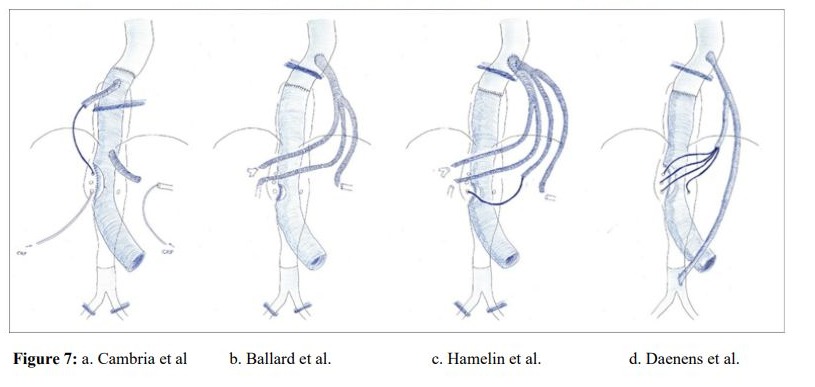
The passive arterial shunt was already described by Cambria et al. [2] in 1998.Visceral perfusion through the CT or SMA was obtained through a 16 to 22 Fr perfusion catheter, connected to a 10mm Dacron side-branch of the aortic graft after completion of the proximal anastomosis (Figure 7a). Using this shunt reduced the duration of visceral ischemia by an average of 31.3 minutes. There was no evidence of coagulopathic bleeding in their 15 patients. However, compared with the group without a shunt, they had a similar need for transfusion, more complications, and still a postoperative hospital stay of 15.1 days. There were also indications that visceral perfusion was not normalized with shunt, which they attributed to the limitations of catheter diameter and length. Perhaps other factors can play a role in their results. Their technique provides visceral perfusion only 25 minutes after aortic cross-clamping. Only one of the visceral arteries is perfused. They defend the single vessel perfusion by observing pulsatile arterial back-bleeding in the second visceral artery after perfusion of the first visceral artery.
On the other hand, this can explain why visceral perfusion was not normalized with their shunt. Renal arteries received only cold perfusion and no pulsatile arterial perfusion. During aortic cross-clamping, there is no perfusion to the legs. Without systemic heparin, there could be a risk of thrombosis in more diseased peripheral arteries. Division of the diaphragm is required to have optimal access; however, if it can be avoided, it could help reduce pulmonary complications.
In order to reduce ischemia time to the abdominal viscera, Ballard [5] started with a trifurcated graft proximal to the following aortic anastomosis (Figure 7b). Before opening the aneurysm and performing the proximal aortic anastomosis, sequential end-to-end bypasses to the LRA, SMA, and CT helped to reduce ischemia time: 11 minutes for each bypass and 34 minutes for the RRA. The average blood loss was 4100ml. Although they used this technique in eight selected patients, they favour a multi-adjunct approach with cerebrospinal fluid drainage, distal aortic and visceral perfusion using a Bio-Medicus pump, and selective intercostal artery reimplantation.
Possible disadvantages of their technique are that there is still an ischemia time of 34 minutes for the RRA and no perfusion of the lower extremities during aortic cross-clamping. The extraanatomical bypasses are also prone to kinking after restoring the retroperitoneum to its anatomical position. There is also more prosthetic material, potentially increasing the risk of graft infection.
Hamelin et al. [6] combines, to some extent, Ballard’s debranching strategy with Cambria’s passive shunt. They adapt the advantage of the proximal debranching to overcome the 25 minutes of nonperfusion. However, they have a more flexible application of a multi-branch graft. Like Ballard, they start with a bypass to the LRA. Depending on the situation, the CT, SMA, or RRA can also be anastomosed to the branched graft. From one branch, a cannula with one or more shunts can provide temporary pulsatile arterial flow if no bypass is required (Figure 7c). With their technique, they had a mean visceral ischemic time of 17 minutes. They state that complete left phrenectomy seems to be well-tolerated, also in patients with chronic obstructive pulmonary disease. They emphasize the advantage of the physiological pulsatile flow, providing final results better than found in recent literature. Since F-BEVAR is not significantly better in perioperative mortality than open repair but has higher follow-up mortality and a higher rate of interventions, they suggest comparing their technique with endovascular repair. Requiring at least six anastomoses is undoubtedly time-consuming, and with those extra-anatomical bypasses, there is still the risk of graft-kinking. Indeed, there were four patients out of 40 seen with kinking and requiring reintervention, attributed to a learning curve.
Monnot et al. [7] constructed a shunt from the axillary artery to connect a cannula for visceral perfusion. They used this technique in 10 cases where an extra-corporal shunt was undesirable due to severe iliac artery occlusive disease. Luparelli et al. [8] constructed a shunt from the axillary artery through a reversed bifurcated graft on the distal infrarenal aorta. The cannula for visceral perfusion was connected to the other branch of that bifurcated graft. The renal arteries received cold perfusion. Nesi et al. [9] used an already existing axillofemoral graft as a source of their visceral shunt during an emergency repair, proving that the inspiration of the moment is still important. Indeed, the left axillary artery can be an alternative in selected cases. However, you may have to consider that an extra operation field is necessary, that the extracorporal position of the graft is more prone to infection during long operations, and that flow can be restricted due to the smaller axillary artery and more extended graft.
Hostalrich et al. [10] presented their series of 38 patients with coral reef atherosclerosis of the visceral aorta for 15 years. Distal aorta or visceral perfusion was not provided, resulting in a mean visceral ischemic time of 28 minutes. Nevertheless, the results were quite good, with an “acceptable rate of postoperative complications. “Cases are complex to compare, and we performed these repairs without shunting. However, since our first patient was rejected for operation in two university hospitals, we were convinced that we had to provide distal pulsatile arterial flow to limit the impact of the operation. Our technique reduced the visceral ischemic time to two times two minutes, the time required for placing and removing the selective catheters.
Conclusion
In the search to minimize the impact of supra-celiac aortic crossclamping, it is not surprising that several people independently find similar solutions. Nowadays, there are a lot of protective techniques available that you can use depending on the complexity of the cases. In addition, to strive for the patient’s condition to be as stable as possible, we try to preserve the diaphragm, maintain insufflation of both lungs, and provide arterial pulsatile flow in the visceral, renal, and leg circulation. Our simplified passive arterial shunt helped minimize ischemic time and seems an important part of all the measures to carry out the operation in the most favourable conditions.
Acknowledgments: Acknowledgment to Dr Gerrit Koppert and Dr Sabrina Houthoofd for presenting the second and third patient.
Ethical Considerations: Approval for this study was obtained by The Ethics Committee Research (S70208) and informed consent was obtained by the three patients.
Conflict of Interests: There are no conflicts of interests concerning all the four authors.
References
- Gertler JP, Cambria RP, Laposata M, Abbott WM. (1996) Coagulation changes during thoracoabdominal aneurysm repair. J Vasc Surg. 24:936-45.
- Cambria RP, Davison JK, Giglia JS, Gertler JP. (1998) Mesenteric shunting decreases visceral ischemia during thoracoabdominal aneurysm repair. J Vasc Surg. 27:745-749.
- Waked K, Schepens M. (2018) State-of the-art review on the renal and visceral protection during open thoracoabdominal aortic aneurysm repair. J Vis Surg. 4:31.
- Tanaka A, Estrera AL, Safi HJ. (2021) Open thoracoabdominal aortic aneurysm surgery technique: how we do it. J CardioVasc Surg. 62:295-301.
- Ballard JL. (1999) Thoracoabdominal aortic aneurysm repair with sequential visceral perfusion: a technical note.Ann Vasc Surg. 13:216221.
- Hamelin T, Bouziane Z, Settembre N, Malikov S. (2024) Elective open repair with the debranch, perfuse, reconstruct technique to treat suprarenal or type IV thoracoabdominal aortic aneurysms. J Vasc Surg. 80:1669-75.
- Monnot A, Dusseaux MM, Godier S, Plissonnier D. (2016) Passive temporary visceral shunt from the axillar artery as an adjunct method during the open treatment of thoracoabdominal aortic aneurysm. Ann Vasc Surg. 36:127-131.
- Luparelli A, Minucci M, Donato F, Tinelli G, Donati T, et al (2024) Passive temporary arterial shunt for visceral and distal aortic perfusion during complex aortic surgery. J Vasc Surg Cases Innov Tech. 10:101592.
- Nesi F, Pogany G, Bartolucci R, Leo E, Rabitti G. (2004) Emergency Repair of Type IV Thoracoabdominal Aneurysm with the Use of a Singular Shunt to Maintain Visceral Perfusion. Eur J Vasc Endovasc Surg. 27:445-446.
- Hostalrich A, Hurtado R, Boisroux T, Garmy-Susini B, Ricco JB, et al (2024) Modern Open Surgery for Coral Reef Aorta with Viscerla Artery Involvement. Eur J Vasc Endovasc Surg. S1078-5884(24)01319-4.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.