Shifting Paradigms in Andrology: National Trends in Penile Prosthesis and Artificial Urinary Sphincter Use Among Older Australian Men
by Nicholas Gillman*, Craig Neilson, Jason Kim, Neil Smith
Department of Urology, Gold Coast University Hospital, 1 Hospital Boulevard, Southport, Queensland, 4215, Australia
*Corresponding Author: Nicholas Gillman, Department of Urology, Gold Coast University Hospital, 1 Hospital Boulevard, Southport, Queensland, 4215, Australia
Received Date: 04 February 2026
Accepted Date: 09 February 2026
Published Date: 11 February 2026
Citation: Gillman N, Neilson C, Kim J,Smith N (2026) Shifting Paradigms in Andrology: National Trends in Penile Prosthesis and Artificial Urinary Sphincter Use Among Older Australian Men. J Surg 11: 11564 https://doi.org/10.29011/2575-9760.011564
Abstract
Background: Erectile Dysfunction (ED) and Stress Urinary Incontinence (SUI) are prevalent conditions in older men and substantially impact quality of life. Penile Prosthesis (PP) implantation and Artificial Urinary Sphincter (AUS) surgery represent definitive surgical management for refractory disease, yet utilisation of these interventions in older populations has historically been limited. The study examines long-term national trends in andrological implant surgery in Australian men aged 75 years and older.
Methods: A retrospective, population based observational study using Australian Medicare Benefits Schedule (MBS) claims data from 1994-2024 was performed. Age stratified, population-adjusted utilisation of AUS and PP procedures was analysed. Primary outcomes included annual procedure volumes and standardisation rates in men aged ≥75 years. Secondary outcomes included the proportion of national implant activity attributable to this age group and comparative temporal trends between AUS and PP.
Results: Between 1994 and 2024, 7,474 AUS and 12,881 PP procedures were recorded nationally. Men aged ≥75 years comprised approximately 36.9% of AUS, and 10.4% of PP procedures over the study period. Annual AUS utilisation in this cohort increased from 7 procedures in 1994 to 333 in 2024, representing a 48-fold increase, while PP procedures rose to a lesser extent from 18 to 114 annually, representing a 6-fold increase. From 2022, men aged ≥75 years comprised more than half of all AUS procedures nationally.
Conclusion: Andrological implant surgery in men aged ≥75 years has increased substantially over the past three decades, particularly for AUS implantation. This change is indicative of evolving attitudes towards continence and sexual function later in life and may reflect improved perioperative care and prostate cancer survivorship. Chronologic age along should not be viewed as a barrier to definitive surgical management in appropriately selected older men.
Introduction
Erectile Dysfunction (ED) and stress Urinary Incontinence (SUI) are prevalent conditions among older Australian men, and their incidence increases with age [1]. Data from the English Longitudinal Study Of Ageing (ELSA) have demonstrated an association between the conditions in older men [2]. Population-level studies, such as the Massachusetts Male Aging Study [3], Men In Australia Telephone Survey (Mates) [1] and 45 and Up Study [4], have consistently demonstrated that moderate to severe ED peaks beyond the seventh decade of life, while SUI may affect up to 12% of Australian men aged 70-74 [5]. Together, these conditions exert a significant impact on quality of life, affecting psychologic wellbeing, intimate relationships social participation and physical function [6-8]. Beyond symptom burden,ED and SUI are increasingly recognised as clinically meaningful conditions in older age. Incontinence and persistent sexual dysfunction are associated with loss of independence, psychological conditions such as anxiety and depression and reduced self-esteem [5,6]. These outcomes remain relevant to older men, many of whom value sexual intimacy and maintain active relationships [9]. As a result, ED and SUI should not be viewed as inevitable sequelae of aging, but as conditions with the potential for substantial quality of life impairment.A substantial proportion of complex ED and SUI in older men occur in the context of prostate cancer treatment [10]. Radical treatments including radical prostatectomy and radiotherapy are increasingly offered to older men, reflecting improved oncologic and functional outcomes post treatment [11-14]. As survivorship following prostate cancer improves, long term function outcomes, including severe treatment related ED and incontinence have emerged as important survivorship indices.Consequently, the demand for definitive surgical solutions may be expected to extend into older age groups. Penile prosthesis implantation and Artificial Urinary Sphincter (AUS) surgery represent definitive management for refractory ED and SUI respectively. Both procedures are well established and are associated with high patient satisfaction in appropriately selected patients [15-18]. However, surgical management in elderly men has historically been approached with caution. Over recent decades, several factors have prompted re-evaluation of this paradigm in surgery, including urology, with a growing recognition that functional and individual patient goals are more critical than chronologic age alone [19,20]. Advancements in peri-operative care and implant technology have also challenged traditional paradigms.An analysis of long-term, population-adjusted trends is needed to analyse changing practice patterns in andrology implant surgery in Australia. The availability of 30 years of MBS data provides a unique opportunity to investigate these trends using age-stratified, population-adjusted statistics. This study aims to analyse national trends in penile prosthesis and AUS surgery in Australia in the geriatric population and contextualise these trends with evolving attitudes towards andrological care in older men.
Methods
A retrospective population-based observational study was undertaken examining national trends of andrological implant surgery in Australia. Procedure-level data was obtained from the Australian Medicare Benefits Schedule (MBS), which captures medical services subsidised by the Australian Government, Annual item-level claims data were extracted from the period of 1994 to 2024. This data provides aggregated counts of services for each year stratified by state of provision and age group, but does not provide individual clinical data, indication for surgery, comorbidities, or outcomes.The study population comprised of males aged 75 or older at the time of service provision, with age stratification performed using MBS-reported age categories and stratified using Australian Bureau of Statistics population data. Comparator groups (<75 years) were examined to contextualise trends observed in the >75-year cohort.
Andrological implant procedures of interest were identified using relevant MBS item numbers
- Item 37429: Artificial erection device, insertion of pump and pressure-regulating reservoir
- Item 37426: Artificial erection device, insertion of, into one or both corpora
- Item 37432: Artificial erection device, complete or partial revision or removal of components, with or without replacement
- Item 37381: Artificial urinary sphincter, insertion of cuff, perineal approach
- Item 37384: Artificial urinary sphincter, insertion of cuff, abdominal approach
- Item 37390: Artificial urinary sphincter, revision or removal of, with or without replacement
The primary outcome was annual utilisation of penile prosthesis and artificial urinary sphincter surgery in men aged 75 years and older, with rates standardised per 100,000 Australian men. Secondary outcomes included proportion of total national penile prosthesis and AUS procedure performed in men 75 and older, temporal trends in utilisation over the study period, and comparative trends between penile prosthesis and AUS implantation within the 75 year and older cohort.Descriptive statistics were used to analyse annual procedure counts and proportions. Where appropriate, trends in the 75 year and older cohort were compared with those in younger age groups using proportional analysis. All analyses were conducted using aggregated MBS data. Inferential statistical testing was not performed. Items 37429 and 37426 are typically billed together for inflatable prosthesis insertion. To avoid double counting, counts from 37426 and 37429 were combined and halved and results rounded to the nearest whole number, recognising this may modestly underestimate malleable prothesis rates.This study used publicly available, deidentified, aggregated administrative data and in accordance with national guidelines, formal human research ethics committee approval was not required.
Results
Between 1994 and 2024, a total of 7,474 AUS procedures and 12,881 penile prosthesis procedures were recorded in Australia through the Medicare Benefits Schedule. Annual national procedure counts increased over the study period, with annual AUS procedures rising from 49 in 1994 to 591 in 2024, and penile prosthesis procedures rising from 301 in 1994 to 697 in 2024. Marked growth was observed for both groups from the mid 2000s onwards (Table 1).
|
AUS (n) |
AUS (%) |
PP (n) |
PP (%) |
|
|
15-24 |
60 |
0.8 |
27 |
0.21 |
|
25-34 |
35 |
0.47 |
139 |
1.08 |
|
35-44 |
33 |
0.44 |
445 |
3.45 |
|
45-54 |
119 |
1.59 |
1615 |
12.54 |
|
55-64 |
1002 |
13.41 |
4543 |
35.27 |
|
65-74 |
3462 |
46.32 |
4767 |
37.01 |
|
75-84 |
2488 |
33.29 |
1271 |
9.87 |
|
85+ |
275 |
3.68 |
74 |
0.57 |
|
Total |
7474 |
100 |
12881 |
100 |
Table 1: Total National Activity of Artificial Urinary Sphincter and Penile Prosthesis related procedures 1994-2024.
Over the study period, 2,763 (36.97%) AUS procedures and 1,345 (10.44%) penile prosthesis procedures were performed in men aged 75 and older. From 1994 to 2024 annual utilisation of implant surgery in Australia aged 75 years and older rose substantially for both AUS and PPI. AUS volumes rose from 7 procedures in 1994 to 333 in 2024. Penile prothesis related procedures increased more modestly in the 75 years and older age group, from 18 procedures in 1994 to 114 in 2024, with utilisation peaking at 140 procedures in 2023. Overall growth over the study period was greater for AUS (~48-fold) than for penile prothesis procedures (~6-fold).In the early study period, utilisation was low and relatively stable for both procedures. A clear acceleration in AUS uptake occurs from the mid 2000s, with annual counts increasing from 19 to 40 in 2006, with a sustained rise thereafter with annual volumes exceeding 100 from 2014 onwards. Penile prothesis procedures increased more gradually over time. In the most recent decade, annual volumes typically ranged between 60 and 100 procedures, with a peak in 2023 (140).The relative utilisation of AUS and PPI in men aged over 75 changed over time. In earlier years, penile prosthesis volumes were similar, or exceeding AUS volumes (2008 penile prosthesis 31, AUS 30). From 2009 onward, AUS annual counts were consistently higher than PPI, with the gap between procedures widening over time (Table 2).
|
Year |
AUS ≥ 75 |
AUS ≥75 (%) |
PP ≥75 (n) |
PP ≥75 (%) |
|
1994-1999 |
48 |
14.86 |
71 |
4.39 |
|
2000-2004 |
59 |
16.25 |
60 |
5.01 |
|
2005-2009 |
168 |
24.07 |
127 |
8.46 |
|
2010-2014 |
371 |
27.81 |
189 |
8.09 |
|
2015-2019 |
798 |
36.11 |
395 |
12.66 |
|
2020-2024 |
1319 |
51.08 |
510 |
16.31 |
Table 2: Total number and % of national activity of Artificial Urinary Sphincters and Penile Prosthesis related procedures 1994-2024 in those aged ≥ 75.
The proportion of implant procedures performed in men aged 75 or older increased over time for both AUS and penile prothesis. For AUS, men aged ≥75 accounted for 14.3% of all AUS procedures in 1994, increasing to 56.3% in 2024. From 2022 onward, men aged ≥75 comprised more than half of all AUS recipients nationally. The proportion of penile prosthesis procedures performed in men ≥75 increased from 6% in 1994 to 16.4% in 2024, with a peak of 19.5% in 2023. When considered alongside annual counts, the findings demonstrate growth in implant utilisation among older men not only in procedural volume, but increasing share of national implant activity occurring at this age, especially for AUS (Figure 1).
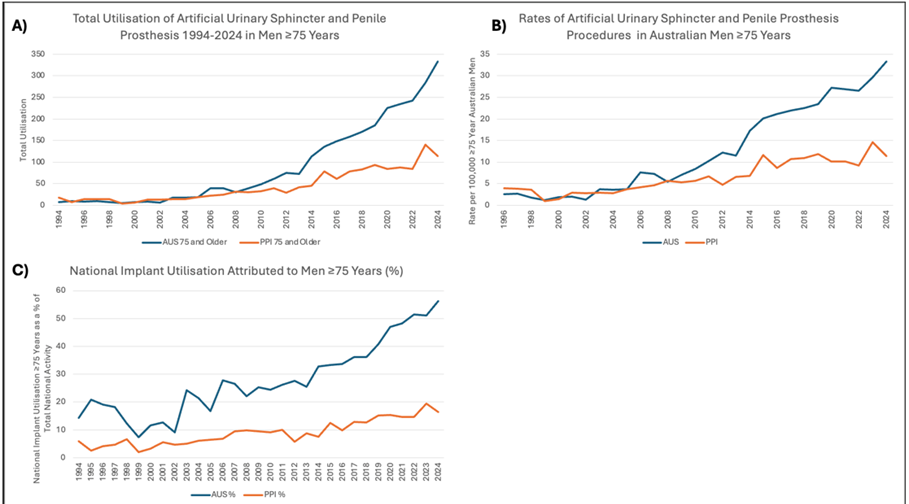
Figure 1:
A) Total Utilisation of AUS and PP 1994-2024 in Australian men ≥75 Years
B) Standardised Rates of AUS and PP in Australian men ≥75 Years per 100,000 men
C) National Implant Utilisation Attributed to Australian men ≥75 Years as a % of Total Implant Activity
Discussion
Implant surgery in older men is an increasingly important component of contemporary andrological care. In this national MBS analysis, utilisation of both AUS and penile prosthesis procedures among Australian men aged ≥75 years increased over the last three decades. Annual AUS procedures in this cohort increased from single-digit volumes in the mid 1990s to several hundred procedures per year by 2024 (n=333).Penile prosthesis procedural volume also increased, although more modestly. Importantly, the age distribution of AUS recipients shifted substantially, with the proportion of all AUS procedures in men aged ≥75 years exceeding half of national activity from 2022 onward (56% in 2024). A smaller, but consistent age shift was also observed for penile prothesis procedures, with older men comprising ~16% of national activity. Together, these findings suggest demographic change and evolving clinical attitudes towards sexual and continence outcomes as legitimate priorities in older age, with the burden of severe urinary incontinence and complex ED later in life increasingly being addressed with definitive surgical solutions.Historically, published cohorts have reported generally low utilisation of AUS and penile prosthesis in men aged >70 compared to younger men [21,22].Often this is attributed to concerns regarding comorbidity burden and device related complications including erosion and infection. Although some earlier series suggests higher complication rates in older men despite acceptable overall device survival [22], contemporary series have challenged this notion, showing AUS to be a safe and effective option in patients with severe SUI over the age of 70 [23,24]. Similar attitudes have been challenged in relation to penile prosthesis implantation, with Chung et al demonstrating no significant difference in device survival, and high patient satisfaction in men aged 75 and older undergoing prosthesis implantation [25]. Several factors likely explain this observed expansion of implant surgery in older men. Progressive reframing of sexual health and continence as legitimate functional outcomes in older age rather than luxury concerns may increase the likelihood of older men pursuing treatment for SUI and ED. Severe SUI in older men is associated with increased care requirements, as well as significant physical, psychological and social morbidity [5,7,8,26]. Reconceptualising AUS in this way as a function-restoring intervention may partially explain this expansion. Studies have demonstrated sexuality, and intimacy remains important in advancing age [9,7],with up to 30.8% of people aged over 75 having had at least one sexual encounter in the past 12 months [27,28], and recognition of these changing attitudes may also contribute to increased uptake in older populations.Additionally, improvements in perioperative care have improved outcomes for older adults undergoing surgery. One major developments includes the implementation of the Comprehensive Geriatric Assessment (CGA) [29], recommended by the American Geriatrics Society, Society of Anaesthesiologists, and American College of Surgeons. This structured, often multidisciplinary, evaluation of the elderly being considered for surgery aims to create a plan to optimise health and function after assessment of multiple domains including medical, functional status, frailty and physiologic reserve to modify risk in the perioperative period, reducing post-operative complications. This is particularly useful in implant surgery, as this framework assists in selective patients based on biologic fitness and highlights practical issues which matter for implants, including cognition, dexterity, ability to attend follow up, and optimisation to reduce infection risk. In Australia, perioperative geriatric services have been successfully employed in acute surgical units for elderly patients, and shown to maintain low numbers of surgical complication, length of stay, and patient re-presentation [30]. These improvements in perioperative care have enabled a broader pool of elderly patients to undergo surgery safely, increasing the pool of patients who may be considered for implant surgery.A large proportion of men undergoing andrologic implant surgery occurs in the context of prostate cancer treatment. The contribution of prostate cancer survivorship to the burden of SUI and complex ED later in life is considerable. As survivorship improves, more men are living to experience persistent treatment related SUI and ED, for while AUS and penile prosthesis represent established, definitive options. Kopp et al demonstrated that compared with age-matched men without prostate cancer, elderly prostate cancer survivors have a two to five fold greater prevalence of urinary incontinence, with this disparity increasing with time since diagnosis [31].
Additionally, pad-free and social continence rates post robot-assisted radical prostatectomy markedly decline with age [32], highlighting the need for targeted management strategies in this population. AUS may provide a durable solution for these men, with elderly men demonstrating significantly improved continence, with acceptable device survival [22,33]. Contemporary series highlight that frailty, rather than age along, should be incorporated into perioperative decision making for elderly men being considered for AUS surgery [34]. This evolution away from age and towards assessment of frailty is reflected in contemporary guideline consensus position. Major groups consistently emphasise comprehensive preoperative evaluation in older populations, rather than chronologic age thresholds. The American Urological Association (AUA) [35], British Association of Urological Surgeons (BAUS) [36] and Asia-Pacific AMS 800 Artificial Urinary Sphincter Consensus Statement [37] recommend preoperative assessment for men being considered for AUS including cognitive status, manual dexterity evaluation and functional status, rather than relying on age alone.The more dramatic age shift for AUS compared with penile prosthesis is consistent with survivorship-linked continence burden that is difficult to substitute with non-operative alternatives and may reflect treatment priorities in men after prostate cancer treatment.
By contrast, ED has multiple non-surgical therapies including phosphodiesterase-5 inhibitors, intracavernosal injections and vacuum devices [38,39].Older men may elect to continue non-operative therapy, accept residual dysfunction, or prioritise other health concerns contributing to a slower growth in penile prosthesis utilisation.This study has several important limitations inherit to the use of MBS claims data. Primarily, clerical inaccuracies, recording bias, and temporal changes in coding can affect the consistency and comparability of data, making longitudinal studies challenging [40].Moreover, data completeness and accuracy can vary significantly, with an Australian vascular audit finding a 63% capture rate, indicating underestimation of total activity [41]. Specific to MBS claims data, procedures are only captured if billed via Medicare, generally in the private sector, and although the majority of implant surgery occurs in the Australian private hospital sector, overall activity is underestimated. Moreover, the use of aggregated data prevents capture of clinical details surrounding implant surgery such as indication, symptom severity, prior treatments or patient reported outcomes. These limitations mean that findings should be interpreted as describing temporal patterns of service delivery as opposed to appropriateness or outcomes of implant surgery in older men.
Conclusion
National claims data indicates utilisation of AUS and penile prosthesis procedures has increased over the past three decades. Specifically, utilisation has increased substantially in men aged ≥75 years. Findings suggest a gradual cultural shift in how andrological health is valued in older men, and may reflect in part improve prostate cancer survival, with a larger pool of older men seeking definitive surgical solutions to treatment related incontinence and erectile dysfunction.
References
- Holden CA, McLachlan RI, Pitts M, Cumming R, Wittert G, et al. (2005)Men in Australia Telephone Survey (MATeS):a national survey of the reproductive health and concerns of middle-aged and older Australian men. Lancet 366: 218-224.
- Lee DM, Tetley J, Pendleton N (2018) Urinary incontinence and sexual health in a population sample of older people. BJU Int 122: 300-308.
- Johannes CB, Araujo AB, Feldman HA, Derby CA, Kleinman KP, et al.(2000)INCIDENCE OF ERECTILE DYSFUNCTION IN MEN 40 TO 69 YEARS OLD: LONGITUDINAL RESULTS FROM THE MASSACHUSETTS MALE AGING STUDY. The Journal of Urology 163: 460-463.
- Weber MF, Smith DP, O'Connell DL, Patel MI, de Souza PL,et al. (2013)Risk factors for erectile dysfunction in a cohort of 108 477 Australian men. Med J Aust 199: 107-111.
- Kwong PW, Cumming RG, Chan L, Seibel MJ, Naganathan V, Creasey H, et al. (2010) Urinary incontinence and quality of life among older community-dwelling Australian men: the CHAMP study. Age Ageing 39: 349-354.
- Lu Y, Fan S, Cui J, Yang Y, Song Y,et al.(2020)The decline in sexual function, psychological disorders (anxiety and depression) and life satisfaction in older men: A cross-sectional study in a hospital-based population. Andrologia 52: e13559.
- Sørensen KH, Levinsen AKG, Kjaer TK, Borre M, Brasso K,et al. (2026)Associations Between Stress Urinary Incontinence and Self-reported Functioning and Urinary Symptoms Among Survivors of Prostate Cancer Treated With Radical Prostatectomy. Urology 207: 207-211.
- Shaw NM, Breyer BN, Walter LC, Sudore RL, Suskind AM, et al. (2024)How older men live with stress urinary incontinence: Patient experience and navigation to treatment. Neurourol Urodyn 43: 11-21.
- Fileborn B, Hinchliff S, Lyons A, Heywood W, Minichiello V,et al. (2017)The Importance of Sex and the Meaning of Sex and Sexual Pleasure for Men Aged 60 and Older Who Engage in Heterosexual Relationships: Findings from a Qualitative Interview Study. Arch Sex Behav 46: 2097-2110.
- Donovan JL, Hamdy FC, Lane JA, Mason M, Metcalfe C,et al. (2016)Patient-Reported Outcomes after Monitoring, Surgery, or Radiotherapy for Prostate Cancer. N Engl J Med 375: 1425-1437.
- Roberts MJ, Papa N, Perera M, Scott S, Teloken PE, et al. (2019)A contemporary, nationwide analysis of surgery and radiotherapy treatment for prostate cancer. BJU Int 124: 31-36.
- Yu V, Treacy PJ, Thanigasalam R, Ahmadi N, Doeuk N, et al.(2026)Robotic-Assisted Radical Prostatectomy in the Elderly Patient-A Study of Functional, Surgical, and Oncological Outcomes in an Australian Cohort. Prostate 86: 158-166.
- Singhal U, Hollenbeck BK, Kaffenberger SD, Salami SS, George AK, et al. (2023) Comparing Patient-reported Functional Outcomes After Radical Prostatectomy in Historical and Contemporary Practice. J Urol. 210: 771-777.
- Goineau A, Campion L, d'Aillières B, Vié B, Ghesquière A, et al. (2018) Comprehensive Geriatric Assessment and quality of life after localized prostate cancer radiotherapy in elderly patients. PLoS One 13: e0194173.
- Pillay B, Moon D, Love C, Meyer D, Ferguson E,et al. (2017) Quality of Life, Psychological Functioning, and Treatment Satisfaction of Men Who Have Undergone Penile Prosthesis Surgery Following Robot-Assisted Radical Prostatectomy. J Sex Med 14: 1612-1620.
- Luna E, Rodriguez D, Barrios D, Hernandez H, Bianco F, et al. (2022) Evaluation of Quality of Life After Inflatable Penile Implantation and Analysis of Factors Influencing Postsurgery Patient Satisfaction. J Sex Med 19: 1472-1478.
- Peterson AC, Wood HM, Myers J, Breyer BN, Erickson BA, et al. (2026) The Artificial Urinary Sphincter Improves Emotional Health in Men With Stress Urinary Incontinence: Results From the Prospective, Multi-institutional AUSCO Study. Urology 207: 227-232.
- Deruyver Y, Schillebeeckx C, Beels E, De Ridder D, Van der Aa F (2022) Long-term outcomes and patient satisfaction after artificial urinary sphincter implantation. World J Urol 40: 497-503.
- Ajitsaria P, Lott N, Baker A, Lacey J, Magnusson M,et al. (2023) Protocol paper for SMART OPS: Shared decision-making Multidisciplinary Approach - a Randomised controlled Trial in the Older adult Population considering Surgery. BMJ Open 13: e070159.
- Droz JP, Aapro M, Balducci L, Boyle H, Van den Broeck T, et al. (2014)Management of prostate cancer in older patients: updated recommendations of a working group of the International Society of Geriatric Oncology. Lancet Oncol 15: e404-e414.
- Davis R, Ginsberg D, Loh-Doyle JC (2025)Utilization of Incontinence Procedures Following Prostate Cancer Treatment: A Population-Level Analysis. Neurourol Urodyn 44: 1621-1627.
- Ziegelmann MJ, Linder BJ, Rivera ME, Viers BR, Rangel LJ,(2016) Outcomes of artificial urinary sphincter placement in octogenarians. Int J Urol 23: 419-423.
- Chung E, Wang J, Cartmill R. (2022) Is artificial urinary sphincter surgery safe and effective in elderly males aged 70 years and above? Low Urin Tract Symptoms 14: 416-420.
- Girard C, El-Akri M, Durand M, Guérin O, Cornu JN, et al. (2023) Efficacy, Safety, and Reoperation-free Survival of Artificial Urinary Sphincter in Non-neurological Male Patients over 75 Years of Age. Eur Urol Open Sci 53: 23-30.
- Chung E, Solomon M, DeYoung L, Brock GB.(2014) Clinical outcomes and patient satisfaction rates among elderly male aged ≥75 years with inflatable penile prosthesis implant for medically refractory erectile dysfunction. World J Urol 32: 173-177.
- Sims J, Browning C, Lundgren-Lindquist B, Kendig H. (2011) Urinary incontinence in a community sample of older adults: prevalence and impact on quality of life. Disabil Rehabil 33: 1389-1398.
- Bauer M, Haesler E, Fetherstonhaugh D(2016)Let's talk about sex: older people's views on the recognition of sexuality and sexual health in the health-care setting. Health Expect 19: 1237-1250.
- Hyde Z, Flicker L, Hankey GJ, Almeida OP, McCaul KA, et al. (2010) Prevalence of sexual activity and associated factors in men aged 75 to 95 years: a cohort study. Ann Intern Med 153: 693-702.
- Welsh TJ, Gordon AL, Gladman JR.(2014)Comprehensive geriatric assessment--a guide for the non-specialist. Int J Clin Pract 68: 290-293.
- Styan L, Murphy S, Fleury A, McGowan B, Wullschleger M. (2018) Establishing a successful perioperative geriatric service in an Australian acute surgical unit. ANZ J Surg 88: 607-611.
- Kopp RP, Marshall LM, Wang PY, Bauer DC, Barrett-Connor E,et al. (2013)The burden of urinary incontinence and urinary bother among elderly prostate cancer survivors. Eur Urol 64: 672-679.
- Gondoputro W, Thompson J, Evans M, Bolton D, Frydenberg M, et al. (2022) How Does Age Affect Urinary Continence following Robot-Assisted Radical Prostatectomy? A Prospective Multi-Institutional Study Using Independently Collected, Validated Questionnaires. J Urol 207: 1048-1056.
- O'Connor RC, Nanigian DK, Patel BN, Guralnick ML, Ellision LM, et al. (2007) Artificial urinary sphincter placement in elderly men. Urology 69: 126-128.
- Medendorp AR, Anger JT, Jin C, Amin KA, Hampson LA, et al. (2019)The Impact of Frailty on Artificial Urinary Sphincter Placement and Removal Procedures. Urology 129: 210-216.
- Sandhu JS, Breyer B, Comiter C, Eastham JA, Gomez C,et al. (2019)Incontinence after Prostate Treatment: AUA/SUFU Guideline. J Urol 202: 369-378.
- Bhatt NR, Biers S, Sahai A, Belal M, Kozan A, et al.(2025) British Association of Urological Surgeons (BAUS) consensus document on post-prostatectomy incontinence-stress urinary incontinence. BJU Int 135: 887-901.
- Chung E, Liao L, Kim JH, Wang Z, Kitta T, et al. (2023) The Asia-Pacific AMS800 artificial urinary sphincter consensus statement. Int J Urol 30: 128-138.
- Salonia A, Capogrosso P, Boeri L, Cocci A, Corona G, et al. (2025) European Association of Urology Guidelines on Male Sexual and Reproductive Health: 2025 Update on Male Hypogonadism, Erectile Dysfunction, Premature Ejaculation, and Peyronie's Disease. Eur Urol 88: 76-102.
- Burnett AL, Nehra A, Breau RH, Culkin DJ, Faraday MM, et al. (2018) Erectile Dysfunction: AUA Guideline. J Urol 200: 633-641.
- Patel AA, Singh K, Nunley RM, Minhas SV (2016) Administrative Databases in Orthopaedic Research: Pearls and Pitfalls of Big Data. J Am Acad Orthop Surg 24: 172-179.
- Beiles CB, Bourke BM (2014) Validation of Australian data in the Australasian Vascular Audit. ANZ J Surg 84: 624-627.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.