Secure Technological Solution for the Implementation of a New Cross-Border Health Care Model
by Eduardo Hidalgo-Fort1*, Fernando Muñoz-Chavero1, Javier López-Narbona2, Jesús Carrillo-Castrillo2
1Electronic Engineering Department. University of Seville, Camino de los Descubrimientos sn, Seville, 41092, Andalusia, Spain
2Consejería de Salud y Consumo. Junta de Andalucía. Avenida de la Innovacion sn. Edificio Arena 1. Seville, 41020, Andalusia, Spain
*Corresponding author: Eduardo Hidalgo-Fort, Electronic Engineering Department, University of Seville, Camino de los Descubrimientos SN, Seville, 41092, Spain
Received Date: 10 June, 2024
Accepted Date: 17 June, 2024
Published Date: 20 June, 2024
Citation: Hidalgo-Fort E, Muñoz-Chavero F, López-Narbona J, Carrillo-Castrillo J (2024) Secure Technological Solution for the Implementation of a New Cross-Border Health Care Model. J Family Med Prim Care Open Acc 8: 262. https://doi.org/10.29011/2688-7460.100262
Abstract
This article presents the design and implementation of a complete technological solution which allows a new cross-border care model through a profound change in the health management by integrating the pharmacy offices into the public healthcare system. This integration has many advantages, not only because of its proximity and close relationship with patients, but also because the staff in pharmacies is highly qualified and pharmacies represent a link between public and private health care. The proposed technological solution consists of different biosensors, user interface suitable for each of the actors and the deployment of communications and cloud computing platform. The new care model has been validated thanks to three different use cases deployed in 10 pharmacy offices, 10 Health Centers and more than 100 patients around Andalusia (Spain) health area for 6 months: early detection of fragility, new medication adherence, and taking biomedical constants.
Keywords: Health care Model; Cross-border healthcare; COVID-19; Pharmacy integration; Health chain
Introduction
According to Spanish National Healthcare system [1], in the year 2020, there is one pharmacy office for approximately every 2,100 inhabitants in Spain, that’s mean more than 22000 pharmacy offices. In addition, national regulation [2] limits the minimum distance between pharmacies to 250m and the distance between pharmacy offices and public healthcare centres to 200m, causing them to be evenly distributed throughout the territory so that all citizens have a pharmacy nearby. This capillarity, therefore, makes them a strategic element for the attention of practical cases for which their staff has the appropriate training, such as the taking of biomedical constants or the detection of frailty in the elderly, among others.
This project presents the design of a complete technological solution that allows the integration of pharmacy offices in the public health system. This integration would give rise to a new healthcare model with some important advantages in terms of quality, efficiency, and proximity, such as:
Reliability in taking measurements: One of the most important factors for making an accurate diagnosis lies in the quality of the bio measurements acquired. Pharmacy staff are qualified for some of the most common interventions in primary care centres, such as taking biomedical constants or early detection of fragility, defined as the progressive age-related deterioration of physiological systems leading to a decrease in the reserves of intrinsic capacity [3], which would guarantee their quality and, therefore, the quality of diagnosis.
Public-private link: Pharmacies are the main common element between public and private health and, therefore, this places them as a strategic element since they have more medical and personal information about the patients than the Health Centres (private or public ones). This information allows them knowing the complete clinical cases, to which would be added the knowledge of the parapharmacy elements that each patient uses. Once again, knowledge of this information has a direct impact on the quality of diagnoses.
High frequentation and closeness: The kind of patients targeted by the new care model proposed (over than 65 years old with chronic disease or fragility), is assiduous in visiting pharmacies regularly, which raises two immediate benefits: on the one hand, immediate access to it for any necessary intervention and, on the other hand, the professional-patient relationship is narrowed and strengthened, which allows the professional to obtain an early diagnosis while controlling the details of adherence to the treatments prescribed by the medical staff.
Filter for peaks in demand for Healthcare Centres: The current situation, because of the pandemic caused by COVID-19, has revealed the impossibility of healthcare centres to face the demand requested in situations in which said demand reaches very high levels. During the 9 first months, more than 2.000.000 positive cases were detected of 20.000.000 tests carried out [1], which caused the saturation of current healthcare centres. Due that situation, it seems clear that it was necessary to find a solution to minimize the impact of these situations and try to offer a best healthcare services to final uses. The training of pharmacy office staff enables them, as previously mentioned, to carry out certain interventions on patients, such as taking vital signs or early detection of cases of frailty. This would complement the function of the healthcare centres, freeing them from this workload and therefore facilitating their decongestion and improving sanitary quality at a time of such great need.
The advantages offered by the new healthcare model impact directly on the quality of the services offered, since there will be more qualified personnel assigned to it, and on the health of the healthcare system itself in general (public and private). However, to offer these capabilities, it is necessary to face some challenges, both functional and technological or associated with the usability of the tools, so that the system offers a solution to the needs mentioned for patients and professional staff as well.
One of the most important factors in the management of clinical or medical information is its ownership, which must always belong to the user himself, and its storage and encryption [4], which allows its management and use by the public health system at the time of its affiliation to it. In the proposed new healthcare model, the patient, by means of informed (and signed) consent, allows the use and sharing of the information strictly necessary for the management and intervention in the cases of use foreseen between the three entities that comprise it (public health, private health and community pharmacy). This is controlled through the implementation of a specific security and traceability scheme that will be detailed throughout this article.
So, in an application framework that is increasingly globalized, where periodic healthcare attention for the "fragile" population is very common, the cross-border nature of the care model is fundamental, insofar as it allows the mobility of patients, guaranteeing adequate healthcare of quality, regardless of the geographical location and the professional who attends them.
To demonstrate the advantages and feasibility of the proposed new healthcare system, a pilot experience has been carried out focusing on three use cases:
Early detection of frailty: 30% of people older than 65 years old and 50% older than 80 years old suffer at least one fall a year [3], which entails medical consequences and increases the person's dependency. The shared intervention between healthcare centres and the pharmacy would help to early detection of fragility, as well as the necessary intervention. The service consists of the early detection of fragility through the Barthel test (level of dependency in carrying out basic activities), the walking speed test (time to walk 4m) and the fall risk questionnaire (record of falls in the last year).
Taking constants and therapeutic reinforcement: hypertension affects more than 50% of people older than 65 years old and the degree of control barely reaches 15% of people with diagnosis and prescribed treatment [3]. Diabetes, another highly prevalent chronic pathology in this population, alters basic needs and deteriorates people's quality of life, limiting their autonomy. Chronic Obstructive Pulmonary Disease (COPD) affects this population group, 10% of people older than 70 years old [1] and is the fourth leading cause of death in Spain and has a cost of almost 3Million € due to hospital admissions and treatments. In all these cases, shared intervention between primary healthcare and community pharmacy, both in detection and therapeutic reinforcement, is essential to improve the health and quality of life of patients. The service consists of taking biomedical constants by qualified personnel who guarantee the quality of measurements such as taking temperature, weight, abdominal circumference and Body Mass Index (BMI), blood pressure, glycosylated hemoglobin, oxygen saturation and concentration of carbon monoxide in expired air. After taking bio measurements, intervention or communication to the healthcare centre is carried out if it is necessary, as well as the corresponding therapeutic reinforcement on the use of medication, eating habits, physical activity, sleep and well-being emotional.
Adherence to New Medications (ANM): the service consists in an accompaniment to the elderly when they receive a prescription for a new medication and thus help them to improve their adherence and effectiveness, as well as to optimize pharmacotherapy. It is carried out based on 2 interviews known as Health Coaching whose main objective is to detect people who are not adherent to treatment, and thus facilitate the intervention of the pharmacy staff to solve, in collaboration with the patient, the situation detected.
Finally, the New Care Model aims to demonstrate its viability by means of a technological demonstrator that covers the three cases of use mentioned to improve the quality of life of patients and includes all the actors that make up the healthcare chain, that is: public healthcare centres, offices pharmacy and private healthcare centres.
Materials and Methods
New Healthcare Model
The proposed healthcare model begins in the "recruitment" or ascription phase in which patients older than 65 years old who may suffer (even without a diagnosis) some chronic pathology (hypertension, diabetes or COPD) or some degree of fragility request their inclusion in the program, either on their own initiative or on the recommendation of their referring doctor or pharmacist. At that time, the patient is informed of the case(s) of use applicable(s) to their case and, after accepting the informed consent, they are assigned to aa unique and unequivocal identifier that identifies them in the new model and which is the key to access their personal and medical information stored pseudo-anonymized.
Once registered in the program, the patient, following their calendar, goes to any pharmacy office and, after identifying both the patient and the professional, the necessary intervention is carried out according to the corresponding use case, generating medical records. These registers are potentially accessible by any healthcare and pharmacy staff for their interpretation and act accordingly, always after the authentication mechanism. In the same way, the program itself can generate a series of parameterized alerts classified by their severity for each user which were configured at the time of ascription to the new model. This will notify of said alarms to the corresponding healthcare or pharmacy professionals, who can exchange opinions and information about them through the direct communication channel among any professionals that are part of the program.
The communication channel of the new model is presented as one of the key elements as it is responsible for providing a secure communication channel to share clinical information about patients with other professionals and even with patients if needed and, therefore, converting what are now local and isolated services into global and unified services. This would avoid the exchange of information between different tools, which can lead to interpretation, retransmission of the same or, what is worse, inadequate management of patient information due to the use of tools not provided with the necessary security mechanisms.
As shown, the proposed new healthcare model offers a complete solution for the integration of all the actors that are part of the healthcare chain for patients with some type of chronic pathology or detected frailty, improving on the one hand the quality of the service offered to patients and, on the other hand, and more importantly, improving their quality of life.
Healthcare chain entities
To know the scope of the new healthcare model, it is necessary to detail both the entities that are part of it and the roles assigned to each of these entities:
Public healthcare system: the Spanish national healthcare system provides a reference doctor for each patient and offers them resources available both in hospitals and primary healthcare centres with the aim of offering a quality healthcare service that has a positive impact on patient’s health. As a centralized entity, it has a central and isolated repository where the clinical history of each patient is stored, available so that any professional can consult it in accordance with current regulations. However, it is a regional competence, which means that each Spanish autonomous community has a proprietary service that makes it impossible to globalize information outside its borders, which is considered a major problem in terms of patient mobility and cross-border information.
Private Healthcare systems: many of the users of the public healthcare system have a private insurance whose interventions or prescriptions are unknown to the public system. Overcoming this important inconvenience would have a direct impact on the quality of patient health, as well as on the prevention of possible diseases. Although private healthcare is an important element within the New Healthcare Model, the development carried out, although it allows its ascription to the service, has been piloted with the two main actors (by number of users and resources): Public Health and pharmacy
Pharmacies: thanks to the fact that they have greater capillarity than healthcare centres, they often become the place of reference for those patients with chronic diseases (diabetes, COPD, hypertension, etc.) or with some type of frailty diagnosed, so that places them as a strategic element. Due to their regular attendance at these centres, patients establish a personal relationship with pharmacy professionals, which facilitates and improves the quality of the diagnoses made and allows certain pathologies to be noticed before they are aware of it and go to their healthcare centre. As mentioned above, it is well known that patients often consume parapharmacy elements and even treatments prescribed by private health, which is totally unknown by health centres. All these reasons make pharmacies a strategic point for the early detection of chronic diseases or fragility.
What is detailed in the previous paragraphs highlights the need for a solution that connects all the possible actors present in the health framework of each patient so that the information provided by each of the parties adds value and, therefore, improve the overall quality of service each user receives. This implies, not only a healthcare model that allows to share information, but also establishes a communication channel between any professional, which are described below.
- Healthcare Centres (public or privates):
- Doctors: reference medical personnel for patients who perform medical interventions on patients.
- Nurses: Responsible for caring for patients in nursing tasks.
- Centre referent: this is a necessary and fundamental role to manage the healthcare model change both in the healthcare centre and in the pharmacies, because they are presented as a single interface for them and he/she will perform the functions of control of the flow of patients derived from pharmacies to healthcare centres, carrying out the assignment of interventions to the corresponding doctor or nurse.
- Pharmacy
- Pharmacists: they oversee carrying out interventions in pharmacies for which they are qualified, such as recruiting fragile patients or those with chronic illnesses, taking biomedical constants for the control of chronic pathologies (COPD, diabetes or hypertension) and therapeutic reinforcement to improve their quality of life, as well as the management of medication adherence. In the same way, they become the first line of intervention at the service of health centres, assuming the referral of patients and anticipating to doctors and nurses the information acquired in pharmacies, always through the reference centre and the direct channel of communication of the new model. Once the scope of the new healthcare model has been presented, as well as the entities and roles that comprise it, the architecture implemented to achieve the objectives is detailed.
System Overview
In the deployed architecture diagram (Figure 1), it is shown how all the actors described above are interconnected through the central server interface, which stores the health registrations information, and offer to the users (professionals in healthcare centres, pharmacy and patients) all IT services, like, messaging and health alarms anonymously or graphical representation of bio measurements stored. On the other hand, this central server has a secure MPLS connection with the central data base to guarantee the integrity of the medical data that is stored. On the other hand, it can be seen how the service point of the new healthcare model is in the pharmacy offices, where the professional performs and records the bio measures and questionnaires of the three use cases proposed to determine the status of each patient. It can also be seen how the tablet, which collect the biosensors deployed at the service point of the new model, send their information directly to the secure data base without going through intermediate services, guaranteeing its integrity.
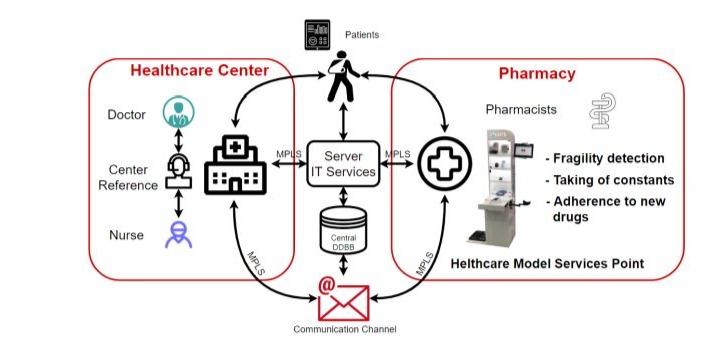
Figure 1: System Overview.
Implementation Aspects
Software technologies applied
As shown, the proposed new healthcare model is based on three main elements: central server, healthcare centres (publics or privates) and pharmacy offices.
The central server is the element that integrates all the actors involved in the healthcare circuit in a single framework that offers secure connections on all its interfaces to guarantee the integrity and security of the information it offers. However, it is important to note how the interface to patients does not require MPLS communication, since it is an interface only for notifications where sensitive information is not used. Additionally, the server implements a personalized permission scheme for the different roles existing in the project: pharmacists, doctors or nursing professionals, who enjoy the same permissions (viewing, editing and creating content associated with their personal profile and their patients) and centre referents, with permissions to manage all the data related to patients and professionals associated with their primary healthcare centre.
From a hardware point of view, the server and its services have been deployed on a virtual machine with 2 vCPUs and 8 GB of RAM. From the software point of view, the main challenge has focused on the development and integration of a series of web applications that guarantee compatibility with the variety of web browsers (Chrome, Firefox, Explorer, Edge, Midori or Safari) installed on both computers of the public healthcare network, as well as private and pharmacies. These technologies have been the following, for each of the functional blocks:
Front-End: JSP technologies have been used for the generation of software blocks and JSTL as a complement, JavaScript for checking forms and basic management of the front-end, the jQuery library for writing and managing the code, as well as jQuery UI for the optimization of the framework and adding functionalities such as Datatables or Datepicker, Ajax for requesting tables and checking forms, and Bootstrap as a style library and responsive design, so that its usability is guaranteed on any type of device. In Figure 2 shows the main page of the graphical interface designed for the proposed healthcare model which integers all services offered, like patients, alarms, bio measurements and appointments management, a specific area for adherence use case, the messaging service and the professional’s directory.
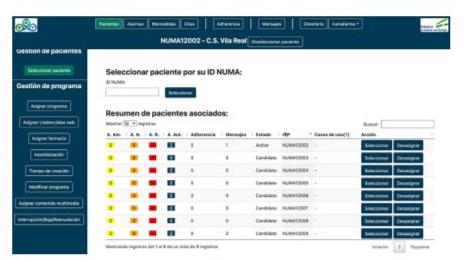
Figure 2: Graphical User Interface. Overview.
Back-End: It has been developed on the Spring framework using Spring Boot, which minimizes dependencies and, therefore, speeds up the execution of the application and Hibernate / JPQL as a library to streamline access to the data base, facilitating the adaptation of the data model to possible future revisions.
Data base (DDBB): MySQL technology with InnoDB engine has been used and it stores both the pseudo-anonymized information of the patients as well as the signed informed consent of each one. Moreover, it stores the graphic material (videos) for the therapeutic reinforcement of the patients.
Connectivity of the New Healthcare Model
Once the new model integrates all the professionals in the healthcare chain as well as pharmacists into a single framework, it is necessary to detail the connection scheme that guarantees the security of the communications carried out and, therefore, the protection and integrity of shared information.
Healthcare Centres (Public or private): Through a dedicated MPLS connection that guarantees the integrity of the information [5]. This implies the need for all health centres to join said MPLS network, either physically or through a secure VPN connection. All healthcare personnel have access to the information of each patient, which is pseudo-anonymized, since it is not related to the patient's identification information (DNI, Name and Surname, etc.) but to a unique identifier that only the patient has. In addition, as a security measure on the privacy of sensitive information, all access to information is recorded, guaranteeing the traceability of all of them.
Pharmacies: They have two different types of connection: on the one hand, the computer, which has the same connection as the healthcare centres, and the point of service, where interventions are carried out on patients. This point has a control tablet with several biosensors connected (body temperature, blood pressure, glycosylated glucose, blood oxygen concentration, heart rate, carbon monoxide concentration in expired air, weight, BMI and perimeter abdominal) which, after taking the bio measurement by the pharmaceutical staff, transmits these values to a local tablet via secured Bluetooth and finally these are sent via a dedicated M2M channel connection [6-9] to the central data base in a secure manner.
Patients: Although the patients have connectivity with the new healthcare model, this will be for the reception of information by the professionals of the program and always anonymously. In addition, it is important to highlight the use of security measures such as connectivity through an external DNS to hide the source IP address, the use of SSL security certificates and the access through HTTPS with control of secure credentials [10].
Communication channel: As previously mentioned, all the professionals (included in a searchable directory) who are part of the new care model have access to a dedicated and direct communication channel in which they can share messages with each other (marked as prioritized or not) and information registered in the new care model, as well as diagnoses, assessments or any information referring to patients, always anonymously. It can be seen in Figure 3 how send, receive and reply messages services are available as well as linking the messages to a specific patient profile or not. Moreover, since this is a service deployed in the central server, the access path to it is made, again, through the secured MPLS network.

Figure 3: Unified messaging service.
Key functional aspects
As far as functional aspects are concerned, the applied technologies and the developments carried out provide a series of capabilities that are key in the new healthcare model for its deployment and acceptance, such as those described in the following paragraphs.
One of the most important added values of the new healthcare model lies in its cross-border nature, which is supported by the communication network and the security methods applied. This characteristic allows assigned professionals to access patient information directly, regardless of the geographical region or the country from which it is accessed, integrating public and private health and pharmacy offices. In this way, this characteristic has a direct impact on the quality of the service offered. On the other hand, it allows patients, especially the chronic ones who are subject to regular check-ups and interventions, to travel and be able to receive such care in any geographical location, thus improving their current experience.
On the other hand, to improve the usability of the tool, the graphic interface is adapted to each type of user, in addition to having a responsive design that guarantees its compatibility with the most used screen formats (computer, tablet and mobile phone). In this way, the interface for professionals is presented with all its potential in terms of the actions it allows to perform while being intuitive, while the user interface that involves patients is even more intuitive, always guiding them to browse through the information sent by professionals. Additionally, to encourage adherence to the deployed model, both FAQ and video tutorial sections were enabled for the most frequent processes.
The design of a specific data model in terms of structure and generic in terms of its parameterization allows establishing a system of automatic notifications categorized by level of severity to the professionals of the healthcare model. These warnings are generated based on the thresholds established at the time of enrolment of a new patient for the records taken in each of the three use cases contemplated. This feature, although it does not replace health professionals, contributes directly to reduce the time spent reviewing patient records and makes it possible to know an alarm status of any patient at the same time of data collection, even if it has not carried out at your health centre, but at any service point of the new model. In this case, medical professionals could request an appointment directly for the patient in question, which would be notified by the communication channel enabled for it.
As can be seen, the main innovation and most notable feature of the proposed care model is the integration, as far as the cases of use contemplated are concerned, of the three levels under a single technological solution that responds to the needs raised and even not resolved by the current model. However, within this solution, the key element that makes this solution possible is the deployment of service points of the new healthcare model in pharmacies.
Service points of the new care model
The service point of the new healthcare model is presented as an area of the pharmacy offices in which all the services contemplated in each of the use cases included in the proposed model are offered comprehensively. This service point has been designed with an attractive aesthetic line in accordance with the aesthetic lines followed in pharmacies as it is shown in Figure 4. In this sense, it has logos and signage that clearly identify it, as well as a series of backlit compartments to present the biosensors and the tablet in an attractive way, as well as an articulated arm for taking blood pressure, a retractable tray to facilitate the task of the pharmacy staff and a lower compartment for the storage of biomedical consumables. Finally, all the equipment is protected under lock and key or by means of security cables.
As can be seen in Figure 4, the service point is fully instrumented to take the necessary bio measurements in the three use cases. It includes the following equipment: Body temperature sensor, pulse oximeter, blood pressure monitor, glycosylated glucose meter, co-oximeter, scale and tape measure, which have the following technical characteristics:
- Body temperature sensor, model FORA IR21 [11]: measurement range from 32ºC to 43ºC, resolution of 0.2ºC (36ºC -39ºC) and 0.3ºC (34ºC -39ºC and 39.1ºC -42.2ºC), internal memory for up to 10 measurements and 2x1.5V AAA power supply.
- Co-oximeter, CO Check+ model [12]: measurement range from 0 to 99 ppm, 1ppm resolution, 2% accuracy and 9V PP3 power supply.
- Glycosylated glucose sensor, Model A1CNow+ Professional [13]: NGSP measurement range from 4% to 13% with 0.1% resolution.
- Body composition monitor, model BF206-BT [14]: body weight measurement range from 0kg to 150kg with 0.1kg resolution, body fat from 5% to 60% with 0.1% resolution, skeletal muscle from 5% to 50% with resolution 0.1%, visceral fat of 30 levels with resolution of 1 level, BMI of 7 to 90 with resolution of 0.1, body age from 18 to 80 years old with resolution of 1 year and metabolism rate from 385kcal to 3999kcal with 1kcal of resolution. 4x1.5V AA power supply.
- Tape measure: 2m long with 1mm resolution.
- Blood pressure sensor, Model 708-BT [15]: oscillometric method, pressure measurement range from 0 to 299 mmHg with +-3mmH precision and pulse from 40 to 180 beats/min with +-5% precision, with electronically controlled inflation, capacitive pressure sensor, memory for 84 measurements and 4x1.5 AA power supply.
- Pulse oximeter, Model Onyx 9560 II [16]: oxygen saturation measurement range from 0 to 100% with +-2% accuracy and pulse rate from 18 to 321 pulses/min with +-6 pulses/min accuracy. 2x1.5AAA power supply.

Figure 4: Two of the ten service points deployed.
In addition, the service point includes the instrumentation control tablet, which collects the information from the sensors and sends it through a secure channel to the central data base. On the other hand, the table, which has a double degree of identification security to allow access (the patient and the pharmacist), allows users to access their profile and consult the history of the interventions carried out. Additionally, this tablet allows to do some questionnaires to determine the quality of life of patients, as well as for the detection of some degree of frailty or the evaluation of adherence to medications. Finally, the service offered at the point of service in general and, for the tablet more specifically, guides users (pharmacy professionals and patients) from the beginning to the end, favouring adherence to it and minimizing the possibility of that users perform some wrong action.
An additional factor that greatly facilitates the deployment and integration of the point of service and all its functionality in the pharmacy as a physical entity and in its operation is the provision of wireless communication to all its elements, both biosensors (Bluetooth) such as the tablet (dedicated M2M channel). In this way, the point of service integrates all the functionality of the pharmacy in terms of the three cases of use contemplated like it is demonstrate in the pilot detailed in the next section.
Pilot Experience and Experimental Results
The main objective of the piloting of the new healthcare model is to demonstrate the implantation of the model and the integration of the entire healthcare chain through the assessment of the most important figure of this healthcare model, the patients, as well as the impact of its implementation on the roles of health professionals. However, although private healthcare is an important element within the New Healthcare Model, the development carried out, although it allows its ascription to the service, has been piloted with the two main actors (by number of users and resources):
Public Health and pharmacy
Since one of the main objectives of the presented model is its cross-border nature, it has been developed in agreement with the health authorities of the Junta de Andalucía through the Ministry of Health (Spain) and the Regional Health Administration of the Algarve (Portugal), so it guarantees the integrability of the new model outside the Spanish borders, which is a fundamental characteristic, especially for geographical areas close to national borders, such as Ayamonte (Huelva – Spain) and the Algarve (Portugal). The Figure 5 (a) shows the 10 Spanish selected pharmacies for the pilot deployment and the Figure 5(b) shows the deployment of pharmacies (red ones) and healthcare centres (blue ones) in Seville.
As shown in Figure 5, the 10 selected pharmacies (and equipped with a service point) with their respective reference health centres are distributed as follows: 7 in Seville city, 2 in the town of Écija (province of Seville) and 1 y the town of Ayamonte -1- (province of Huelva). The distribution of pharmacies meets a criterion of diversity in terms of the socio-economic capacity of the population.

Figure 5: Pilot deployment map. (a) Spanish pharmacies, (b) Pharmacies – red- and Healthcare Centres -blue- deployed in Seville city.
As quantitative results of the deployment carried out, during the 6 months of the pilot, the new healthcare model has been piloted by 169 professionals (83 doctors, 66 nurses, 10 centre referents and 10 pharmacists), who have exchanged 122 messages, and a recruitment of 418 use cases can be highlighted, distributed as it is shown in Table 1, which generate 505 alarms and 17 automatic appointments.
|
Use Case |
Number of Patients |
Patient evaluation of the service (10 max) |
|
Use Case 1: Detection of fragility and risk of falls |
125 |
9.4 Men 9.3 Women |
|
Use Case 2: Adherence to New Medications |
168 |
9.8 Men 9.7 Women |
|
Use Case 3: Taking vital signs and therapeutic reinforcement |
125 |
9.7 Men 9.7 Women |
Table 1: Use Cases Results.
Discussion
Based on the number of patients recruited for the pilot study, a sufficiently representative sample can be considered, with an enough variety of chronic pathologies or degree of frailty to represent the entire target population. Therefore, this highlights the high degree of satisfaction obtained among patients assigned to the new care model without differences in criteria according to gender.
On the other hand, if the geographical distribution of pharmacies is considered, it can be seen as a clear case of mobility of users, initially local (Seville), later provincial (Sevilla - Écija) and finally national (Seville - Huelva), which demonstrates the validity of the new healthcare model as far as cross-border is concerned. On the other hand, the degree of satisfaction of the users (both men and women) shows that the new proposed model generates the same degree of adherence and satisfaction regardless of the socio-economic level of its users, maximizing the globality of the model.
Finally, it is important to highlight that the new care model deployed and detailed in this article manages to integrate the 3 main entities (public and private health and community pharmacy), in favour of improving the quality of the services offered to patients and the liberation of interventions to health professionals for which pharmacy operators are qualified, without putting at risk the rights of patients over their medical and personal information, guaranteeing their anonymization, integrity and security and, in addition, satisfying their expectations according to the data collected in pilotage.
Conclusions
This work proposes a new healthcare model based on a holistic solution for the integration of all the actors in the healthcare chain (public primary healthcare centres, private healthcare and pharmacies). Three particularly relevant use cases are proposed to validate the model, such as the early detection of frailty in people over 65 years of age, the monitoring of biomedical constants in people with chronic pathologies such as hypertension or diabetes and, finally, the control of adherence to new medicines. These use cases demonstrate how the training of pharmacy staff and their integration into them have a direct impact on both the decongestion of health centres, which is particularly important as highlighted by Covid-19, and on the quality of care received by patients. The proposed solution is presented as a cross-border care model that is technologically secure and guarantees the integrity of patients' medical information (private data network and pseudo-anonymization of data), which is particularly important in areas close to borders. This solution therefore guarantees patients in those areas equal availability, quality of service and alternatives in terms of medical care compared to those residing in areas completely surrounded by land in the same country.
Finally, the proposed healthcare model has been validated through the deployment and implementation of 10 pharmacy offices and their associated health centres, geographically distributed throughout the health areas of Andalusia (Spain), where more than 100 users of the system have rated the quality of the services offered by the proposed solution very satisfactorily for more than 6 months. It can therefore be concluded that a new cross-border healthcare model has been validated, offering advantages to all the actors in the healthcare chain by means of a secure and viable technological solution that guarantees the rights of all users.
Disclosure
Author Contributions
Conceptualization, F.M.C, J.L.N, E.H.F and J.C.C; methodology, F.M.C, J.L.N and E.H.F; software, F.M.C and E.H.F; validation, F.M.C, E.H.F and J.C.C; formal analysis, E.H.F and J.L.N; investigation, F.M.C and E.H.F; resources, F.M.C, J.L.N, E.H.F and J.C.C; data curation, F.M.C and E.H.F; writing—original draft preparation, F.M.C and E.H.F; writing—review and editing, F.M.C, J.L.N, E.H.F and J.C.C; supervision, F.M.C and E.H.F.
Institutional Review Board Statement: Not applicable
Data Availability Statement: Not applicable
Acknowledgments
This work has been developed within the framework of the NUMA project (0197_NUMA_5_E) which has been co-financed by the European Regional Development Fund ERDF through the Interreg V-A Spain-Portugal Programme (POCTEP) 2014-2020.
This work has been also developed within the framework of the “Nuevo Modelo Asistencial: Regiones Cardio aseguradas (NUMAPLUS)" project (0237_NUMAPLUS_5_E) which has been co-financed by the European Union through the Interreg VI-A Spain-Portugal Programme (POCTEP) 2021-2027.
Conflicts of Interest: None.
References
- Informe anual del Sistema Nacional de Salud 2022. Resumen Ejecutivo. (2023) En Spanish Ministry Of Health (NIPO: 133-20-031-6). Publications Center. Spanish Ministry of Health.
- LEY 22/2007, de 18 de diciembre, de Farmacia de Andalucía (2008) En Boletin Oficial del Estado (BOE núm. 45. Pág. 10069). Spanish Government.
- Informe mundial sobre el envejecimiento y la salud (2015) Organizacion Mundial de la Salud.
- Pandey AK, Singh P, Agarwal N, Raman B (2018) SecMed: A Secure Approach for Proving Rightful Ownership of Medical Images in Encrypted Domain over Cloud. 2018 IEEE Conference On Multimedia Information Processing And Retrieval.
- Perez A (2014) MPLS Technology. Wiley Data And Cybersecurity 155-183.
- System Design and Implementation of Machine-to-Machine (M2M) for Hypertension Patients (2017) IEEE Conference Publication | IEEE Xplore.
- Enriko IKA, Wibisono G, Gunawan D (2015) Designing machine-to-machine (M2M) system in health-cure modeling for cardiovascular disease patients: Initial study. 2015 3rd International Conference On Information And Communication Technology (ICoICT).
- De Mattos WD, Gondim PR (2016) M-Health Solutions Using 5G Networks and M2M Communications. IT Professional 18: 24-29.
- Maurya A, Bade DS (2014) Design of a wireless health monitoring system based on M2M communication. 2014 International Conference On Control, Instrumentation, Communication And Computational Technologies (ICCICCT).
- Mohsin J, Albermany S (2023) Proposing an IOT Secure Framework for Monitoring COVID-19 Patients. 2023 Al-Sadiq International Conference On Communication And Information Technology (AICCIT).
- ForaCare Asia Pacific. (April 14th, 2024).
- Sanisus Medical (2024) Cooxímetro de mano CO Check+ - Sanisus Medical.
- PTS Diagnostics (2024) A1CNow+ System - PTS Diagnostics.
- ManualsLib (2016) OMRON BF206-BT Instruction Manual.
- Omron Serie 10 Plus. Model BP791IT.
- Onyx® II Model 9560 Finger Pulse Oximeter.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.