Risk Prediction Models for Venous Thromboembolism in Geriatric Patients with Hip Fracture: A Systematic Review and Meta-Analysis
by Qin Guo, Jiaxi Wang, Shiyun Qin, Guilan Huang, Shuyan Zeng, Jinyan Li, Qiuyi Ouyang, Pin Wang, Fengqiu Gong*
Department of Operating Room, The First Affiliated Hospital of Sun Yat-sen University, Guangzhou 510080, Guangzhou, China
*Corresponding author: Fengqiu Gong, Department of Operating Room, The First Affiliated Hospital of Sun Yat-sen University, Guangzhou 510080, Guangzhou, China
Received Date: 15 January 2025
Accepted Date: 20 January 2025
Published Date: 22 January 2025
Citation: Guo Q, Wang J, Qin S, Huang G, Zeng S, et al. (2025) Risk Prediction Models for Venous Thromboembolism in Geriatric Patients with Hip Fracture: A Systematic Review and Meta-Analysis. J Surg 10: 11231 https://doi.org/10.29011/2575-9760.011231
Abstract
Introduction: Many studies on Venous Thromboembolism (VTE) risk prediction models for elderly hip fracture patients, but effectiveness and applicability are unclear.
Objectives: To systematically review published studies on risk assessment models for venous thromboembolism (VTE) in elderly individuals with hip fractures, to provide clinicians and nursing staff with scientific evidence that can aid in clinical decision-making and optimize patient care.
Methods: Data bases like CNKI, SinoMed, Wanfang, VIP, PubMed, Web of Science, Cochrane Library, CINAHL, and Embase were searched from inception to May 31, 2024. Study details like design, data source, outcomes, sample size, predictors, model development, and performance were collected. The PROBAST checklist assessed bias risk and relevance.
Results: Out of 565 studies, seven prediction models were chosen. Each used logistic regression to predict VTE risk. VTE incidence in elderly hip fracture patients ranges from 12.3% to 72.5%. Indicators include time from injury to admission, D-dimer, fibrinogen, and SII. AUC values range from 0.65 to 0.95, showing moderate to high discrimination. However, each study had bias risks due to poor data and limited reporting. Combining models, the aggregated AUC was 0.81 (95% CI 0.73-0.89), indicating good distinction.
Conclusions: Despite the studies indicating some degree of accuracy in predicting venous thromboembolism (VTE) in elderly patients with hip fractures, they all exhibited a significant risk of bias according to the PROBAST criteria. Future investigations should prioritize the development of novel models incorporating larger sample sizes, robust study designs, and multicenter external validation.
Keywords: Deep vein thrombosis; Geriatric patients/Older People; Hip fracture; Meta-analysis; Quality of life; Risk prediction model; Systematic review
Background
Hip fractures are a common orthopedic injury in the elderly, mainly due to the decline in bone density and strength associated with aging [1]. These fractures, which included femoral neck fractures, intertrochanteric fractures, and subtrochanteric fractures, are common among elderly individuals and are associated with significant morbidity and mortality [2]. Epidemiological studies indicate that the absolute number of hip fractures is currently increasing, with a projected increase to 21 million cases by 2050 [3]. The mortality rate following hip fractures can range between 22% and 30% within the first year [4]. Besides the direct effects of hip fractures, including discomfort, restricted movement, and reduced independence, patients frequently endure prolonged bed rest. Extended periods of inactivity increase the likelihood of long-term complications, especially the formation of Venous Thromboembolism (VTE) [5]. VTE, as a serious complication of hip fracture, is significantly associated with the incidence, recurrence risk, and mortality of Pulmonary Embolism (PE), which further illustrates and emphasizes the importance of this disease [6].
Venous Thromboembolism (VTE), a significant yet often overlooked threat to geriatric patients suffering from hip fractures, is a formidable "invisible killer." Its occurrence is intricately intertwined with various factors, including the patient's advancing age, the specific site of the fracture, the surgical outcomes, and a diminished level of physical activity. Significantly, the likelihood of experiencing Deep Vein Thrombosis (DVT) and Pulmonary Embolism (PE) rises considerably after a hip fracture, with incidence rates reported to be between 11% and 57% among these at-risk patients [7-9]. Considering the severity of this problem, it is crucial to pinpoint predictive elements that assist in the early detection and treatment of VTE related to hip fractures. Enhancing the accuracy in forecasting and handling Venous Thromboembolism (VTE) risks in elderly patients with hip fractures has led to the creation and evaluation of predictive models becoming key research directions. These models, through the compilation and analysis of clinical data, coupled with pertinent risk factors, offer patients tailored risk assessments and projections. Such frameworks not only empower physicians to determine the VTE risk of patients with greater accuracy, but also steer the design of clinical treatment and nursing strategies, ultimately increasing patient outcomes and quality of life [10].
This study aimed to conduct a comprehensive evaluation of the current predictive models for Venous Thromboembolism (VTE) risk in geriatric patients sustaining hip fractures. Through a rigorous analysis of the methodologies, assessment metrics, and forecasting capabilities of these models, we aspire to delineate their respective merits, limitations, and scope of applicability. Our objective is to provide clinicians and nursing staff with scientific evidence that can aid in clinical decision-making and optimize patient care. Furthermore, we intend to delve into strategies for refining and enhancing these predictive models, thereby increasing their accuracy and practicality and ultimately contributing to the robust health management of geriatric patients with hip fractures.
Methods
The study protocol was registered on PROSPERO (registration number: CRD42024564428).
Search Strategy
We conducted a comprehensive literature review by exploring data bases in both Chinese and English, recognizing the large Chinese demographic and the global prevalence of English. The investigation covered numerous data bases, such as the China National Knowledge Infrastructure (CNKI), Wanfang Data base, China Science and Technology Journal Data base (VIP), SinoMed, PubMed, Web of Science, Cochrane Library, Cumulative Index to Nursing and Allied Health Literature (CINAHL), and Embase. The search period spanned from the inception of these data bases to May 31, 2024. The search was conducted via a comprehensive set of keywords, including "Venous Phlebothrombosis", "Deep Vein Thrombosis", "Pulmonary Thromboembolism", "Deep Vein", "Pulmonary Thromboembolis*", "Thrombus", "DVT/PTE", "Hip Fracture", "Fracture of Femoral Neck", "Intertrochanteric Fracture", "Subtrochanteric Fracture", "Risk Prediction Model", "Prediction Model", "Model", and "Risk Score". The specific search strategies employed are detailed in the Supplemental Materials.Furthermore, we discovered relevant research by examining the bibliographies of the obtained articles and review papers.
In our systematic review, we followed the PICOTS framework, as recommended by the CHARMS checklist (Critical Appraisal and Data Extraction for Systematic Reviews of Prediction Modelling Studies) by Moons [11]. This framework enabled us to clearly define the scope, methodology, and criteria for the inclusion and exclusion of studies [12]. The key components of our comprehensive review are detailed below:
P (Population): Individuals aged 60 and above with hip fractures, including those of the femoral neck, intertrochanteric area, and subtrochanteric zone.
I(Intervention/Exposure): Risk prediction models for predicting Venous Thromboembolism (VTE) in elderly hip fracture patients who were developed and published (predictors)≥2.
C (Comparator): No rival model.
O (Outcome): The primary outcome of interest was VTE/DVT, without distinction to its subgroups.
T (Timing): The result was forecasted following the assessment of initial admission data, clinical scoring metrics, and pertinent lab markers.
S (Setting): The goal of the risk prediction models is to personalize VTE risk evaluation for elderly patients with hip fractures, thereby supporting the application of specific preventive strategies to reduce negative outcomes.
Inclusion and Exclusion Criteria
Studies were included if they met the following criteria: (1) involved elderly patients with hip fractures; (2) used an observational study design; (3) featured a predictive model; and (4) focused on VTE/DVT as the outcome. The criteria for exclusion included: (1) research that did not create a predictive model; (2) papers not authored in English or Chinese; and (3) studies for which the complete texts were inaccessible even after emailing the authors.
Study Selection and Screening
The screening process of the studies was executed independently by two authors (GQ and WJX). Initially, duplicate studies were systematically eliminated to ensure the uniqueness of the dataset. The leftover studies were then meticulously assessed, concentrating on their titles and summaries, to determine their suitability for inclusion. Once the inclusion and exclusion criteria were rigorously applied, the full texts of the potential candidates were thoroughly reviewed. Furthermore, the bibliographies of all qualifying studies were thoroughly reviewed to find any relevant research that might have been missed during the initial search. In instances where disagreements arose regarding the selection of studies, a collaborative discussion involving three authors (GQ, WJX, and QSY) was conducted to foster a consensus decision.
Data Extraction
In a rigorous and standardized process, two independent reviewers screened the search results to establish eligibility. Differences found while evaluating the eligibility of full-text articles were settled by discussion or by seeking advice from a third reviewer. The information extracted from the selected studies was subsequently systematically categorized into two distinct groups. Initially, fundamental details were collected, including the author's identity, year of publication, research methodology, participant characteristics, data source particulars, and the number of subjects. Secondly, data pertaining to the prediction model was gathered, covering multiple facets such as the method for choosing variables, the strategy for model creation, the validation type employed, the performance evaluation metrics, the approach to missing data, the processing of continuous variables, the final predictors used, and the model's presentation format. For precision and uniformity, one reviewer first extracted the information, which was then confirmed by another reviewer.
Quality Assessment
To evaluate the methodological rigor and potential for bias in the included studies, we employed two well-established assessment tools: the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) framework [13] and the current iteration of the Prediction Model Risk of Bias Assessment Tool (PROBAST) [14]. The GRADE approach categorizes research outcomes and critically assesses the quality of evidence, taking intoaccount six pivotal factors: the study design, potential for bias, inconsistency of results, indirectness of evidence, imprecision, and additional considerations such as publication bias. This framework is tailored specifically for evaluating the quality of evidence in systematic reviews, ensuring a rigorous and standardized evaluation process.
The assessment of bias risk and study applicability was conducted via the PROBAST checklist. Two researchers, GQ and QSY, separately and thoroughly assessed the potential bias and relevance issues of the studies. Specifically, the PROBAST checklist serves as a valuable instrument for the critical evaluation of studies involved in the development, validation, or refinement of prediction models for personalized forecasting. This checklist encompasses 20 signaling questions, organized into four distinct domains: participants, predictors, outcome, and analysis. Each signaling question is answered according to a five-point scale, ranging from "yes" to "no information". Importantly, if any key question in a domain is answered with 'no' or 'likely no', that domain is considered to have a significant risk of bias. On the other hand, the study's overall risk of bias can be deemed minimal only if every domain is uniformly evaluated as having a low risk of bias.
Data Synthesis and Statistical Analysis
A meta-analysis of the area under the curve (AUC) values from the validated models was conducted via Stata software.
Results
Study Selection
Figure 1 illustrates the PRISMA 2020 flow diagram, detailing the thorough search methodology and outcomes for systematic reviews and meta-analyses. The first query produced 565 cataloged entries. Following the elimination of 67 redundant entries found in all data bases, 498 titles and abstracts were reviewed for eligibility. After this review stage, 24 articles were selected for additional assessment. During the subsequent evaluation, 9 studies did include geriatric patients. Additionally, 4 studies lacked a VTE/DVT prediction model, 2 studies were restricted to specific surgeries, 1 model was limited to the calf muscle vein, and 1 study was limited to the study of emergency patients. In the end, this review incorporated seven studies with seven distinct models, while five of these studies were also part of the meta-analysis.
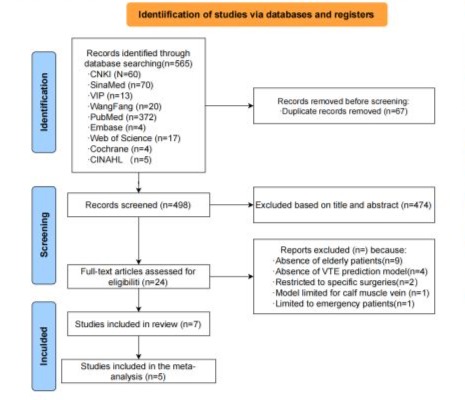
Figure 1: Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) flowchart of the literature search and selection.
Study Characteristics
Table 1 summarizes the design and participant characteristics of the seven included studies. They were published between 2018 and 2024 and were conducted in China. Out of the studies reviewed, two were forward-looking (one being a multicenter study), while the remaining five were backward-looking and carried out in individual centers. Regarding the participants, six studies concentrated on individuals with hip fractures, while one study targeted those with isolated intertrochanteric fractures. The number of participants in the studies varied between 104 and 970. The details of the models used in the studies are shown in Table 2. All the studies employed logistic regression analysis to create predictive models. The predictors most frequently utilized across the models included the duration from injury to hospital admission or DVT screening and D-dimer levels, appearing in seven and six models respectively. Other frequently used predictors included FIB and the SII, which were used in four and three models, respectively. The documented AUC or C-statistic scores varied between 0.65 and 0.95. Calibration was reported for six models, with the Hosmer-Lemeshow test being the most commonly used method.
|
Author (year) |
country |
Study design |
participants |
Data source |
Main outcome |
DVT cases/sample size(%) |
|
Yao, W (2023) |
China |
Retrospective study |
Patients ≥60 years old with femoral neck fractures |
Institution of a hospital |
DVT |
125/970(12.88%) |
|
Wang, Xiaofei (2022) |
China |
retrospective single-center study |
Patients ≥60 years old with an isolated intertrochanteric fracture caused by a low energy injury mechanism |
Orthopedic center of a hospital |
DVT |
105/855(12.3%) |
|
Xing, Fei (2018) |
China |
retrospective study |
Elderly Chinese HF patients ≥60 years |
Orthopedics Department from a hospital |
DVT |
74/248(29.8%) |
|
Zhang, Liang (2022) |
China |
retrospective cohort study |
Geriatric patients with hip fracture ≥ 60 years |
orthopedic department of a Hospital |
DVT |
28/209(13.39%) |
|
Peng, Jiangnan (2021) |
China |
Prospective cohort study |
patients ≥60 years with a hip fracture |
orthopedic department of a Hospital |
VTE |
52/104(50%) |
|
LI ye (2021) |
China |
Prospective cohort study |
patients ≥65 years with a hip fracture |
Orthopedics Department from a hospital |
DVT |
31/128(24.21%) |
|
Chen, Xiao (2024) |
China |
retrospective cohort analysis |
Patients≥60 years with hip fractures |
Department from a hospital |
VTE |
251/346(72.5%) |
Table 1: Overview of the basic data of the included studies.
|
Author (year) |
Missing data handling |
Continuous variable processing method |
Variable selection |
Model development method |
Calibration method |
Validation method |
Final predictors |
Model performance |
Model presentation |
|
|
Yao, W (2023) |
Multiple imputation |
Categorical variables |
Stepwise Regression Analysis |
Multivariable Logistic regression model |
Hosmer- Lemeshow test |
Internal validation external validation |
Smoking,Diabetes, |
A1: 0.792 |
Nomogram model |
|
|
History of VTE, |
(0.786-0.878) |
|||||||||
|
Bedridden time, |
B1:0.888 |
|||||||||
|
D-dimer, |
(0.721-0.901) |
|||||||||
|
Wang, Xiaofei (2022) |
Exclude |
continuous variables |
stepwise back ward method |
Multivariable Logistic regression model |
Hosmer- Lemeshow test |
Internal validation |
History of a VTE, |
A:0.780 |
Nomogram model |
|
|
Peripheral vascular disease, BMI, |
(0.731-0.829) |
|||||||||
|
Delay to DVT examination |
||||||||||
|
Albumin (32.5g/L), |
||||||||||
|
D-dimer>1.0mg/L |
||||||||||
|
Xing, Fei (2018) |
- |
continuous variables |
Single-factor analysis |
Multivariable logistic regression analysis |
- |
Internal validation |
Age, Gender, |
A: 0.852 |
calculated as different cut-off values of statistically significant factors |
|
|
Time from injure to admission, |
(0.806-0.898) |
|||||||||
|
FIB, D-dimer, |
||||||||||
|
Zhang, Liang (2022) |
- |
continuous variables& Categorical variables |
logistic regression model |
Multivariate logistic regression analysis |
Calibration curve of the nomogram prediction model |
Internal validation |
Time from injury to hospitalization, |
A: 0.808 |
Nomogram model and calculate the consistency index (c-index). |
|
|
PLT, D-dimer, |
(0.757-0.866) |
|||||||||
|
FIB, SII, |
||||||||||
|
Peng, Jiangnan (2021) |
- |
Categorical variables |
logistic regression model |
Multivariate logistic regression analysis |
Hosmer-Lemeshow test |
Internal validation |
Time from injury to DVT screening, |
A:0.949 |
Calculating the total risk score according to the program based on the score of each factor |
|
|
Caprini score, |
(0.901-0.996) |
|||||||||
|
SII, FIB |
||||||||||
|
LI ye (2021) |
- |
continuous variables |
logistic regression model |
Logistic regression analysis |
Hosmer- Lemeshow test |
Internal validation |
Time from injury and admission, |
A:0.795 |
Nomogram model |
|
|
Caprini score, SII |
(0.685-0.905) |
|||||||||
|
Chen, Xiao(2024) |
- |
continuous variables |
Least absolute shrinkage and logistic analysis |
Logistic regression Analysis and nomogram techniques |
Calibration plots |
Internal validation |
Gender, |
A:0.648 |
Formula of risk score obtained by partial regression coefficient of each factor |
|
|
Age(years), |
(0.567-0.728) |
|||||||||
|
Time from injury to admission (days), |
B:545 |
|||||||||
|
FIB, D-dimer |
(0.404-0.687) |
“-”, not reported; A, development cohort; B, validation cohort; PLT, platelet count; FIB, fibrinogen level; SII, systemic immune-inflammatory index score; AUC, area under the curve.
Table 2: Overview of the information of the included prediction models.
Model Validation
In the studies reviewed, Yao, W’s[15]model was validated both internally and externally, Xing, Fei’s [16] model underwent internal validation, while the remaining models lacked any form of validation post-development.
Results of the Quality Assessment
According to the GRADE approach, all studies included in this systematic review were evaluated as having high certainty. The corresponding results are shown in the Supplementary Material (Appendix C). Table 3 provides an overview of the bias risk and relevance of the studies that were included. All studies were evaluated as having a high risk of bias, this conclusion underscores the methodological challenges and limitations encountered by these studies, manifested specifically in potential flaws and deficiencies across critical aspects such as study design, data collection, processing, and analysis. Consequently, caution must be exercised in interpreting the findings of these studies, acknowledging the inherent uncertainties and their potential implications for the generalizability and reliability of the conclusions.
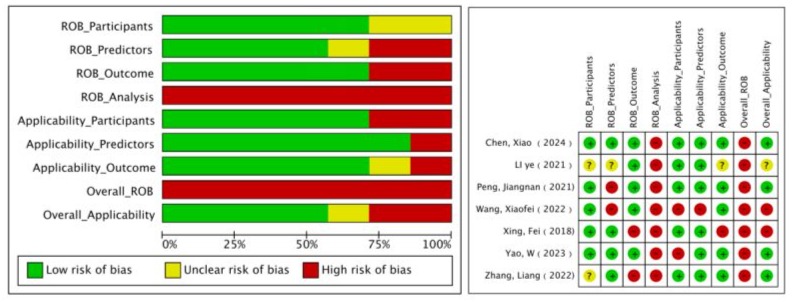
PROBAST, Prediction Model Risk of Bias Assessment Tool; ROB, risk of bias.
A indicates “development only”; B indicates “development and validation in the same publication”. + indicates low ROB/low concern regarding applicability;
- indicates high ROB/high concern regarding applicability; ? indicates unclear ROB/unclear concern regarding applicability.
Table 3: PROBAST results of the included studies.
Within the participant category, two investigations presented an ambiguous risk of bias due to the lack of explicit information about the data source [17,18]. Within the predictor field, two investigations were found to possess a significant risk of bias, while another study exhibited an ambiguous risk of bias. Both studies used outcome information when assessing predictors [19,20]. A particular study exhibited an ambiguous risk of bias due to the omission of quality control measures for predictor evaluation, potentially attributable to its retrospective nature[18]. Within the outcome domain, two studies were found to possess a significant risk of bias due to their definitions lacking predictors, potentially causing an overestimation of the relationships between predictors and outcomes, thereby introducing bias [16,17]. Within the realm of analysis, each of the seven studies exhibited a significant risk of bias. Among the studies, one failed to clarify if the sample size adhered to the guideline of having over 20 Events Per Variable (EPV) [20], three did not analyze all enrolled participants and mishandled missing data [18,19,21], one chose variables based on univariate analysis [16], three studies did not comprehensively assess the predictive performance of their prediction models [17-19], two studies did not provide information on the coefficients of the predictors in the multivariate regression model [20,21] and six relied solely on internal validation using a single random split of participant data, with one exception [21].
Regarding the evaluation of applicability risk, two studies were deemed to have a high risk, four studies were considered to have a low risk, and one study had an indeterminate risk of bias. Within the participant category, two studies were deemed to have a high applicability risk because they included participants restricted to certain subgroups of femoral neck and isolated intertrochanteric fractures. Within the predictor field, a study was flagged for high applicability risk due to issues related to the timing of predictor assessments. In the results area, one research had a significant applicability risk, while another had an ambiguous bias risk due to the definition, time frame, and analysis being additional anticipated outcomes of the system evaluation issue.
Comprehensive analysis of the validation models featured in the review
Five models that were eligible for synthesis and developed via logistic regression were included. Using a random effects model, the combined AUC was determined to be 0.81, with a 95% confidence interval ranging from 0.73 to 0.89 (see Figure 2). The heterogeneity among the studies was substantial, with an I2 value of 91.9% (p < 0.001). Egger's test showed a value of 2.54 (p = 0.12), indicating no notable publication bias (see Appendix D).
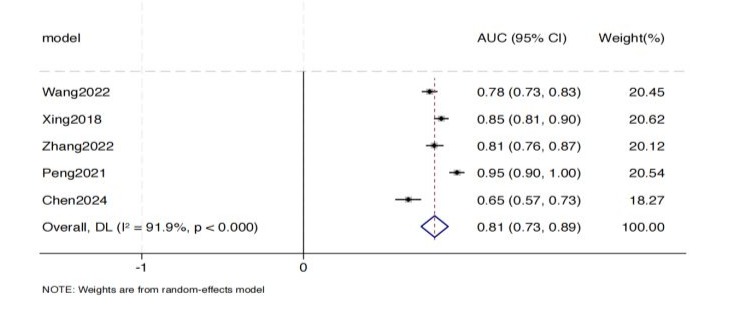
Figure 2: Forest plot of the random effects meta-analysis of pooled AUC estimates for 5 validation models.
Discussion
Elderly patients with hip fractures frequently experience a high rate of VTE. Given the substantial health and financial implications, evaluating the likelihood of VTE in elderly individuals with hip fractures to enable early intervention is essential and can greatly diminish negative consequences. This analysis highlights a growing array of risk assessment models for VTE in elderly individuals with hip fractures, though the majority are derived from Chinese patient information. We assessed seven models that showed moderate to strong predictive accuracy in either internal studies or external validations, with AUC values reported between 0.648 and 0.949. Nevertheless, based on the PROBAST criteria, every study was found to possess a significant risk of bias, which restricts the practical application of these predictive models. The pooled AUC value of the meta-analysis was 0.81 (95%CI: 0.73-0.89). Nonetheless, there was significant variability among the models, potentially due to differing focuses on VTE, predictors, and methodologies. Moreover, while assessing the model, we noticed that the majority of the articles scarcely mentioned the Transparent Reporting of a Multivariate Prediction Model for Individual Prognosis or Diagnosis (TRIPOD) statement [22]. The absence of transparency creates ambiguity and the possibility of biases in the models. Therefore, upcoming research should focus on creating new models with bigger sample groups, stringent study methodologies, multicenter external validation, and improved reporting transparency.
Following a thorough review and assessment of the available literature, seven studies featuring seven distinct models were selected for inclusion in this analysis and subsequent discussion. The creation of the included models offers important insights. Research conducted by Peng [19] and LI et al [18] utilized a prospective cohort design and reported that a longer interval between injury and admission was associated with a higher Caprini score and that an increased SII expression level was an independent risk factor for deep venous thrombosis after the treatment of elderly patients with hip fractures. Additionally, they identified higher SII expression levels as an independent risk factor for deep vein thrombosis in elderly patients treated for hip fractures. The forecasting model, derived from these three elements, effectively predicts VTE risk and serves as a valuable guide for preventing, managing, and treating VTE following hip fractures in older adults. The studies by Yao [23] and Xing [24] et al. utilized a large sample size and performed internal validation. Both investigations indicated a high incidence of DVT among elderly Chinese patients with hip fractures at the time of hospital admission, and developing nomogram models using novel risk factor predictors proved effective for enhancing deep vein thrombosis diagnosis. Numerous studies encountered difficulties related to the number of participants, handling of continuous data, and choice of predictors. Integrating machine learning techniques into model creation can resolve several of these problems. One downside of machine learning models is the present absence of adequate visualization tools. Therefore, scientists need to select the suitable model creation technique depending on particular conditions. In summary, despite the models showing moderate to strong performance, the potential for bias was still significant. Enhancements are required regarding the data origin (whether cohort or case-control study), the duration between predictor evaluation and outcome measurement, the event count, handling of continuous variables, method for choosing predictors, data intricacy, and the calibration and fitting of the model.
The reported existing prediction models in this review also have certain clinical implications. First, the high-frequency predictors were shown to have certain reference significance for nursing practice and future research. The most commonly used predictor across the models was time from injury to admission or DVT screening, which appeared in seven models. As a laboratory indicator, D-dimer is a well-documented and clinically used biomarker for VTE [25] and was identified in five models. However, other studies have reported certain limitations in the use of D-dimer in certain patient groups, such as advanced-aged hospitalized patients or patients with cancer [26]. Therefore, if D-dimer is to be clinically used for VTE in geriatric patients with hip fracture, patients with cancer and the age-adjusted D-dimer cut-off value also need to be further explored.
Three research papers utilized the SII as a predictive factor, suggesting that elderly individuals with hip fractures are at an increased risk of VTE. In recent years, SII has gained popularity as an immune-deficiency index and is recognized as a new, stable, and easily obtainable serological marker for inflammatory immunity [27-29]. The integration of neutrophils, lymphocytes, and platelets enhances predictive accuracy in orthopedics. Based on our findings, the SII is a significant indicator of VTE in elderly individuals with hip fractures. The comprehensive immune-inflammatory index (SII). In recent years, the SII has gained widespread use in reflecting systemic inflammatory immune status, determining prognosis, and stratifying risk. In contrast to other indices like NLR, PLR, and MLR that consider just two cell types (lymphocytes, neutrophils, or monocytes), the SII provides the benefit of including three cell types (lymphocytes, neutrophils, and platelets). This combination offers a broader view of the equilibrium among inflammation, immune response, and blood clotting within the body. Furthermore, the SII has demonstrated superior effectiveness in forecasting survival rates or prognoses compared to the NLR, PLR, and MLR [30]. Research has shown that these processes are somewhat interconnected and influence each other through molecular elements and signaling routes, shedding light on the link between the inflammatory immune response and VTE [31,32]. This understanding offers a conceptual basis for exploring the link between the SII and the likelihood of VTE after hip fractures in older adults.
In conclusion, numerous studies have highlighted the prognostic utility of VTE risk evaluation instruments like the Caprini RAM and the Padua prediction score. While these tools have demonstrated adequate sensitivity, they have also been noted for their low specificity (below 70%) [33]. Consequently, even though there is a pressing demand for VTE prediction models to be used clinically in elderly patients with hip fractures, further clinical studies are required to confirm the efficacy of these models in lowering VTE rates among such patients, before they can be considered for broader use. It is necessary to develop a VTE prediction model for geriatric patients with hip fractures. Future research needs to expand the sample size and explore more easily accessible predictors to improve internal and external validation, making it more universally applicable and operable.
Limitations
This review has limitations. First, most studies were in mainland China, which affects their generalizability to Western populations. Second, owing variations in reporting and methods, only seven models were included. This limited the discussion of heterogeneity and publication bias testing. However, this did not impact model assessment, reflecting shortcomings in methodology and reporting. Future studies should use more rigorous methodologies and transparent reporting. Finally, the review included only English and Chinese studies, potentially excluding findings from other languages.
Conclusion
To sum up, this comprehensive review of seven distinct model studies found an average AUC of 0.81 (95% CI 0.73-0.89) for five comparable models, suggesting a moderate level of discrimination. However, according to the PROBAST assessment, all studies included in this analysis exhibited a significant risk of bias, particularly with concerns raised in seven studies regarding their applicability. Notably, the current prediction models for venous thromboembolism (VTE) in elderly patients with hip fractures fail to meet stringent PROBAST criteria. Consequently, it is essential for researchers to deeply understand the PROBAST checklist and rigorously follow the TRIPOD statement's reporting guidelines to improve the methodological quality and reproducibility of future research. Moreover, upcoming studies ought to focus on creating new predictive models that utilize larger datasets, strong research methodologies, and validation across multiple centers to improve their relevance and applicability in clinical settings.
References
- Bhandari M, Swiontkowski M (2017) Management of Acute Hip Fracture. N Engl J Med 377: 2053-2062.
- Cauley JA, Chalhoub D, Kassem A M (2014) Geographic and ethnic disparities in osteoporotic fractures. Nat Rev Endocrinol 10: 338-351.
- Zhang C, Feng J, Wang S (2020) Incidence of and trends in hip fracture among adults in urban China: A nationwide retrospective cohort study. PLoS Med 17: e1003180.
- Bliuc D, Nguyen ND, Milch VE (2009) Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA 301: 513-521.
- Heit JA (2015) Epidemiology of venous thromboembolism. Nat Rev Cardiol 12: 464-474.
- Brill A, Fuchs TA, Chauhan AK (2011) von Willebrand factor-mediated platelet adhesion is critical for deep vein thrombosis in mouse models. Blood 117: 1400-1407.
- Tang Y, Wang K, Shi Z (2017) A RCT study of Rivaroxaban, low-molecular-weight heparin, and sequential medication regimens for the prevention of venous thrombosis after internal fixation of hip fracture. Biomed Pharmacother 92: 982-988.
- Taoka T, Ohmori T, Kanazawa T (2023) Delayed surgery after hip fracture affects the incidence of venous thromboembolism. J Orthop Surg Res 18: 630.
- Zhang BF, Wei X, Huang H (2015) Deep vein thrombosis in bilateral lower extremities after hip fracture: a retrospective study of 463 patients. Clin Interv Aging13: 681-689.
- Guan C, Ma F, Chang S (2023) Interpretable machine learning models for predicting venous thromboembolism in the intensive care unit: an analysis based on data from 207 centers. Crit Care 27: 406.
- Moons KG, de Groot JA, Bouwmeester W (2014) Critical appraisal and data extraction for systematic reviews of prediction modelling studies: the CHARMS checklist. PLoS Med 11: e1001744.
- Debray TP, Damen JA, Snell KI (2017) A guide to systematic review and meta-analysis of prediction model performance. BMJ 356: i6460.
- Guyatt GH, Oxman AD, Vist GE (2008) GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ 336: 924-926.
- Moons K, Wolff RF, Riley RD (2019) PROBAST: A Tool to Assess Risk of Bias and Applicability of Prediction Model Studies: Explanation and Elaboration. Ann Intern Med 170: W1-W33.
- Yao W, Tang WY, Wang W (2023) Development and validation of preoperative proximal and distal lower limb deep vein thrombosis nomograms in geriatric hip fracture patients. Eur Rev Med Pharmacol Sci 27: 10269-10283.
- Xing F, Li L, Long Y (2018) prevalence of deep vein thrombosis in elderly Chinese patients with hip fracture and a new predictor based on risk factors for thrombosis screening. BMC Musculoskeletal Disorders 19.
- Zhang L, He M, Jia W (2022) Analysis of high-risk factors for preoperative DVT in elderly patients with simple hip fractures and construction of a nomogram prediction model. BMC Musculoskelet Disord 23: 441.
- Ye L, Xuan T, Cong W (2021) Risk factors analysis and model prediction of deep venous thrombosis after treatment in elderly patients with hip fracture. Journal of Vascular and endovascular Surgery 7: 909-913.
- Peng J, Wang H, Zhang L (2021) Construction and efficiency analysis of prediction model for venous thromboembolism risk in the elderly after hip fracture. Zhong Nan Da Xue Xue Bao Yi Xue Ban 46: 142-148.
- Wang X, Jiang Z, Li Y (2022) Prevalence of preoperative Deep Venous Thrombosis (DVT) following elderly intertrochanteric fractures and development of a risk prediction model. BMC Musculoskelet Disord 23: 417.
- Yao W, Tang WY, Wang W (2023) Development and validation of preoperative proximal and distal lower limb deep vein thrombosis nomograms in geriatric hip fracture patients. Eur Rev Med Pharmacol Sci 27: 10269-10283.
- Steyerberg EW, Harrell FJ, Borsboom GJ (2001) Internal validation of predictive models: efficiency of some procedures for logistic regression analysis. J Clin Epidemiol 54: 774-781.
- Yao W, Tang W, Wang W (2022) Association between hyperglycemia on admission and preoperative deep venous thrombosis in patients with femoral neck fractures. BMC Musculoskeletal Disorders 23.
- Xing F, Li L, Long Y (2018) Admission prevalence of deep vein thrombosis in elderly Chinese patients with hip fracture and a new predictor based on risk factors for thrombosis screening. BMC Musculoskeletal Disorders 19.
- Han S, Bai Y, Jiao K (2023) Development and validation of a newly developed nomogram for predicting the risk of deep vein thrombosis after surgery for lower limb fractures in elderly patients. Frontiers in Surgery 10:095505.
- Schaefer JK, Jacobs B, Wakefield TW (2017) New biomarkers and imaging approaches for the diagnosis of deep venous thrombosis. Curr Opin Hematol 24: 274-281.
- Han J, Yang L, Lou Z (2023) Association between Systemic Immune-Inflammation Index and Systemic Inflammation Response Index and Outcomes of Acute Ischemic Stroke: A Systematic Review and Meta-Analysis. Ann Indian Acad Neurol 26: 655-662.
- Huang T, Peng Q, Zhang Y (2024) The Systemic Immune-Inflammation Index (SII) and coronary artery lesions in Kawasaki disease. Clin Exp Med 24: 4.
- Huang T, Peng Q, Zhang Y (2024) The Systemic Immune-Inflammation Index (SII) and coronary artery lesions in Kawasaki disease. Clin Exp Med 24: 4.
- Zeng G, Li X, Li W (2023) A nomogram model based on the combination of the systemic immune-inflammation index, body mass index, and neutrophil/lymphocyte ratio to predict the risk of preoperative deep venous thrombosis in elderly patients with intertrochanteric femoral fracture: a retrospective cohort study. Journal of Orthopaedic Surgery and Research 18.
- Chen X, Fan Y, Tu H (2024) A nomogram model based on the systemic immune-inflammation index to predict the risk of venous thromboembolism in elderly patients after hip fracture: A retrospective cohort study. Heliyon 10: e28389.
- Bo R, Chen X, Zheng X (2024) A Nomogram Model to Predict Deep Vein Thrombosis Risk After Surgery in Patients with Hip Fractures. Indian Journal of Orthopaedics 58: 151-161.
- Xian Mei X (2023) Construction and efficacy evaluation of preoperative prediction model of deep vein thrombosis after hip fracture in elderly patients. Guangzhou University of Traditional Chinese MedicineOsteomatology of traditional Chinese medicine.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.