Retrospective Study of Cephalic Vein Cutdown Technique of Chemoport Insertion: Our Experience at Sawai Man Singh Hospital, Jaipur in 23 Cases
by by Kumar P1*, Sinha S2, Swain P K3, Bhalgat B S4, Lakhera K K5
1 Department of surgical oncology, All India Institute of Medical Science, Patna, India.
2 Dept of obstetrics and gynecology, North Bengal Medical College & Hospital, Siliguri, India.
3 Department of surgical oncology, All India Institute of Medical Science, Bhubaneswar, India.
4 Department of surgical oncology, Shahyadri hospital, Pune, India.
5 Department of surgical oncology, SMS Hospital, Jaipur, India.
*Corresponding author: Kumar P, Department of surgical oncology, All India Institute of Medical Science, Patna, India.
Received Date: 13 September, 2024
Accepted Date: 23 September, 2024
Published Date: 25 September, 2024
Citation: Kumar P, Sinha S, Swain P K, Bhalgat B S, Lakhera K K (2024) Retrospective study of: Our experience at Sawai Man Singh Hospital, Jaipur in 23 cases. J Oncol Res Ther 9: 10248. https://doi.org/10.29011/2574-710X.10248.
Abstract
There are various approaches for chemoport insertion. Most commonly used approach is internal jugular vein followed by subclavian vein. Cephalic vein cutdown technique is relatively easy, cost-effective technique as it doesn’t require any specialized equipment like percutaneous vascular kits, tunnelling instruments and intraoperative USG. Chemoport insertion can be done for various cancer like breast cancer, colorectal cancer, ovarian carcinoma, lymphoma, leukaemia etc for delivering either neoadjuvant or adjuvant chemotherapy.
In this study, we performed cephalic vein cutdown for the patients of breast cancer from August 2021 to February 2022 in surgical oncology department of Sawai Man Singh Hospital, Jaipur, India. These patients were either planned for neoadjuvant chemotherapy or adjuvant chemotherapy through chemoport.
The result of this study is remarkable. In this study, hematoma and abscess were found in 4.34% while retrograde entry of chemoport tip into axillary vein was found in 8.69% of patients.
This study demonstrates that cephalic vein cut down technique for chemoport insertion is safe, feasible and effective technique as compared to internal jugular vein or subclavian vein cannulation which can be performed in less resources set up.
Keywords: Cephalic; Chemoport; Subclavian; Internal Jugular.
Introduction
Adequate vascular access is of paramount importance in oncology patients [1]. There are various venous approaches available for chemoport insertion. Most commonly used vein for chemoport insertion are subclavian vein and internal jugular vein [2]. With the introduction of totally implantable devices for intermittent venous access, commonly known as chemoport have improved the quality of life for patients receiving long term chemotherapy
[3]. Chemoport insertion can be done for various cancer like breast cancer, colorectal cancer, ovarian carcinoma, lymphoma, leukaemia etc for delivering either neoadjuvant or adjuvant chemotherapy. Techniques for external cannulation of the subclavian and internal jugular veins were described by Broviac and Hickman in the 1970s. In 1982, Niederhuber et al. introduced the totally implantable access port [4].
In 1980s,the cephalic vein cut down technique was initially described for placement of pacemakers and later cephalic vein is used for insertion of chemoports. Cephalic vein cutdown technique has advantage over internal jugular or subclavian vein chemoport insertion that whole procedure is carried under vision. There is no requirement of USG guidance or carried out blindly. This technique avoids the attempt of multiple puncture to cannulate into the vein (if carried out through blind technique) and so injury to apex of lung and so avoids the risk of complication of pneumothorax. But no technique is flawless.This technique of Cephalic vein chemoport insertion is also associated with some disadvantages and various complications.
Our department (surgical oncology), SMS Jaipur started chemoport insertion in cephalic vein mainly in patients with breast carcinoma because of ease of this technique. This study was done with the aim to observe the ease of chemoport insertion through the cephalic vein, and the ease and difficulties of the nursing personnel in accessing the chemoports.
Patients and Methods
All patients with breast cancer presenting to Sawai Man Singh Hospital, Jaipur between August 2021 to February, 2022 were included in this retroospective observational study for chemoport insertion in cephalic vein who gave informed written consent. These patients were either planned for neoadjuvant chemotherapy or adjuvant chemotherapy through chemoport. Those patients with second time chemoport insertion after failure or removal of previously inserted chemoport were excluded from study. All the demographic details of patients were entered into database and these patients were followed in surgical oncology unit regarding locating and easily accessing the chemoport hub.
Chemoport Insertion Technique
All the chemoports were inserted as a daycare procedure under local anaesthesia for those patients who were planned for neoadjuvant chemotherapy and during the surgery of primary cancer under general anaesthesia for those patients who were planned for adjuvant chemotherapy. Size of chemoport selected for insertion were of 8F of BARD company which were MRI compatible.
Cephalic vein was the vein of choice for chemoport insertion except in patients with truncal obesity where localizing the cephalic vein was difficult. The side of vein selected was contralateral to the side of pathology. After insertion of chemoport, tip of chemoport was confirmed with C-arm or underwent chest x-ray PA view as per protocol.
Chemoport Insertion Method
Patient was laid in supine position. Procedure was carried out under local anesthesia ( for those patients undergoing neoadjuvant therapy ) or under general anesthesia ( for those planned for adjuvant chemotherapy). After proper prepping and draping, incision was given over delto-pectoral groove. Subcutaneous tissue was dissected. Cephalic vein was identified lying lateral to lateral border of pectoralis major muscle (Fig.1). Cephalic vein is ligated distally and venotomy is done proximal to it. Through the venotomy, chemoport tube is inserted proximally (Fig.2). Measurement of length of tube is taken from planned chemoport chamber placement site to 2nd intercostal space. Subcutaneous pocket was created after raising inferior flap at incision site under which chamber is placed. Chamber is fixed at three points. Then incision site is sutured (Fig.3). Position of tube in vein is confirmed by aspirating blood in heparinized syringe. Tip of chemoport catheter is confirmed with intra-operative C-arm machine or postoperative chest x ray.
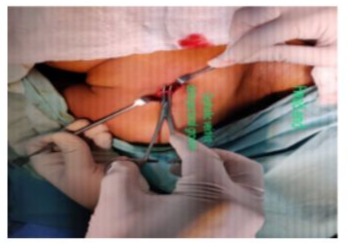
Figure 1: Showing identification of cephalic vein in delto-pectoral groove.

Figure 2: Showing insertion of chemo port catheter into cephalic vein proximally.

Figure 3: Showing sutured incision site.

Figure 4: Showing position of tip of catheter into superior vena cava.
Results
All 23 patients included in this study were patients suffering from breast cancer. Out of 23 patients, 2 were male, rest were female. Maximum age of patient was 76 while that of minimum was 33 with mean age being 54.52 for female and 62 for male. Maximum patients belong to the age group of 51-60 years [Table 1]. All patients were suffering from breast cancer. In all 23 patients, cephalic vein cannulation was successfully attempted. There were good calibre cephalic vein in all patients. There were no obliterated vein or absent vein or small lumen vein (<3mm). Mean duration of surgery was 49.9 min ( median 47, ranges from 30 min to 80 min).
Complications developed during chemoport insertion are shown in Table 2. One patient developed post-operative hematoma which was managed conservatively using aspiration and pressure bandaging. One patient developed abscess formation due to malpositioning of huber needle causing extravasation of chemotherapeutic drug which was managed by incision and drainage of abscess and removal of chemoport. Fortunately, this complication developed after the injection of last dose of chemotherapeutic drug. Tip of port was retrogradely directed into axillary vein instead of subclavian vein was found in 2 patients (Fig.5). We were unable to cannulate the hub of chemoport in one patient due to her obesity. None of patient developed post-operative oedema or shoulder pain. There was no any patient who required repositioning of tube.

Figure 5: Showing tip of catheter retrogradely directed into axillary vein.
|
Age |
Frequency |
|
31-40 |
1 |
|
41-50 |
7 |
|
51-60 |
8 |
|
61-70 |
5 |
|
71-80 |
2 |
Table 1: Showing frequency of patients according to age.
|
Complications |
Number of patients |
Percentage(%) |
|
Hematoma |
1 |
4.34 |
|
Abscess |
1 |
4.34 |
|
Retrograde entry of chemoport into axillary vein |
2 |
8.69 |
|
Post-operative edema |
0 |
0 |
|
Shoulder pain |
0 |
0 |
|
Inability to cannulate |
1 |
4.34 |
Table 2: Showing complications of chemoport insertion.
Discussion
There are several approaches for chemoport insertion in cancer patients. Cephalic vein chemoport insertion is a good alternative to internal jugular/subclavian vein chemoport insertion because it is safe without any added high risk complications. In cancer patients, central venous access devices were first introduced in 1982 [5] to decrease complications (thrombophlebitis, edema) associated with frequent venous cannulation during chemotherapy. While the USG guided chemoport insertion in IJV is practiced at most centres as it is safe and associated with less complications, but it requires expert surgeon. Also this approach requires specialized and expensive instruments including portable ultrasound machine which render its clinical application in small volume centre. Subclavian vein approach of chemoport insertion without USG is associated with life-threatening complications such as hemothorax, pneumothorax, mediastinal hematoma, vascular perforation etc [6]. Therefore we started to perform cephalic vein cutdown for chemoport insertion due to its cost effectiveness, less expertise and less complications [7]. Several studies have shown that immediate fatal complications, including pneumothorax and arterial puncture can be avoided in the cephalic vein approach [8,9].
In our study, all the procedures were carried out by single oncosurgeon, which is contrary to study by Rhu, Jiyoung et al where this procedures were carried out by several general surgeons [10]. This may lead to inter-operator variation and reporting biases. In this study, we were unable to cannulate cephalic vein in 4.34% of cases which is superior to previous studies in which it was ranging from 12%-20% [11-13]. One patient (4.34%) developed post-operative hematoma in this study which is lower than the study done by Mathews et al where post-operative hematoma was found in 3 cases (10%) while there was no reported postoperative infection (abscess) in the same study as compared to our study where one patient (4.34%) developed delayed postoperative abscess at chamber site due to extravasation of drug.3 In two (8.69%) patients, tip of chemoport was directed distally (retrograde) into the axillary vein while Koketsu et al reported the same finding in two (2.53%) cases [14]. None of patient developed post-operative edema or shoulder pain in our study while shoulder pain was reported in 14 cases (46%) in study by Mathews et al [3].
Conclusions
This study demonstrates that cephalic vein cut down technique for chemoport insertion is safe and effective technique as compared to internal jugular vein or subclavian vein cannulation which can be performed in less resources set up. It is associated with less complications. In addition, this approach doesn’t require any specialized equipment, like percutaneous vascular kits, tunnelling instruments, and intraoperative USG.
Conflict of Interest
The authors have no conflict of interest.
References
- Gallieni M, Pittiruti M, Biffi R (2008) Vascular access in oncology patients. CA Cancer J Clin 58:323-46.
- Hyoung Ran Kim, T Hong, Keun Ho Lee, Se Jung Oh, Seung-Man Park et al. (2008) Chemoport Insertion using Cephalic Vein. Journal of The Korean Surgical Society 75:421-424.
- Mathews J, Abraham S, Philip R (2018) “Cephalic vein cut down technique for chemoport implantantion and ease of chemoport access - A cohort study.” Archives of International Surgery 8: 113 - 118.
- Zerati AE, Wolosker N, Luccia ND, Puech-Leão P (2017) Cateteres venosos totalmente implantáveis: histórico, técnica de implante e complicações. J Vasc Bras 16:128-139.
- Niederhuber JE, Ensminger W, Gyves JW, Liepman M, Doan K, et al. (1982) Totally implanted venous and arterial access system to replace external catheters in cancer treatment. Surgery 4:706-12.
- Karakitsos D, Labropoulos N, Groot ED, Patrianakos AP, Kouraklis G, et al. (2006) Real-time ultrasound-guided catheterisation of the internal jugular vein: a prospective comparison with the landmark technique in critical care patients. Crit Care 10:R162.
- Carlo ID, Pulvirenti E, Mannino M, Toro A (2010) Increased use of percutaneous technique for totally implantable venous access devices. Is it real progress? A 27-year comprehensive review on early complications. Ann Surg Oncol 17:1649-56.
- Otsubo R, Hatachi T, Shibata K, Yoshida T, Watanabe H, et al. (2016) Evaluation of totally implantable central venous access devices with the cephalic vein cut-down approach: Usefulness of preoperative ultrasonography. J Surg Oncol 113:114-9.
- Carlo ID, Cordio S, Greca GL, Privitera G, Russello D, et al. (2001) Totally implantable venous access devices implanted surgically: a retrospective study on early and late complications. Arch Surg 136:1050-3.
- Rhu J, Jun KW, Song BJ, Sung K, Cho J (2019) Cephalic vein approach for the implantable central venous access: A retrospective review of the single institution’s experiences; Cohort Study. Medicine 98:e18007.
- Hsu CCT, Kwan GNC, Evans-Barns H, Rophael JA, van Driel ML (2016) Venous cutdown versus the Seldinger technique for placement of totally implantable venous access ports. Cochrane Database Syst Rev 2016:CD008942.
- Povoski SP (2000) A prospective analysis of the cephalic vein cutdown approach for chronic indwelling central venous access in 100 consecutive cancer patients. Ann Surg Oncol 7:496-502.
- Chang HM, Hsieh CB, Hsieh HF, Chen TW, Chen CJ, et al. (2006) An alternative technique for totally implantable central venous access devices. A retrospective study of 1311 cases. Eur J Surg Oncol 32:903.
- Koketsu S, Samesima S, Yoneyama S, Okada T, Tomozawa S, et al. (2010) Outcome of cephalic vein cut-down approach: A safe and feasible approach for totally implantable venous access device placement. Oncol Lett 1:1029-1031.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.