RESET Therapy and ICU Restraint-Induced Psychosis: A Case Report George Lindenfeld
by Diplomate in Clinical Psychology, USA
*Corresponding author: George Lindenfeld, Diplomate in Clinical Psychology, USA
Received Date: 03 February 2026
Accepted Date: 09 February, 2025
Published Date: 12 February, 2026
Citation: Lindenfeld G (2026) RESET Therapy and ICU Restraint-Induced Psychosis: A Case Report. Int J Nurs Health Care Res 9:1696. https://doi.org/10.29011/2688-9501.101696
Abstract
The author has explored the remediative effects of RESET Therapy (RT) (Reconsolidation Enhancement by Stimulation of Emotional Triggers) across various psychiatric conditions, such as Body Dysmorphic Disorder, trauma-afflicted first responders, and combat veterans with PTSD. This article shifts focus to the intensive care setting, where the use of restraints induced a psychotic episode in a previously treated psychotherapy patient. A case report is presented of a patient who, in 2022, following two psychotherapy sessions, demonstrated a positive response to RESET Therapy, using the BAUD (Bio-Acoustical Utilization Device) to access cortical circuitry and achieve a normative, resilient state. A follow-up appointment was requested four years later due to his incurring an ICU restraintinduced trauma resulting in a psychotic episode. This patient’s background involved restraining individuals in the course of his duties as a probation officer throughout his career. As described in the article, he found himself unwillingly restrained in a medical facility following a surgical procedure. This induced a brief psychotic experience lasting around two months. RT, using a recently developed app called Resolve-It! also altered this disruptive state after two treatment sessions, rapidly re-establishing his prior level of cognitive function and resilience. In essence, the RT approach is based on the effects that binaural sound has on cortical circuitry via sensory mechanisms, particularly when paired with emotionally salient stimuli. A thorough description of the treatment process, including the use of the ideomotor response (pendulum) via subconscious muscle movement to identify specific trauma triggers and trauma release sound frequencies, is provided.
Keywords: BAUD (Bio-Acoustical Utilization Device); Ideomotor response; Memory reconsolidation; Reset therapy; Resolve-It! Restraint-Induced Psychosis
Introduction
RESET Therapy (RT) (Reconsolidation Enhancement by Stimulation of Emotional Triggers) is a remediate treatment approach that couples resonating binaural sound with sensory perceptions to alter the reconsolidation of targeted trauma memories. By using binaural sound frequencies that produce a binaural beat, the procedure blocks the hyperarousal emotional and somatic memories of trauma from being reconsolidated into longterm memory. Within the treatment context, memory is selectively triggered in emotion-sensitive brain regions, such as the amygdala and hypothalamus, by the patient’s intentional focus [1].
In contrast with cognitive-behavioural approaches, the use of sensory-based stimuli has demonstrated efficacy in positively addressing trauma-induced consequences. This type of approach addresses the physiological, bodily storage of traumatic stress, rather than relying solely on cognitive processing [2]. As in other sensory-based approaches, a primary principle of RT is that the user must experience the trauma at a sensory/feeling level. Identifying the sound frequency that resonates with the target emotion, akin to a tuning fork, is a primary goal. Once this is accomplished, the secondary goal is to identify the effective binaural sound offset that neutralizes the triggering experience. For example, a frequency of 150 Hz may elicit a maximal pendulum-ideomotor response, followed by a release setting at 157 Hz to establish an effective binaural beat that mitigates trauma-related experiences.
The aim of this treatment approach is to identify a resonant frequency that aligns with (resonates) the disruptive memory. Within this context, change is perceived as a profound sensory shift that restores brain circuitry to a prior state of homeostasis. A distinctive feature of RT is that, because it is non-verbal, the participant is spared the shame and vulnerability associated with potentially embarrassing self-disclosure. Similarly, the therapist is less disposed to develop secondary features of PTSD due to frequent exposure to traumatic material [3]. While still considered investigational, RT therapy is rapid in its effects, requiring fewer treatment sessions than conventional psychotherapies.
Foundational Pillars
The core element of RT derives from findings reported around 2000 that disrupting memory reconsolidation can alter long-term emotional memories [4]. RT is considered a transformational method, positing that traumatic memory circuits have unique frequencies distinct from those of hippocampus-dependent normal memory circuits. In contrast, traumatic memories are processed and stored differently in the brain, often bypassing the areas responsible for autobiographical memory storage. Instead of being integrated into the hippocampus, traumatic memories often become trapped in deeper, emotional, or fragmented regions, such as the amygdala and posterior cingulate cortex [5]. Therapeutic transformational methods aim for profound, lasting change by altering the root causes of emotional, behavioural, and cognitive issues rather than just managing symptoms. The approach rewrites subconscious beliefs, reconstructs past experiences, and fosters somatic awareness to achieve rapid, often permanent therapeutic breakthroughs [6].
Three columns of neuro-scientific information form the foundation for RT Therapy.
Nader and associates’ contributions form the first crucial column. They report that: “New memories are initially labile and sensitive to disruption before being consolidated into stable long-term memories” [7]. Their findings propose that whenever a fear memory is re-energized, it is re-established (reconsolidated or restored) primarily in the amygdala and hippocampus.
One might imagine these brain regions as being comparable to a locked storage vault for long-term, emotionally charged, traumatic memories. The transformative approach prominent in LeDoux’s work [8] is that the fear memory can be effectively ‘erased’ from stored memory. The content feature of the disturbing memory remains, but the strong emotional component is lost once the memory has been reconsolidated. According to these researchers, transformational methodologies involve several naturalistic steps that comprise the change process, including the brain’s unlearning and eradication of a targeted traumatic component of memory.
The required steps include
A: The index trauma must be re-energized by using relevant cues.
B: There must be a disparity that is at odds with the subject’s inherent non-verbal understanding of how the world works. With RT, the mismatch is produced by identifying unique sound frequencies that activate memory circuits, rendering them labile and susceptible to new learning.
C: There is a window of vulnerability of approximately 5 hours before the memory synapses relock to store the newly reconsolidated material [9].
The second support pillar concerns the development of a batterypowered, binaural sound generator, credited to Dr. Frank Lawlis called the Bio-Acoustical Utilization Device [10], that is capable of producing a selective binaural beat that serves as the vehicle for change. Once the selected frequency has been established, an offset frequency (binaural beat) is adjusted until it subjectively causes the target-related sensations to fade, diminish, or disappear.

Figure 1: Bio-Acoustical Utilization Device (BAUD).
The final pillar is based on the pioneering work by Lindenfeld et al., who found that unique sounds can serve as an effective ‘key’ to temporarily disengage and alter the stored emotional aspects of the hippocampal-based memory storage system [11]. The exploratory development and release of both iPhone and Android versions of RT, called Resolve-It! expands access and affordability to a vast array of potential users. Thus, the ability of those with trauma induced conditions to experience an affordable binaural-soundbased treatment through personal or telehealth means becomes a distinct and unique possibility. Furthermore, it enhances patients’ access to self-sustaining remediation over time and distance, thereby improving their potential for mental health improvement. Specifically, Resolve-It! is a binaural sound generator used to remediate, control, and reduce a range of emotional or physiologically based difficulties.
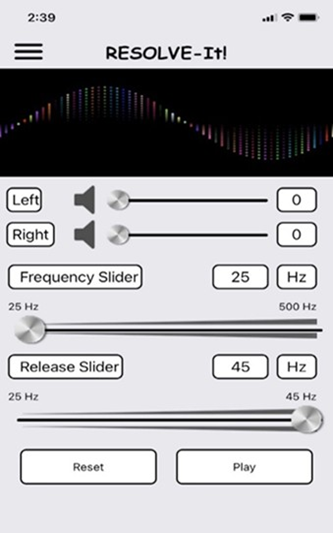
Figure 2: Resolve-It! App.
The Resolve-It! application is designed to use independent volume controls and sound generators for each ear. The volume control sliders are measured in decibels (dB), ranging from 0 to 100. The sound intensity depends on the volume control level that the iPhone or Android is set to. In contrast, the left ear frequency slider ranges from 25 to 500 Hertz (Hz). The secondary right-ear frequency slider resets to the frequency selected in the left-ear slider, then adds an additional range of 20 Hz. For example, if a frequency of 380 Hz is identified in the left ear, the secondary range in the right ear will extend from 380 to 400 Hz. When the frequency and offset settings are correctly identified by the treating therapist or trained patient, a rhythmic pulsating sound will be noticeable midway in the mind called the resonant frequency/binaural beat.
Pendulum: The pendulum is a weighted object, such as a crystal of some type, suspended from a chain. When held between the thumb and index finger, it can swing in different directions in response to inquiries. The movement results from subconscious regions of the mind that influence nerve endings, thereby causing the pendulum to move. This reaction is known as the ideomotor response, wherein involuntary muscle reactions occur. The pendulum magnifies these subtle signals from the subconscious mind, making them visible and easy to interpret.

Figure 1: Crystal Pendulum.
Historically, pendulums have been associated with Ouija boards and consequently carry a negative cultural reputation as being a gateway to undesirable or dark presences. Many people express fear of using them. Within the context of RT Therapy, the traumatriggered pendulum has demonstrated high levels of sensitivity in the identification of binaural frequencies that underlie the existing trauma. Patients may elect to use this approach. Alternatively, they may choose a subjective approach based on their conscious sensitivity to sound frequency.
Case Report
Incident One
Ronnie is an 80-year-old married male whose career was as a New York State Probation Officer on a warrant squad, arresting individuals who violated their legal conditions. “All I did was to restrain offenders and make arrests day and night over thirtytwo years.” Specifically, a warrant squad is a specialized law enforcement unit that focuses on locating and arresting individuals with outstanding arrest warrants, including fugitives and those who failed to appear in court. These teams often employ undercover surveillance and operate across jurisdictions to execute warrants, including arrest, felony, and probation-violation warrants. Warrant service is considered a high-risk police assignment due to the potential for confrontation with desperate, dangerous suspects.
Ronnie initially sought treatment in 2022 due to difficulties he was experiencing with his fifty-six-year-old son, Mark. “He didn’t want anything to do with my wife, Laura. He never listened to what I said. He was diabetic, and didn’t pay any attention to what I told him about diabetes, and how to take care of himself. Laura was basically spearheading it because I felt I had done as much as I could. It was just so agitating to me that I couldn’t lead him on a path to sanity. It was beginning to affect my underlying health issues, like kidney, diabetes, and heart disease, in negative ways.
I remember a time when I was working and Mark, a security guard at a mall, called me to report that his feet were killing him. I said, you probably have stress fractures. You have to go to the foot doctor because your feet are gonna swell, and your feet are gonna look misshapen. So, he calls me up one day and says, ‘Dad, I have to go to a diabetic foot doctor. Will you come with me?’ I said, of course. When he was there, he took off his shoes and socks, and then, shockingly, one of his toes fell off.
I said, Mark, do you see what’s going on here? Do you see what you’re doing to yourself? You’re going to lose parts of your body along the way here. He didn’t pay any attention to me, which was obviously frustrating. But the main thing was that he didn’t want anything to do with Laura, so ultimately, I wrote him out of my will. That was the part that bothered me most because he was my only child. I came in here to talk to you about it because I’m having a hard time keeping my emotions under control because of his behavior.”
Laura added that the main reason why Ronnie sought therapy was that Mark was verbally abusive and that he acted horribly. “He was abusive to his dad. His dad did everything for him. He was his only child. And Mark kept on taking advantage of and treating us like we were garbage. Mark would call his birth mother horrible stuff. And I finally said to Mark, you know what? I don’t respect you at all because of what you call your mother. Your mother does everything for you. And I basically laid it on the line. I don’t like your behavior, and it’s abusive. And I’m not going to tolerate it from you anymore. I set my boundaries.”
At the time (2022), Ronnie was informed of a sound-based intervention called RESET Therapy, which would likely help him bring his emotional reactivity under control. He was shown the BAUD (Bio-Assistance Utilization Device) and agreed to its use at our next scheduled session. The remainder of the initial session was spent illustrating the use of the pendulum for frequency identification purposes. Ronnie was instructed to hold the chainlinked pendulum at about a 30-degree angle, with his elbow firmly resting on an armchair or a similar surface.
Two experiments were advised to help Ronnie understand the pendulum process. After properly positioning the pendulum, he was to politely instruct his subconscious mind, referred to as Mikey (from the cereal ad – Mikey Likes It), to move the pendulum when he silently said his birth mother’s name after first saying two false names. The second experiment used birth dates to initiate pendulum motion. Thus, two false birth dates were initially introduced, followed by the actual birth date. In both instances, a readily recognizable movement occurred when the correct name or date was provided.
Ronnie was informed at our following session that we would first set the Volume Dials of the BAUD to balance the sound in both ears. At Ronnie’s request, the therapist slowly adjusted the volume to a point of balance. Next, Ronnie held the pendulum in his right arm as previously advised. He then activated the sense of frustration he had felt toward his son. The therapist slowly adjusted the BAUD Frequency Dial until the pendulum reached its maximum range of motion.
The final step in the process involved Ronnie asking Mikey to move the pendulum again, once the aggravation had subsided, by adjusting the BAUD Release Dial. Following movement, the pendulum was removed, and the binaural beat was continued for five minutes. During this time, Ronnie’s eyes were closed, and he appeared to be in a state of deep sleep. Following this experience, Ronnie noted that, “all of a sudden, the aggravation was replaced by an image of deer frolicking in a valley eating grass. It was the most restful and peaceful experience I could have imagined that had entered my mind in a long time. It completely replaced any animosity or other feelings related to my son. And even now, every time I think of him, that sight of the deer in the valley comes to my mind.”
Following this experience, Ronnie perceived that his circumstances were like night and day.” It was immediate, as if someone had turned a switch on, then turned it off. It was replaced by this idyllic scene in my brain.” At this point, Ronnie realized his issues with his son had been resolved. He didn’t feel that follow-up care was necessary, and he was consequently discharged with the awareness that further assistance could be provided if indicated.
Incident Two
Four years later (2026), Ronnie’s wife, Laura, contacted this therapist to discuss the feasibility of resuming therapy for her husband. She then assisted him in providing details of his more than two months of prior hospital/rehab experience. Initially, Ronnie underwent a Mental Status Examination provided by the therapist. He appeared to be properly attired, frail, and used a walker for stability. He recognized the therapist and appeared oriented to the current situation. Regarding his attention capacity, he appeared to be somewhat confused. His eye contact was normal, with his speech somewhat pressured. His affect was occasionally labile, with his mood ranging from blandness to anger or anxiety. His thought processes were loose with an underlying content of resentment related to his hospital/rehab experience. His judgement was somewhat impaired, as was his memory of recent events. No risk of self-harm or harm to others was noted. Protective factors included his positive past response to treatment as well as his current help-seeking behavior initiated by his wife.
With the assistance of his wife, the following material was reported. In June of 2025, Ronnie was diagnosed with bladder cancer. “I was in the hospital 11/13/2025-12/4/2025 after they removed my bladder and prostate, and they took a section of my small intestine, made a bladder out of it, and reattached it. I am currently using the previous intestine as a bladder. As a result, I now have incontinence. I’m wearing a diaper, and it’s a very long and embarrassing process of healing.
It was immediate when I became conscious in the hospital following the surgery. I was totally whacked out and struggled to remove the restraints they placed on me. In my mind, I thought that I was the offender and was going to be sent to jail. I didn’t recognize my wife, who was there beside me. I didn’t even know who I was for a long time, like around five days. While there, I sat on a toilet for 30 minutes after pulling the red alarm string and needed help, but no one came. Other issues with the care included my lying in a bed full of urine, and no one came to help me. It really affected me, and I’ve been having nightmares and feeling disconnected ever since.” Ronnie described his sleep as disrupted, rating it an 8 on a 10-point scale, with 10 indicating the worst level possible.
Ronnie experienced a form of stress-induced reaction described as restraint-induced psychosis (RIS). Symptoms of this condition include hallucinations, delusions, and extreme distress. Patients with this diagnosis may experience intense fear, agitation, anger, hostility, and a loss of the concept of time, leading to feelings of detachment or disintegration. Often, the experience is rooted in uncertainty about the situation and a sense of powerlessness. Episodes of this type are often temporary, lasting from a few days to a month. Alternatively, the lasting results can include ongoing psychological distress, nightmares, and a negative impact on the patient-provider relationship.
“So then, I went to rehab because I needed physical therapy. I was still in this other world, and now every morning, I’m waking up in a bed full of urine. I was there for another month. I wasn’t in restraints, but there were times when I had a catheter, and I couldn’t get out of bed. Other times, I got up and found myself tethered to the bed. All of a sudden, once again, I lost control. This whole thing went on for another month. I was pretty much out of it over that time period as well. It was degrading and a total nightmare. It was something that I never expected in my entire life. Finally, Laura took me home despite the nurses’ insistence that I stay there.”
At this point, Laura added that, “Ronnie wasn’t making any progress, and I decided that he would do better in the home setting with some assistance provided there as necessary. I also decided that we needed to start therapy again, as he did so well in the past with your care.”
The therapist described a new app, Resolve-It! developed for the iPhone and Android, which was available at no cost to the user, replacing the previously used BAUD. Aside from the cost aspect, with proper training, the app became available for home use as required, thereby expanding treatment options. Consent was provided by both Ronnie and Laura to proceed with the usage of this therapeutic tool. They were advised to download the app and obtain a headset that provided sound through their phone. Additionally, they were to purchase a pendulum that was approximately the thickness of Ronnie’s thumb.
Ronnie was instructed to hold the therapist’s chain-linked pendulum at about a 30-degree angle, with his elbow firmly resting on an armchair or a similar surface. As provided four years earlier, two experiments were recommended to help Ronnie understand the pendulum’s dynamics. After properly positioning the pendulum, he was instructed to let Mikey (from the cereal ad – Mikey Likes It), subconsciously move the pendulum. He was to politely address Mikey at a three-to-four-year-old level to activate the pendulum when he silently said his birth mother’s name. As instructed, he first soundlessly repeated in his mind two incorrect female names, followed by his birth mother’s name. The second experiment used birth dates to initiate pendulum motion. Thus, two false birth dates were introduced, followed by Ronnie’s actual birth date. In both instances, a readily recognizable movement occurred when the correct name or date of birth was provided. Ronnie was amazed by this outcome.
After obtaining the recommended items listed above, Laura rescheduled the next appointment. Ronnie requested that the therapist adjust the volume controls on Resolve-It! to balance the sound in both of his ears while he held the pendulum in his right arm, as previously advised. When this was accomplished, he activated the frustration he had felt as a result of his hospital/ rehab experience. The therapist slowly adjusted the Resolve-It! Frequency Dial until the pendulum attained its maximum range of motion.
The final step in the process involved Ronnie asking Mikey to move the pendulum once again to a point where the aggravation was reduced by adjusting the Resolve-It! Release Dial. Following the appearance of maximum movement, the pendulum was removed, and the selected binaural beat was continued for ten minutes. Ronnie’s eyes closed, and he appeared to enter a trance-like state over the entirety of the time. After 10 minutes had elapsed, the therapist gently called him back and asked him to recount his experience. Ronnie noted that “the sense of being powerless disappeared into the sound. It was a very peaceful experience. It replaced the hateful feelings from my hospital and rehab time. I can think about the incidents that caused the PTSD and not feel the emotions like I did before. Those feelings are completely gone.
Discussion
Ronnie regained both emotional and cognitive control within the context of a selectively attuned ten-minute binaural beat experience. Following this encounter, he became fully cognizant of his surroundings. Mental status-wise, he appeared to regain full control of his faculties. His underlying sense of powerlessness and disconnection was fully replaced by a sense of intactness and resilience. Theoretically, Ronnie met the reconsolidation conditions elucidated by Nadar and LeDoux [5]. First, the index trauma was re-energized by using relevant restraint-induced sensory cues. Secondly, a mismatch arose due to the use of unique sound frequencies that activated trauma memory circuits, rendering them labile and susceptible to new learning. Finally, a follow-up call revealed that the memory synapses had relocked to store the newly reconsolidated material and accompanying changes within the anticipated five-hour time window.
It is likely that Ronnie’s law enforcement experience as a warrant squad officer sensitized him while under anesthesia to perceive of himself to be restrained as though he were a fugitive with an arrest warrant. His behaviour clearly met the requirements for a diagnosis of Restraint-Induced Psychosis (RIS). Symptom-wise, he experienced delusions, extreme distress, intense fear, agitation, anger, hostility, and a loss of the concept of time, as well as feelings of detachment.
Expanding on this discussion, the RIS condition can be triggered or worsened by the use of physical or mechanical restraints in medical or psychiatric settings. Unfortunately, restraints are intended to manage existing disturbance; however, the restraint experience itself causes additional emotional deterioration. For example, those with a history of physical or sexual abuse, the experience of being restrained can initiate revival of past memories, reactivating traumatic flashbacks.
Separating ICU restraint use from psychiatric facility use, the Price study [12] conducted in 2010, examined the use of physical restraints across European ICUs. The following variables were examined: “physical and chemical restraint use during the weekend and weekdays, reasons for physical restraint use, timing of restraint use, type of restraint used, and availability of restraint policies.” Thirty-four ICUs located in nine countries provided information on 669 patients. Among this population, 1/3 were physically restrained. “Larger units were more likely to use commercial wrist restraints, and smaller units were more likely to have a restraint policy, although these results did not reach significance.” [13].
A recent ICU study conducted in 2025 utilized Neuro Linguistic Programming (NLP), and found that: “close to one in 12 patients hallucinated. Moreover, we demonstrated that almost all such patients developed disturbed behavior, and that patients with hallucinations were much more likely to receive antipsychotic medications.” [11]. Furthermore, a 2022 article [42] explored the use of coercion in intensive care units during the treatment of critically ill patients. Twenty-nine semi-structured interviews with patients and relatives who had been in the ICU a few months earlier were conducted.
“Five main themes emerged: memory issues; interviewees’ experiences of restricting measures and coercive treatment; patients’ negative perception of situational and relational dependency with the risk of informal coercion; patients’ perceptions of good care in a context of perceived dependency; progression from perception of coercion and dependency to respect for the person. All patients were grateful to have survived. However, coercion in the form of restraint, restriction of movement, and coercive treatment in the ICU was also acknowledged by patients and relatives. These included elements of informal coercion beyond restraints, such as a perceived negative sense of dependence, surrender, and asymmetrical interaction between the patient and health providers.”
Although some individuals had RIS symptoms prior to restraint intervention, their intensity often increased during the intervention. The following authors [15] speak to the need for holistic care to better meet ICU participants’ needs.
“The experience of physical restraints during mechanical ventilation in intensive care leads to traumatic experiences which can impact patients and families long after their ICU stay. Holistic care, which considers the physical, emotional and psychological needs of patients and families, should be more thoroughly explored when managing treatment interference to minimize harm.”
Conclusion
The results of this case report support the perspective that properly attuned binaural sound has the capability of rapidly remediating emotional issues, including restraint-induced psychosis. Additionally, the findings from this inquiry support the perspective that the BAUD and Resolve-It! app are compatible within the context of trauma resolution. This is the first direct comparison of these two instruments used on the same patient at different time points. Further comparative testing is clearly indicated in order to substantiate this particular conclusion.
Next, this psychologist recognizes that restraint may indeed be necessary at times in an ICU setting to prevent the onset of selfharm or harm to others. In this context, established guidelines should be closely followed. The primary purpose of this article is to elucidate corrective procedures if or when restraint-induced psychosis should occur. Remediation could potentially be provided by properly trained ICU personnel using Resolve-It! protocols or by adequately trained professionals external to the ICU. Furthermore, the patient and family members could be properly trained to use Resolve-It! within the home setting when necessary to negate further psychotic episodes. This intervention can also be successfully delivered via telehealth.
Funding
This research received no external funding.
Institutional Review Board Statement
This case report is not a formal study.
Informed Consent Statement
The case report participant and spouse approved the submission of this article.
Data Availability Statement
All generated data are available in the article.
Conflicts of Interest
The author declares no conflicts of interest, as the referenced app is currently available at no cost through the Apple Store and Google Play Store. References
- Ecker B, Ticic R, Hulley L (2012) Unlocking the Emotional Brain: Eliminating Symptoms at Their Roots Using Memory Reconsolidation. New York, NY: Routledge.
- Fleming LL, Harnett NG, Ressler KJ, (2024) Sensory alterations in post-traumatic stress disorder, Current Opinion in Neurobiology. Volume 84: 102821.
- Miller Itay MR, Turliuc MN (2023) Who Will Save the Savior? The Relationship between Therapists’ Secondary Traumatic Stress, Secondary Stress Self-Efficacy, and Attitudes toward Trauma-Informed Care. Behavioral Sciences. 13: 1012.
- Sohrabi FMM, Hashemi SE, Mehrabizaheh HM, Bassak NS (2025) Investigating Memory Reconsolidation as a Fundamental Mechanism of Therapeutic Change and a Link Between Neuroscience and Psychotherapy: A Narrative Review. 27 :67-85.
- Clancy KJ, Devignes Q, Ren B, Pollmann Y, Nielsen SR, et al. (2024) Spatiotemporal dynamics of hippocampal-cortical networks underlying the unique phenomenological properties of trauma-related intrusive memories. Molecular Psychiatry. 29:2161-2169.
- Ecker B, Ticic R, Hulley L (2024) Unlocking the emotional brain: Memory reconsolidation and the psychotherapy of transformational change. Routledge.
- Nader K, Schafe GE, Le Doux JE (2025) Fear memories require protein synthesis in the amygdala for reconsolidation after retrieval. Page 6 of 7 Neurol Neurosci. 406:722-726.
- LeDoux J (2003) The Emotional Brain, Fear, and the Amygdala. Cell Mol Neurobiol 23: 727-738.
- Nader K (2015) Reconsolidation and the Dynamic Nature of Memory. Cold Spring Harbor perspectives in biology. 7: a021782.
- Lawlis F (2011) PTSD Breakthrough: The Revolutionary, ScienceBased Compass RESET Program.
- Lindenfeld G, Bruursema LR (2015) Resetting the Fear Switch in PTSD: A Novel Treatment Using Acoustical Neuromodulation to Modify Memory Reconsolidation.
- Benbenbishty J, Adam S, Endacott R, (2010) Physical restraint use in intensive care units across Europe: The PRICE study. Intensive and Critical Care Nursing. 26: 241-245.
- Niccol T, Young M, Holmes NE, Kishore K, Amjad S, et al. (2025) Hallucinations and disturbed behaviour in the critically ill: incidence, patient characteristics, associations, trajectory, and outcomes. Crit Care 29:54.
- Jöbges S, Mouton Dorey C, Porz R et al. (2022) What does coercion in intensive care mean for patients and their relatives? A thematic qualitative study. BMC Med Ethics 23.
- Alostaz Z, Ellis WL, Sangeeta S, Aldalaykeh M, Nasrin Alostaz, N, et al. (2025) Developing a Core Outcome Set and a Core Outcome Measurement Set for Studies Evaluating Interventions to Minimize Physical Restraint Use in Adult Intensive Care Units: Protocol for a Modified Delphi Study. JMIR Research Protocols. 14: e76405.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.