Resection of a Giant Middel Mediastinum Paraganglioma by Clamshell Incision without Cardiopulmonary Bypass
Wivine Piette1, Asmae Belhaj1, Claudia Stanciu Pop2, Benoit Rondelet1,2*
1Department of Cardio-Vascular, Thoracic Surgery and Lung Transplantation, CHU UCL Namur, UCLouvain, Yvoir, Belgium
2Department of Anatomopathology, CHU UCL Namur, UCLouvain, Yvoir, Belgium
*Corresponding author: Benoit Rondelet, Department of Cardio-Vascular and Thoracic Surgery and Transplantation, CHU UCL Namur UCLouvain, Namur Avenue G. Therasse, 1 5530-Yvoir, Belgium
Received Date: 29 December 2022
Accepted Date: 03 January 2023
Published Date: 05 January 2023
Citation: Piette W, Belhaj A, Pop CA, Rondelet B (2023) Resection of a Giant Middel Mediastinum Paraganglioma by Clamshell Incision without Cardiopulmonary Bypass. Ann Case Report. 8: 1117. DOI: https://doi.org/10.29011/2574-7754.101117
Abstract
Paraganglioma is a tumor developed from paraganglia, which are groups of neuroendocrine cells located along the vascular and nerve axes of the head and neck and along the spine. These tumors are benign and still localized in more than 80% of cases.
Middle mediastinal paragangliomas represent less than 1% of mediastinal tumors and grow from the superior or middle mediastinal autonomic ganglion; they mostly are non-functional and are found in older patients. The often large volume and complex location of these tumors make their surgical resection challenging forcing the surgical team to resort to cardiopulmonary bypass and practice transfection of the aortic artery.
We successfully operated an 80-year-old patient by clamshell incision without bypass or arterial procedure.
Keywords: Paraganglioma; Middle mediastinum; Clamshell
Case Presentation
History: An 80-year-old female patient consulted her general practitioner for asthenia, dyspnea, and weight loss. She had a history of high blood pressure, hypothyroidism, and Charcot Marie Tooth disease (lower limb mononeuritis).
The blood tests showed increased inflammatory syndrome, chest X-ray revealed diffuse broncho-emphysematous damage and a central bronchial mass with increased cardio-thoracic index.
Thoracic CT-scan performed afterwards showed an isolated and hypervascularized 68x53mm tumor mass in the middle mediastinum (Figure 1, panels A, B, C). Pulmonary function tests measured an obstructive ventilatory deficit on spirometry: FEV1 of 0.65 liters (36% of predicted values). On plethysmography, significant lung distension was observed, and airway conductance was severely reduced. The 18FDG PET-scan confirmed a large mass in the middle mediastinum, necrotic and hypermetabolic; there was no other focus identified (Figure 1, panels D, E, F).
A diagnosis of Castleman’s disease was retained and the patient was referred to our center for surgical treatment.
Figure 1: Images (A and D: Axial; B and E: Sagittal; C and F: coronal) of Pet (D, E, F)-Scanner (A, B, C) in the mediastinal window (injected): large mass, necrotic and hypermetabolic, in stations 4 (76x58mm, SUVmax 8.2) with some peripheral microcalcifications.
Operating room: After operability assessment, we decided to perform a bloc resection of the tumor. Release of the posterior plane was achieved using a peritracheal mini-approach by video-mediastinoscopy. Then a Clamshell incision (Figure 2) was made to gain full access to both the anterior face of middle mediastinum and the posterior aspect of great vessels and pericardium. Large thoracic vessels (aorta, pulmonary arteries, and superior cava vena) and posterior part of atria were freed over 20 cm length and mobilized to largely dissect the middle mediastinal tumor. We did not transect the aorta nor use cardiopulmonary bypass. Resection of lymph node areas 2, 4 and 10 on the right and 2, 4, 5 and 6 on the left allowed lateral access to the middle mediastinum. The thorax was closed and drained according to the lung transplant protocol in our center.
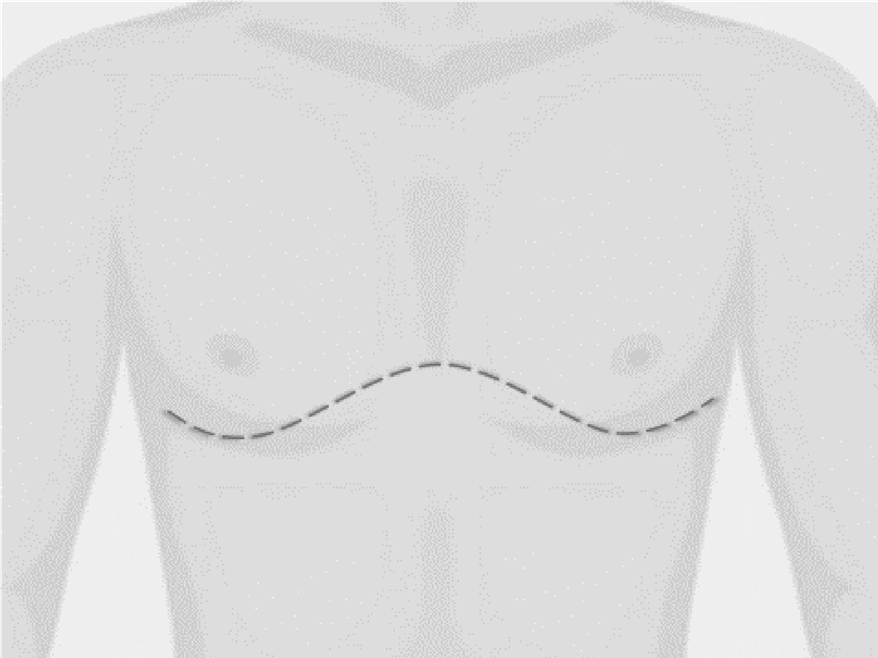
Figure 2: The clamshell incision (also known as a transverse or crossbow transsternal incision) is a combination of a bilateral anterior thoracotomy in the fourth or fifth inter-costal space with an additional transversal sternotomy. It is the rare approach to achieve large exposure and complete resection such as in large space-occupying lesions in the mediastinum.
Pathology: Extemporaneous pathological examination showed a 60 x 60 x 43mm non-hematological tumor mass, finely encapsulated, and completely resected (Figure 3, panel A). The lymph nodes removed showed no metastasis.
The microscopy showed an encapsulated lesion characterized by a proliferation of epithelioid, polygonal tumor cells (Figure 3, panel B). The cells show a uniform distribution, with no significant atypia, with a nesting pattern. Nuclei are round, usually with dispersed chromatin. The supporting stroma is not so abundant; we are seeing some discrete capillary vasculature.
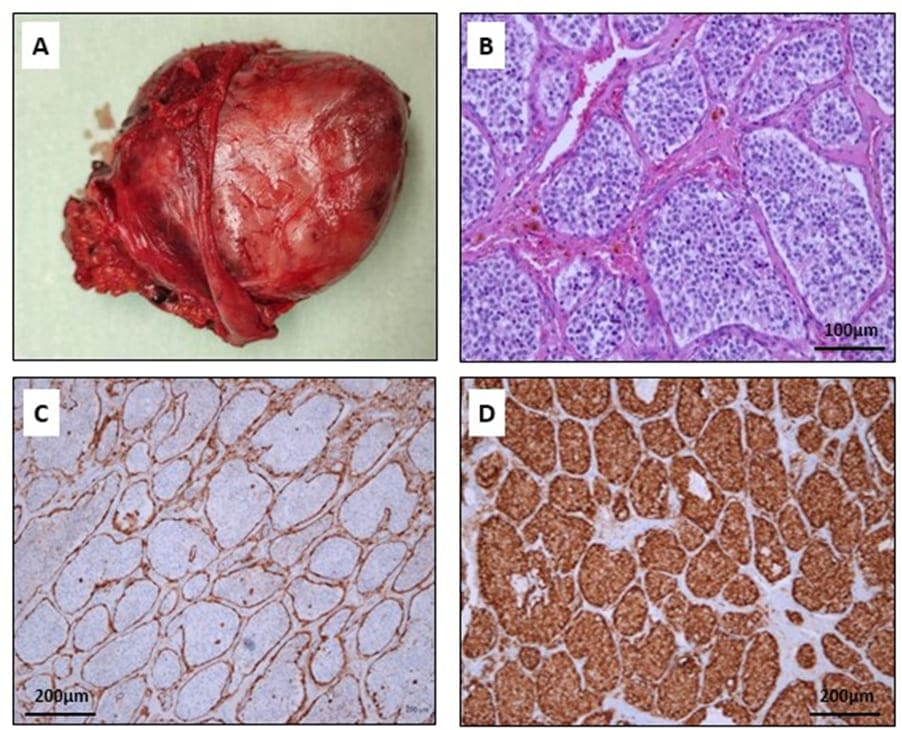
Figure 3: Macroscopic and microscopic findings: A- encapsulated and well-defined tumor; B- Tumoral cells with disposition in nests H.E coloration 20x; C- Immunohistochemical positive stain for Synaptophysin in the tumoral cells 10x; D- Immunohistochemical positive stain for S100 in the sustentacular cells 10x.
In the immunohistochemistry, tumoral cells shows a strong and diffuse staining for synaptophysin (Figure 3, panel C) and chromogranin. GATA3 and cytokeratin are negative. The differential diagnosis is made between a well-differentiated neuroendocrine carcinoma and a paraganglioma. Finally, the S100 protein in immunohistochemistry shows a positive staining (Figure 3, panel D) in the sustentacular cells and the diagnosis of paraganglioma is retained.
Follow-up: The postoperative period was marked by symptomatic atrial fibrillation treated with amiodarone and anticoagulation. The patient was discharged after 10 days without other complication.
After multidisciplinary discussion, endocrine assessment, genetic analysis [search mutations for Succinate Dehydrogenase Complex Flavoprotein (SDH) subunit-A, SDH-B, SDH-C, SDH-D, Von Hippel-Lindau (VHL) and RET genes] and Octreoscan® were performed; all the results were normal.
Three months later, the general status was improved, dyspnea was reduced however the spirometry showed persistent obstructive ventilatory disorder [first second of forced expiration (FEV1) 57% of the predicted values] with discreet restrictive component [forced vital capacity (FVC) 70% of the predicted value]. Increased exhaled Nitric Oxid argued for additional asthma diagnosis. The atrial fibrillation treatment with amiodarone was stopped and the therapeutic anticoagulation continued.
Discussion
Paragangliomas as a rare tumor
The annual incidence of paragangliomas is estimated at 1 per 100,000. These tumors are benign and localized in more than 80% of cases. However, there are malignant forms defined by the presence of tumor cells in neighboring tissues, lymph nodes or metastasis. A paraganglioma is a tumor developed at the expense of paraganglia, which are groups of neuroendocrine cells located along the vascular and nerve axes of the head and neck and along the spine. Paragangliomas can develop in the neck and the lower part of the skull, thorax, abdomen, or small pelvis. Some paragangliomas (3%) secrete hormones, most often catecholamines. These tumors are called functional when these secretions are responsible for clinical symptoms [1, 2].
Twenty to 30% of paragangliomas are hereditary and present in one of the family forms: multiple paraganglioma disease and Von Hippel-Lindau disease. In these familial forms, the paragangliomas are often present on several sites and are recurrent [3-6].
Middle mediastinal paraganglioma is a rare localization
Mediastinal paraganglioma is a rare tumor of the mediastinum (0.3%) and the mediastinum is a rare location of a paraganglioma (1-2%) [1-3, 7]. Mediastinal paragangliomas are mostly located in the posterior part where they arise from the aortic sinus sympathetic ganglion; they are mainly functional and found in younger patients (average age 29 years) [1-2]. Paragangliomas in the anterior mediastinum are often asymptomatic and non-functional but with a poorer prognosis [3]. Middle mediastinal paragangliomas represent less than 1% of mediastinal tumors and grow from the superior or middle mediastinal autonomic ganglion; they are mostly non-functional and found in older patients (mean age 49 years) [2]. Only 3% of paragangliomas secrete catecholamines [12].
Clinical Presentation and Symptoms
The circumstances of discovery are diverse and depend on the functional character (secreting) or not of the tumor. The symptomatology suggestive of a tumor syndrome and can vary according to the seat and the volume of the mass. Sometimes it is a fever, pain, weight loss or lack of appetite, or the discovery of metastasis that will lead to the diagnosis of paraganglioma. Symptoms may also be related to tumor hormone secretion. The secretion of catecholamines (including adrenaline and noradrenaline, dopamine) and their derivatives (metanephrines) by functional paragangliomas will be responsible for arterial hypertension [2, 8-9]. This arterial hypertension can be unstable with paroxysmal attacks. Sometimes it is chronic hypertension that is difficult to balance. It is accompanied by headaches, palpitations, sweating, pallor, chest, or abdominal pain and/or collapse. The tumor can also be discovered incidentally during an imaging examination (scanner, ultrasound) or during surgery for any other condition. Finally, paragangliomas can also be diagnosed during the family assessment of a genetic disease [2-3, 8, 9-14].
Differential diagnosis
The paragangliomas diagnosis and management are complex and require multidisciplinary competences. The diagnosis of paraganglioma is most often made by the analysis of the operative specimen removed during the surgical intervention or during biopsy on the histological aspect of the tumor and on the existence of specific markers such as chromogranin A (which can also be measured in blood) and sometimes synaptophysin [2, 8, 13-14].
Differential diagnosis of middle mediastinum mass is complicated and includes mainly other neuroendocrine tumors but also Castleman’s disease, lymphadenopathy, lymphoma, neurogenic tumors, metastatic disease, granulomatous disease, hemangioma, congenital cyst and angiosarcoma. Precise diagnosis is very complicated without excision of the lesion and immunohistochemical diagnosis [3, 8, 12, 14-15].
The diagnosis of malignancy is based on the demonstration of a relapse or an extension into the lymph nodes, tissues around the primary tumor or extension remote disease in organs such as liver, lung, bone [1-3, 13].
In addition to the analysis of the surgical specimen or the biopsy, several examinations will be carried out, with the aim of specifying tumor location, to look for other paragangliomas and/ or a possible extension, to determine its secreting or not character and look for a hereditary cause. Due to the often-familial nature of this condition, a genetic test is proposed [3, 5, 11, 15].
Pre-treatment assessment
Biological examinations: The most often performed biological test is the measurement of metanephrines in the blood and/or in the urine for 24 hours [1-3, 9, 11-12, 16]; it reflects the secretion of catecholamines. A test for chromogranin a practiced in the blood as well as the verification of the potassium level and the glycemia complete the biological assessment [1, 16].
Imaging exams: Imaging examinations aim to specify both location of the tumor (or tumors) and extension(s) to monitor its evolution [2, 10, 13, 17-18].
On CT-Scan, paragangliomas is a hypervascularized lesion with a rich capillary network. On computed tomography (CT), the typical appearance of a paraganglioma is a mass with an unenhanced density greater than 10 Hounsfield units (HU), avid contrast enhancement, and delayed washout. Sometimes, internal hemorrhage can be seen; cystic changes, necrosis, and internal calcifications are commonly described. Rarely, these masses show low attenuation or minimal enhancement [1, 2, 6-8, 13-14, 16, 18].
Magnetic Resonance Imaging is most often performed and provides a better visualization of the tumor and its anatomical relationship to neighboring organs and vessels. Paraganglioma demonstrate T2 prolongation and variable, although often intense, contrast enhancement. Internal hemorrhage and cystic components contribute to the heterogeneous MRI appearance of these tumors. Additional use of opposed phase imaging can be helpful as paragangliomas do not exhibit dropout of signal on opposed phase imaging, but adenomas do [1, 6, 10, 13, 18].
Nuclear imaging examinations may also be performed. These examinations are generally based on the radiation emitted by a radioactive isotope which is concentrated by the tumor and allows its detection. Firstly, the scintigraphy of the whole body by 123I-MIBG (Meta Iodo Benzyl Guanidine) or the Scintigraphy of the Somatostatin Receptors (SRS), also called Octreoscan®, provide details on the tumor(s), explore the whole body, and participate in the extension assessment [2, 6, 8, 12]. In addition to the interest for the detection of tumors, these scintigraphy examinations assess the importance of the tumor concentration of tracers and the interest of their therapeutic use. Then, the positron emission tomography with 18FDG (PET-FDG), made after the injection of a radioactive product based on glucose, is carried out in addition to the previous examinations and participates in the extension assessment of the disease [3, 6, 8, 12, 18]. Other tracers such as 18F-Dopa are sometimes used. However, it has been shown that the use of PET scan with 68Ga-DOTA-NOC was preferable to 18F-DOPA for the diagnosis as well as for the follow-up of thoracic neuroendocrine lesions because it has a better detection of primary lesions and metastasis [6, 19-20].
Biopsy: Ct-Scan biopsies guided, external ultrasound, EUS (Endoscopic UltraSound), or EBUS (EndoBronchial UltraSound) can help in the preoperative diagnosis of a mediastinal lesion. However, for paraganglioma if the specificity of these procedures is 100%, the sensitivity is limited to 50% [21]. Moreover, for the middle mediastinum tumor, because of the tumors are both close to the great vessels, highly vascularized and at risk of catecholaminergic discharge, biopsy is not recommended.
Currently, the diagnosis of paraganglioma is complicated on a biopsy [3, 8, 16, 19, 22]. It requires a complete structural and morphological pathologic tumor analysis [3, 8].
Histochemical analyzes help to do the differential diagnosis. It is first recommended to look for GATA-3 and TTF-1 markers expressions. Paraganglioma is moreover positive for chromogranin A and synaptophysin but negative for pancytokeratin, TTF-1 and napsin A. GATA-3 is positive in 55% of cases [22].
Treatment
Given the diversity of tumor locations and their great evolutionary heterogeneity, the therapeutic management is adapted to each patient. For functional tumors, the hormonal secretions control must be rapidly efficient because of the risk of cardiac complications and unforeseeable accidents that may be sometimes triggered by the general anesthesia. For these reasons, most paragangliomas are managed in an integrated-care cancer center.
The double objective of the treatment is the hormonal secretions control and tumor control.
To treat the tumor, there are two categories of treatments: First, the local treatments which include surgery, interventional radiology and external radiotherapy, and then the general treatments, including metabolic radiotherapy and chemotherapy [1-3, 7-8, 13, 16, 19, 22, 24-25].
The objective of local treatments is to control the local consequences of the tumor. Impact on disease general control may be important when the treated volume is important.
Surgery: Surgery is the best treatment when the tumor is localized. The main objective is a total resection of the mass with clean margins which gives patient not only a better prognosis and avoids recurrences or malignant degeneration but also constitutes an aid for a best diagnosis and therefore a best management. [13, 8, 10, 12-13, 16, 24-26]. Surgery may also be indicated, on a case-by-case basis, to treat local relapses and/or metastatic [1, 3, 8, 12-13, 16, 25].
In case of functional paraganglioma causing refractory arterial hypertension, and -adrenergic blockers or calcium channel blockers with increase in circulating volume by low molecular weight dextran and a salty diet are useful [1, 3, 13, 25]. Catecholamines synthesis inhibition with Metyrosine can also be established [25]. Surgery may be, by it-self, the source of variations in blood pressure and heart rate linked to a discharge of catecholamines during the resection of the tumor and the cause of significant bleeding given the nature and location of the tumor [1, 3, 12-13, 16, 25].
Significant technical difficulties related to the lesion location and the vascular, respiratory, and nervous structures proximity may be shown. In functional paraganglioma, arteriography with embolization can be performed not only to avoid major intraoperatively bleeding and to reduce catecholaminergic discharges but also to visualize preoperatively the tumor vascularization [3, 13, 16].
The main technique is median sternotomy with or without extracorporeal circulation, circulatory arrest, and hypothermia. Sometimes, a left thoracotomy is also done to improve access to large vessels and control the bleeding. Depending on the locally tumor invasion, an aortic transection may be practiced and the resection of one of more accessory thoracic vessels or the left atrium is sometimes performed with vascular or cardiac reconstruction. In the most often situations, sternotomy allows the mobilization of the aorta, the pulmonary artery, and the main airways to have a good exposure and a secure a bloc resection of the lesion [9, 12, 14, 16, 25-27].
In our case, we performed a clamshell incision, which allowed wide bilateral access, more easy mobilization of the giant lesion from neighboring structures and a control of the large thoracic vessels. This procedure, commonly used by thoracic transplant teams, opened lateral access to the middle mediastinum, to the large thoracic vessels (aorta, pulmonary arteries, and superior cava vena) and the posterior part of left atria and then avoided the use of cardiopulmonary bypass and the transfection of large vessels. Moreover, by this method, the resection of all lymph node areas had been easily possible. However, the size of the lesion may sometimes require vascular or nerve resection. To our knowledge, this surgical plan has never been reported for a giant middle mediastinal paraganglioma [9, 25].
Depending on limited size, favorable location, and obviously free relations, lesion may sometimes be resected with a videoassisted procedure, but it remains, always, significant bleeding or nerve damage risk. Open surgery will often be preferred to offer better control of potential bleeding and to perform a bloc resection with negative margins [3, 12, 16, 18].
Interventional radiology: The main techniques of interventional radiology are embolization, radiofrequency, and cryotherapy. These techniques allow relieve pain and reduce tumor volume. The purpose of embolization is to reduce or interrupt tumor or metastasis blood supply. Metastasis destruction may also be obtained by specific use of guided (CT-Scan or ultrasound) radiofrequency or cryotherapy [3, 13, 16, 25].
External radiotherapy: Radiotherapy has been an established treatment for paraganglioma over many years. However, radiotherapy has often been reserved for failure after surgery or for secondary metastasis, the literature supports the use of radiotherapy as a primary treatment. This has the advantage of avoidance of surgical morbidity, which may be sometimes appreciable, but with the inconvenient that the tumor remains in situ [28].
The goal of systemic treatments is the disease global control. Metabolic radiotherapy and chemotherapy are the classic treatment options. New therapies such as antiangiogenics are also offered within study protocols.
Metabolic radiotherapy: Targeted radionuclide therapies using MIBG and somatostatin analogues as a vehicle for the radioactive agent into the tumor represent several of the therapeutic options in the management of metastatic or inoperable paraganglioma. Metabolic radiotherapy, or “internal radiotherapy” is a method which consists of specifically irradiating the cancerous cells present in various parts of the body. This treatment is only possible for tumors that capture the vehicle, 131I-MIBG or somatostatin analogs. This uptake may be visualized on the scintigraphy [29].
Chemotherapy:
Chemotherapy can be used for palliative treatment of malignant paraganglioma. The purpose of chemotherapy is to slow down, and sometimes even to stop the cancer cells multiplication in untreatable by local treatment techniques [30].
Follow-up
In addition to the already mentioned hemorrhages risk, paraganglioma in the middle mediastinum are also close to structures such as the recurrent laryngeal, vagus, or phrenic nerve that can be injured or sacrificed to perform a complete a bloc resection with clean margins. Respiratory and cardiac complications are also reported [9, 25].
These are mainly benign tumors but with a potential for malignancy (15–35%). There are no long-term deaths in benign paragangliomas [23].
For the malignant forms, the prognosis is better in the event of complete resection with clean margins and in the absence of metastasis. Paragangliomas usually show a poor response to chemotherapy and radiation therapy. In malignant paragangliomas, the prognosis is different depending on the presence of metastasis, the progression rate and the primitive tumor size and its extension to neighboring structures [12].
The criterion for malignancy is the presence of local or distant metastasis. Metastasis are most often located in the lymph nodes, liver, lungs, and bones [2] and 35% are present as synchronous lesions. The tumor recurrence risk is lower in complete surgical resection [12] with a survival rate of 84.6% (125.7 ± 18.7 months). In case of incomplete resection, survival is downed to 50% (71.5 ± 13.8 months) [24].
Regular monitoring will be carried out for several years. The frequency of this monitoring will be adapted to each patient and is based on biological examinations (dosages of hormones, chromogranin A and metanephrines) and imaging (CT, MRI, scintigraphy) which allow to assess the progression of the disease [1, 3, 8, 12].
Half of paragangliomas is linked to a genetic mutation and to certain familial syndromes by autosomal dominant transmission such as mutations in the succinate dehydrogenase (SDHx) genes. A search for genetic mutation is necessary as well as a family screening if a mutation is highlighted. These mutations often lead to multiple, recurrent paragangliomas [4, 5].
Conclusions
Mediastinal paragangliomas are rare but should be considered when a mediastinal lesion shows strong enhancement on the injected CT scan, especially if the biological tests show an abnormal level of catecholamines. These are mostly benign lesions. The treatment of choice is a bloc surgical resection. The paraganglioma presents a certain morbidity and mortality linked to the anatomical relationship of the lesion which generates significant surgical risks and difficulties of resections in negative margins but also linked to the risks of recurrence. In our case, the clamshell incision used here for the first time allowed easy access to the tumor and avoided vascular reconstruction with extracorporeal circulation leading to safe vascular control and complete a bloc resection.
Funding
Benoit RONDELET was supported by grants from the Belgian Fonds de la Recherche Scientifique (FNRS), the Fondation Mont-Godinne (Belgium) and the Fonds Carine Vyghen (Belgium). Asmae BELHAJ was a fellow of the Fondation MontGodinne (Belgium).
References
- Yin YY, Yang B, Ahmed YA, Xin H (2019) Thoracotomy of an asymptomatic, functional, posterior mediastinal paraganglioma: A case report. World journal of clinical cases, 7: 1529-1534.
- Soomro NH, Zahid AB, Zafar AA (2016) Non-functional paraganglioma of the mediastinum. JPMA. The Journal of the Pakistan Medical Association, 66: 609-611.
- De Palma A, Lorusso M, Di Gennaro F, Quercia R, Pizzuto O, et al. (2018) Pulmonary and mediastinal paragangliomas: rare endothoracic malignancies with challenging diagnosis and treatment. Journal of thoracic disease, 10 : 5318-5327.
- Michałowska I, Ćwikła J, Prejbisz A, Kwiatek P, Szperl M, Michalski W, Peczkowska M (2016) Mediastinal paragangliomas related to SDHx gene mutations. Kardiochirurgia i Torakochirurgia Polska, 13: 276-282.
- Ghayee HK, Havekes B, Corssmit EP (2009) Mediastinal paragangliomas: association with mutations in the succinate dehydrogenase genes and aggressive behavior. Endocrine-related Cancer; 16: 291-299.
- Ocazionez D, Shroff GS, Vargas D, Dicks D, Chaturvedi A, et al. (2017). Imaging of Intrathoracic Paragangliomas. Seminars in ultrasound, CT, and MR, 38: 584-593.
- Balcombe J, Torigian DA, Kim W, Miller WT Jr (2007) Cross-sectional imaging of paragangliomas of the aortic body and other thoracic branchiomeric paraganglia. AJR. American journal of roentgenology, 188 : 1054-1058.
- Wald O, Shapira OM, Murar A, Izhar U (2010) Paraganglioma of the mediastinum: challenges in diagnosis and surgical management. Journal of cardiothoracic surgery, 5 : 19.
- Andrade CF, Camargo SM, Zanchet M, Felicetti JC, Cardoso PF (2003) Nonfunctioning paraganglioma of the aortopulmonary window. The Annals of thoracic surgery, 75 : 1950-1951.
- da Silva MCB, Shoji H, Franken M, Shiang C, Garcia RG, et al. (2020). Paraganglioma: An Uncommon Cause of Mediastinal Mass. Cardiovascular imaging, 13 : e009693.
- Young WF Jr (2006). Paragangliomas: clinical overview. Annals of the New York Academy of Sciences, 1073 : 21-29.
- Rahi MS, Gunasekaran K, Amoah K, Rudolph D (2020) Paraganglioma of the middle mediastinum. Respiratory medicine case reports, 31 :
- Zhang B, Liu G, Li J, Wan P (2022) Middle mediastinal paraganglioma enclosing the left anterior descending artery: A case report. Medicine, 101 : e30377.
- Hato T, Kaseda K, Harada M, Horio H (2011) Aorticopulmonary General thoracic and cardiovascular surgery, 59 : 812-814.
- Hsu YR, Torres-Mora J, Kipp BR, Sukov WR, Jenkins SM, Voss JS, et (2019). Clinicopathological, immunophenotypic and genetic studies of mediastinal paragangliomas†. European journal of cardio-thoracic surgery : official journal of the European Association for Cardiothoracic Surgery, 56 : 867-875.
- Miura K, Kobayashi N, Satomi H (2020) Surgical resection of a middle mediastinal paraganglioma that caused diabetes. Surgical case reports, 6 : 241.
- Bourgouin PP, Madan R (2021) Imaging of the Middle and Visceral Radiol Clin North Am; 59: 193-204.
- Cabral FC, Trotman-Dickenson B, Madan R (2015) Hypervascular mediastinal masses: action points for radiologists. European journal of radiology, 84 : 489-498.
- Blanchet EM, Millo C, Martucci V, Maass-Moreno R, Bluemke DA, Pacak K (2014) Integrated whole-body PET/MRI with 18F-FDG,18F-FDOPA, and 18F-FDA in paragangliomas in comparison with PET/CT: NIH first clinical experience with a single-injection, dualmodality imaging protocol. Clinical nuclear medicine, 39 : 243-250.
- Ambrosini V, Tomassetti P, Castellucci P, Campana D, Montini G (2008) Comparison between 68Ga-DOTA-NOC and 18F-DOPA PET for the detection of gastro-entero-pancreatic and lung neuro-endocrine European journal of nuclear medicine and molecular imaging, 35 : 1431-1438.
- Marcus A, Narula N, Kamel MK, Koizumi J, Port JL, Stiles B, Moreira A, Altorki NK, Giorgadze T (2019) Sensitivity and specificity of fine needle aspiration for the diagnosis of mediastinal lesions. Annals of diagnostic pathology, 39 : 69-73.
- Weissferdt A, Kalhor N, Liu H, Rodriguez J, Fujimoto J, Tang X, Wistuba II, Moran CA (2014) Thymic neuroendocrine tumors (paraganglioma and carcinoid tumors): a comparative immunohistochemical study of 46 cases. Human pathology, 45 : 2463-2470.
- Topçu S, Alper A, Gülhan E, Koçyigit O, Tastepe I, Cetin G (2000) Neurogenic tumours of the mediastinum: a report of 60 cases. Canadian respiratory journal, 7 : 261-265.
- Lamy AL, Fradet GJ, Luoma A, Nelems B (1994) Anterior and middle mediastinum paraganglioma: complete resection is the treatment of choice. The Annals of thoracic surgery, 57 : 249-252.
- Paul S, Jain SH, Gallegos RP, Aranki SF, Bueno R (2007) Functional paraganglioma of the middle mediastinum. The Annals of thoracic surgery, 83 : e14-e16.
- Bierler J, Poncelet A, Lacroix V (2021) Aortic transection for resection of middle mediastinal tumor. Acta chirurgica Belgica, 1-4.
- Otake Y, Aoki M, Imamura N, Ishikawa M, Hashimoto K, Fujiyama R (2006) Aortico-pulmonary paraganglioma: case report and Japanese The Japanese journal of thoracic and cardiovascular surgery : official publication of the Japanese Association for Thoracic Surgery = Nihon Kyobu Geka Gakkai zasshi, 54 : 212-216.
- Trombetta M, Silverman J, Colonias A, Lee V, Mohanty A, Parda D (2008) Paraganglioma: a potentially challenging tumor. Oncology (Williston Park); 22: 341-3.
- Jha A, Taïeb D, Carrasquillo JA, Pryma DA, Patel M, Millo C, et al. (2021) High-Specific-Activity-131I-MIBG versus 177Lu-DOTATATE Targeted Radionuclide Therapy for Metastatic Pheochromocytoma and Paraganglioma. Clin Cancer Res; 27: 2989-2995.
- Niemeijer ND, Alblas G, van Hulsteijn LT, Dekkers OM, Corssmit EP (2014) Chemotherapy with cyclophosphamide, vincristine and dacarbazine for malignant paraganglioma and pheochromocytoma: systematic review and meta-analysis. Clin Endocrinol (Oxf); 81: 642
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.