Recurrence of Physeal Bar Formation Following Initial Success of Resection: A Case Report
by Wan Salam WNA1, Mohd EF1, Munajat I1*, Sulaiman AR1, Nur Azutul AK2
1Department of Orthopaedic, Universiti Sains Malaysia, Kubang Kerian, Malaysia
2Department of Orthopaedic, Hospital Tengku Ampuan Afzan Kuantan, Malaysia
*Corresponding author: Munajat I, Department of Orthopaedic, Universiti Sains Malaysia, Kubang Kerian, Malaysia
Received Date: 04 September 2025
Accepted Date: 12 September 2025
Published Date: 15 September 2025
Citation: WNA Wan Salam, Mohd EF, Munajat I, Sulaiman AR, Nur Azutul AK. (2025). Recurrence of Physeal Bar Formation Following Initial Success of Resection: A Case Report. Ann Case Report. 10: 2410. https://doi.org/10.29011/2574-7754.102410
Abstract
Introduction
Managing physeal injury can be challenging, especially when it is complicated by premature growth arrest with physeal bar formation. Physeal injury at distal femur may lead to severe morbidities since it contributes significantly to the longitudinal growth. This case report discussed a paediatric metaphyseal fracture of the distal femur with progressive varus deformity which was successfully managed through physeal bar resection and acute corrective osteotomy, however, represented with recurrent formation of the bone bar after initial success.
Case Report
We presented a polytrauma case of a two-year-old girl with closed left supracondylar femoral fracture following a high-impact motor vehicle accident. She developed a varus deformity in the left distal femur caused by a medial physeal bar two years after the injury which was most likely due to the Salter-Harris type V injury. Medial physeal bar resection, interposition of bone wax and valgus osteotomy were performed. The medial growth of the physis returned. The following year, a lateral physeal bar was formed in the distal physis of the left femur, resulting a valgus deformity. Hence, we proceeded with lateral physeal bar resection and varus corrective osteotomy. Unfortunately, one year later, the medial physeal bar of the distal left femur recurred with varus deformity.
Conclusion
High-energy impact injuries near the physis should be followed up for at least one year to ensure that no associated physeal injury is missed, preventing morbid outcomes from the sequalae of physeal arrest or premature physeal closure. Additionally, we recommend anchoring bone wax packing to prevent proximal migration and recurrence of the bone bridge.
Keywords: Physeal arrest; Physeal bar resection; Epiphysiodesis; Recurrence; Angular deformity
Introduction
Approximately 5-10% of physeal fractures are complicated with growth arrest manifested by length discrepancy or deformity [1]. These fractures are often diagnosed retrospectively following structural deformities caused by premature growth plate closure [1, 2].
Physeal bar resection with growth modulation and corrective osteotomy are among treatment options [1]. We reported a paediatric distal femur metaphyseal fracture complicated with progressive varus deformity successfully managed through physeal bar resection and acute corrective osteotomy. However, she represented with recurrent formation of the bone bar after initial success.
Case Report
This high-impact polytrauma case involved a two-year-old girl who sustained closed left supracondylar femoral fractures, (Figure IA), a brain injury and a right pneumothorax after motor vehicle accident. Closed reduction and transphyseal cross K-wiring of the distal femur were performed (Figure IB). The K-wires were removed 10 months later.
She represented two and a half years later with a progressive varus deformity of the left distal femur (Figure IC). A computed tomography (CT) scan confirmed the formation of a medial physeal bar (Figure ID). At age of five, she underwent medial physeal bar resection with bone wax interposition and valgus osteotomy (Figure IE). The K-wires were removed two months postoperatively.
One year later, the distal physis of the left femur developed a lateral physeal bar, resulting in valgus deformity (Figure IF). A CT scan revealed the formation of a new lateral physeal bar (Figure IG). Therefore, at age of six, a second surgery involving lateral physeal bar resection and varus corrective osteotomy were performed to correct the valgus deformity (Figure II A & IIB).
Within a year, her distal left femur developed varus angulation again, attributed to the recurrence of the medial physeal bar (Figure IIC). A CT scan showed the medial physeal bar recurred with proximal migration of the bone wax (Figure IID).
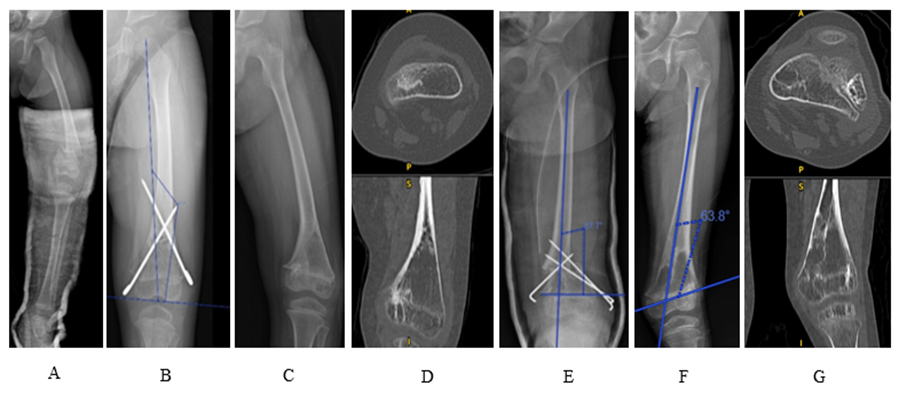
Figure I: A: displaced supracondylar fracture of left femur at age of two. B: left femur was treated with cross K-wires that passed through distal femoral growth plates. C: varus deformity of distal femur with medial physeal bar formation in Sept 2020. D: CT image in Jan 2020 which medial physeal bar identified. E: physeal bar resection followed by corrective osteotomy and fixation with 1.6mm wire performed at the age of 6 (Sept 2020). F: The distal femur became valgus in Dec 2021 (6 years old) to suggest a successful medial physeal bar resection and physeal bar formation on lateral side. G: CT image in Dec 2021 showed a very lateral location of physeal bar.
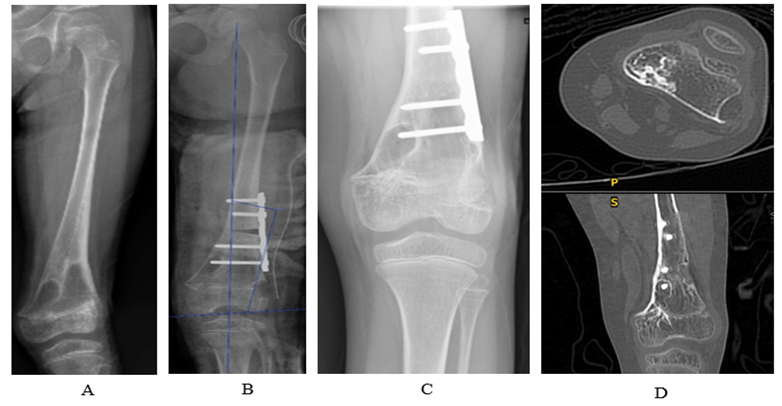
Figure II: A: valgus deformity. B: early radiograph after lateral physeal bar resection and corrective osteotomy. C: successful lateral bar resection with no recurrent of valgus deformity at one year, however varus angulation redevelops. D: CT image of physeal bar reformation medially.
Discussion
The distal femoral physis is the fastest-growing physis contributing 37% of the entire lower limb length and 70% of femoral length [1]. It is associated with a high incidence of growth plate arrest, ranging from 27.3% to 90%, which may result in angular deformity and/or LLD [3]. Younger age, high-energy trauma, fracture configuration, degree and direction of displacement, and transphyseal pinning are factors that may violate the growth plate to varying degree [3].
In our case, plain radiograph of the distal femur revealed a transverse metaphyseal fracture with minimal comminution. It is likely that significant deforming forces were transmitted through the growth plate during the impact due to its proximity to the fracture site. This undetected physeal injury later manifested as incomplete physeal arrest, presenting as a medial physeal bar. Garrett et al. [3] found that high-energy injuries are significantly associated with distal femoral physeal bar formation.
Animal studies demonstrated the potential association between transphyseal pinning with growth disturbance [4]. Size of K-wire, use of threaded wires, location within the physis, obliquity within the physis and duration of K-wire retention are potentially associated with premature physeal closure [4]. In this case, the distal femur fracture was stabilised using cross smooth K-wires, with the medial pin crossing the physis (Figure IB). The number of K-wire insertion attempts depended on the surgeon’s skill. The K-wires were removed 10 months post-operatively. All these factors may have contributed to the formation of the medial physeal bar, resulting in a varus deformity of the distal femur. The patient underwent medial physeal bar resection with bone wax interposition and valgus osteotomy to correct this deformity.
The correction of the distal femur axis indicated a successful medial physeal bar resection (Figure IF). During the first corrective osteotomy, care was taken to position K-wire away from the physis (Figure IE). However, a new lateral physeal bar developed, causing valgus deformity of the distal femur (Figure IIA). The placement of the lateral K-wire at the juxtaphyseal region may have caused iatrogenic injury to the metaphyseal artery, resulting in growth arrest [2]. To address this, the patient underwent a second surgery which was lateral physeal bar resection and varus corrective osteotomy (Figure IIB).
After the second corrective osteotomy, the axis of the distal femur was restored, indicating a complete lateral bar resection (Figure IIC). However, the distal femur progressively developed varus deformity again. The final CT scan (Figure IID) revealed proximal migration of the bone wax, leading to recurrence of the medial physeal bar. According to Hasler et al., the outcomes of physeal bar excision are unpredictable, with poor results and fair results occurring in 15% to 38% of cases [5]. Their study identified graft dislocation from the resection cavity as the major cause of secondary tethers [5].
Autologous fat, bone wax, polymethylmethacrylate, cartilage, silastic and dura are among interpositional fillers used after physeal bar resection [1]. In this case, bone wax was chosen for its haemostasic properties and its ability to prevent bone bridge formation. Failure of interpositional material was previously explored, including cases where the material migrated away from the resection cavity [5].
We postulate that the connection of the filler to the metaphysis region, particularly when it is positioned obliquely to the window created at the metaphyseal cortex (Figure IIIA), may cause the filler to migrate away from the physis with growth. The space left behind may be filled by a bone bridge, resulting in recurrent tethering to the growth plate. In agreement with Hasler et al., we recommend anchoring the filler at the epiphysis, as shown in Figure IIIB, to prevent proximal migration of the interpositional material.

Figure III: A: bone wax was positioned obliquely to the window created at the metaphyseal cortex. B: suggestion to anchor bone wax to the epiphysis and cortex to prevent proximal migration
Conclusion
High-energy impact injuries near the physis should be followed up for at least one year to ensure that no associated physeal injury is missed, preventing morbid outcomes from the sequalae of physeal arrest. Additionally, we recommend anchoring bone wax packing to prevent proximal migration and recurrence of bone bridges.
References
- Singh V, Garg V, Parikh SN. (2021). Management of physeal fractures: a review article. Indian J Orthop. 55: 525-538.
- Nguyen JC, Markhardt BK, Merrow AC, Dwek JR. (2017). Imaging of paediatric growth plate disturbances. Radiographics. 37: 1791-812.
- Garrett BR, Hoffman EB, Carrara H. (2011). The effect of percutaneous pin fixation in the treatment of distal femoral physeal fractures. J Bone Joint Surg Br. 93: 689-694.
- Smith JT, Kasser JR, Waters PM, Jaramillo DI, Kocher MS. (2008). The effect of pinning across the physis for stabilization of fractures in children: an MRI evaluation. Orthop J Harv Med Sch. 10: 99-102.
- Hasler CC, Foster BK. (2002). Secondary tethers after physeal bar resection a common source of failure? Clinical orthopaedics and related research. 405: 242-249.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.