Reconstruction of Bone Loss in an Open Fracture of the Tibia with a Contralateral Free Tibial Graft: A Case Report and Outcome 10 Years Later
Sabri El Banna * , Serge Vandervelde, Olivier Delahaut
Department of Orthopedic and Traumatology affiliated to Brussel’s Free University, CHU de Charleroi (Hôpital Civil Marie Curie) 142, Chaussée de Bruxelles, 6042 LODELINSART, Belgium
*Corresponding author: Sabri El Banna, Department of Orthopedic and Traumatology affiliated to Brussel’s Free University, CHU de Charleroi (Hôpital Civil Marie Curie) 142, Chaussée de Bruxelles, 6042 LODELINSART, Belgium
Received Date: 12 December 2022
Accepted Date: 16 December 2022
Published Date: 19 December 2022
Citation: El Banna S, Vandervelde S, Delahaut O (2022) Reconstruction of Bone Loss in an Open Fracture of the Tibia with a Contralateral Free Tibial Graft: A Case Report and Outcome 10 Years Later. Ann Case Report. 7: 1093. DOI: https://doi.org/10.29011/25747754.101093
Abstract
We report the case of a 50-year-old man, worker on tracks at railway with a Gustillo grade IIIC fracture of the tibia. Management of bone and soft-tissue loss is described. The evolution and follow-ups with soft tissue and bone healing achieved with a contralateral tibial rod.
Keywords: Open fracture; Tibia; External fixator; Wound debridement; Contralateral tibial rod
Case Report
A 50-year-old man, worker on tracks at railway was victim of an accident during night shift on 05/26/2006 11:45 p.m. The patient seems to have passed under a railway. Arrival on site of the Emergency Resuscitation Mobile Unit (ERMU) who contacts the hospital for “leg amputation at the railway”. Immediate contact with the orthopedic surgeon who can be called back by the hospital. Arrival at the Emergency hospital 50 minutes after the accident. The patient is immediately directed to the operating room for surgical management within 30 minutes of arrival and 80 minutes from the time of the accident.
On clinical examination, the left lower limb was amputated almost completely over the entire middle 1/3 of the leg. However, a continuous posterior skin flap of 1/8th of the periphery of the leg was present (Figures 1-17). Distal pulses were absent, and the distal segment was cold. Neurological assessment was not possible at this stage.

Figure 1: A continuous posterior skin flap of 1/8th of the periphery of the leg was present.

Figure 2 : X-ray imaging shows a multifragmented fracture of the tibia and fibula.
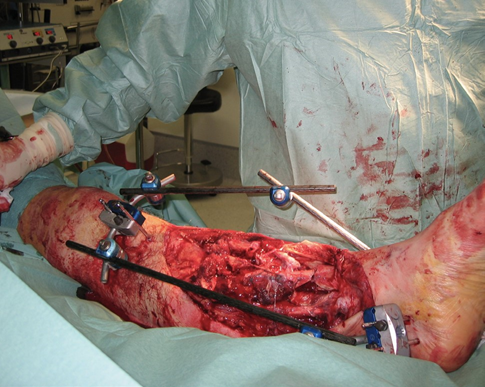
Figure 3 : “Reduction” and osteosynthesis by tibio-calcaneal external fixator was immediately performed.
Method of Treatment
A pulse-lavage with diluted Isobetadine was followed by vascular reconstruction of the tibial vascular pedicles: posterior and anterior as well as the peroneal artery.
A second pulse-lavage was then followed by the reconstruction of neurological lesions observed near the vascular pedicles, while tendons were approximated and sutured according to their original anatomical locations.
Debridement of the wound resulted in the removal of a few completely free bone fragments to avoid the risk of infection.
The wound was closed in as much as it was possible by approximation without tension and bone coverage by a local muscle flap. Incomplete closure at the skin at some levels.
Postoperative Management
The patient was hospitalized for 2.5 months Intravenous antibiotics under the supervision of our infectious disease colleagues associated with regular smears as well as daily wound care were performed. After one week, one smear came back positive for Staphylococcus aureus for which antibiotics were prolonged for 3 weeks.
Complex reflex regional dystrophy (algoneurodystrophy) of the knee, leg and foot was observed. To avoid any ischemic compression, postural drainage and limb suspension by the fixator was done.
We expected secondary healing of the wound without the need for any musculocutaneous flaps such as latissimus dorsi or other.
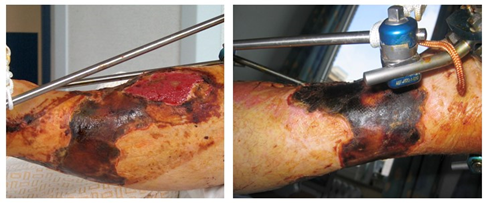
Figure 4, 5: In the beginning, partial skin necrosis was observed and treated by excision and local treatment until healing.

Figure 6, 7 : After 8 months, sufficient skin coverage was obtained to consider filling the loss of tibial defect; algodystrophy was slowly improving.
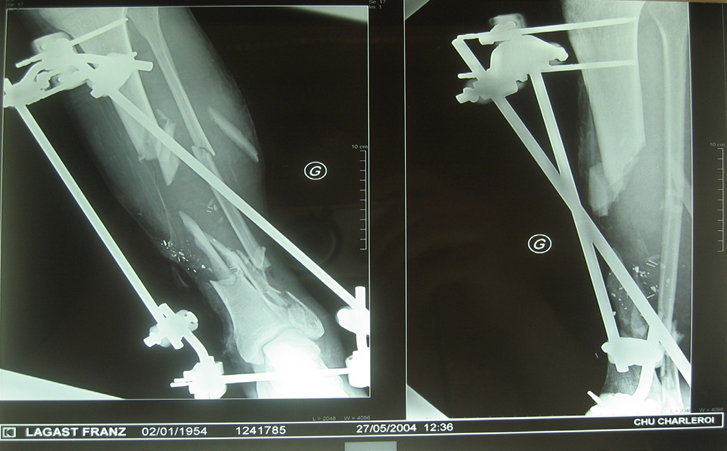
Figure 8 : In view of the present situation the question was what to do next?
|
Allografts: |
|
Bank tibia |
|
Chips with or without growth factors |
|
Autografts: |
|
Vascularized: |
|
Vascularized contralateral fibula |
|
Vascularized iliac crest or rib |
|
Non-vascularized: |
|
Cancellous bones (iliac crests, metaphyses, large trochanter, etc.) |
|
Contralateral tibial rod |
Table 1 : summarizes possible solutions for bone grafting.

Figure 9, 10 : According to the angiogram of the traumatized leg, it was hazardous to perform a vascularized bone graft.
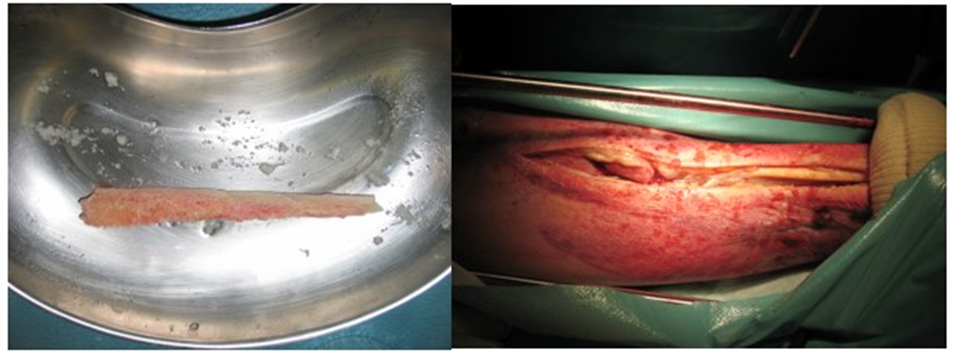
Figure 11, 12 : Our final choice was for a contralateral tibial rod.
Operative technique
The graft was implanted centromedullary to fill the gap between the two tibial extremities, bridging the loss of substance in addition of spongy grafts. The two surgical approaches were closed by simple suture.

Figure 13 : The original fixator was kept in place for the necessary time with no local complications.
Postoperatively, there was a recurrence of the algodystrophy but no further infection. No weight bearing for 3 months.

Figure 14 : Removal of the fixator at 3 months replaced by a walking plaster boot for dynamization.
Currently 15 months after bone reconstruction (23 months post-accident), the patient is full weight bearing with complete recovery of skin and bone as shown in the following pictures (Figures 15, 16, 17).

Figure 15: Currently 15 months after bone reconstruction (23 months post-accident), the patient is full weight bearing with complete recovery of skin and bone.

Figure 16: Currently 15 months after bone reconstruction (23 months post-accident), the patient is full weight bearing with complete recovery of skin and bone.

Figure 17: Currently 15 months after bone reconstruction (23 months post-accident), the patient is full weight bearing with complete recovery of skin and bone.
Discussion
Open fractures of the tibia are the most common open long bone fractures, with an annual incidence of 3.4 per 100 000 [1]. High-energy trauma is the primary mechanism of injury, with over 50% of cases being attributed to road traffic accidents or falls from a great height [2].
Open fractures are categorized according to the GustiloAnderson classification first proposed in 1976 and subsequently modified in 1984 [3]. The case we are presenting is classified IIIc (>10 cm, requiring soft-tissue coverage procedure, with periosteal stripping and vascular injury requiring repair).
The fundamental objectives of treatment are to manage the soft-tissue injury, minimize the risk of infection, stabilize, and repair the skeletal injury and restore the function of the affected extremity [4]. When that is not possible, amputation would be considered.
Several surgical techniques could be performed in successfully managing the traumatic limb injury. However, the literature continues to differ recommending a specific technique and a universal protocol in managing the lower extremity trauma does not exist.
For example, in our case, soft tissue cover by local or crossleg flaps would have failed to cover the defect because of its size, though a free flap could have been used [5]. Finally, skin coverage was solved by conservative local methods.
As for the reconstruction of the skeletal defect, several options were discussed. Contrary to the opinion of one author [6], that a non-vascularised graft in a potentially contaminated bed would have been difficult because of the risk of infection, we had an excellent outcome with a contralateral tibial rod. Actually, the tibia offers the surgeon access to a large quantity of quality autogenous bone that can be harvested easily.
In order to maintain the bone length, with this type IIIc open fracture, ORIF with nail or plates was not an option.
External fixation was a better and accepted option for types IIIA, IIIB and IIIC fractures. As demonstrated by Thakur and Patankar [7]. Excellent results is obtained using a protocol of early bone grafting and fixator dynamization with monolateral fixators.
Conclusion
This case shows the feasibility and success of less hazardous surgical techniques in managing large skeletal defects. It was possible to restore bone length, soft tissue healing and an excellent functional outcome. In case of failure, vascularized musculosqueletal grafts are an option as a secondary procedure. However, time to obtain healing was relatively long but this was the price to obtain the requested result.
References
- Court-Brown CM, Bugler KE, Clement ND, Duckworth AD, McQueen MM (2012) The epidemiology of open fractures in adults. A 15-year Injury; 43: 891-7.
- Larsen P, Elsoe R, Hansen SH (2015) Incidence and epidemiology of tibial shaft fractures. Injury; 46: 746-50.
- Gustilo RB, Anderson JT (1976) Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones. Retrospective and prospective analysis. J Bone Joint Surg; 58A: 453.
- Okike K, Bhattacharyya T (2006) Trends in the management of open A critical analysis. J Bone Joint Surg; 88-A: 2739-48.
- Manktelow RT (1987) Microvascular reconstruction. Anatomy, applications and surgical technique. Springer, Berlin Heidelberg NewYork Tokyo. 12.
- Schuind F, Burny F, Quintin J, Potaznik A, Pasteels JL (1989) Single stage reconstruction of a large tibial defect using a free vascularised osteomyocutaneous ulnar transfer International Orthopaedics (SICOT); 13: 239-245.
- Thakur AJ, Patankar J (1991) Open tibial fractures. Treatment by uniplanar external fixation and early bone grafting. J Bone Joint Surg 73: 448-51.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.