Pyosalpinx in a 12-Year-Old Virgin Following an Untreated Pharyngitis Caused by Streptococcus Pyogenes
by Faton Zeneli1, Giannina Buzzi2, Larissa Greive2, Irene Graf-Rüegg2, Mario Valerio Tartagni2*
1Department of General and Visceral Surgery, HOCH Health Ostschweiz Spital Wil, Wil, Switzerland
2Department of Gynecology and Obstetrics, HOCH Health Ostschweiz Spital Wil, Wil, Switzerland
*Corresponding author: Mario Valerio Tartagni, Department of Gynecology and Obstetrics, HOCH Health Ostschweiz Spital Wil, Fürstenlandstrasse 32, 9500, Wil, Switzerland
Accepted Date: 18 March 2025
Accepted Date: 21 March 2025
Published Date: 24 March 2025
Citation: Zeneli F, Buzzi G, Greive L, Graf-Ruegg I, Tartagni MV (2025) Pyosalpinx in a 12-Year-Old Virgin Following an Untreated Pharyngitis Caused by Streptococcus Pyogenes. Ann Case Report. 10: 2225. https://doi.org/10.29011/2574-7754.102225
Abstract
Case: Pyosalpinx in sexual inactive patients is rare and usually not the first differential diagnosis considered in acute abdomen. We report a case of 12-year-old, sexually inactive patient with unilateral pyosalpinx with appendicular involvement following an untreated pharyngitis caused by Streptococcus pyogenes. A laparoscopic salpingotomy and appendectomy were performed to treat this patient followed by a 10-days antibiotic therapy with amoxicillin/clavulanic acid. The swabs taken from the pyosalpinx and appendix grew Streptococcus pyogenes which was sensitive to chosen antibiotic therapy. Conclusions: Pelvic inflammatory disease (PID), with or without pyosalpinx, may result from untreated Streptococcal pharyngitis in young girls without typical risk factors. Even if streptococcal pharyngitis appears to be resolving spontaneously, antibiotic treatment is still advised to prevent potential complications. Laparoscopy is the preferred diagnostic and therapeutic approach to confirming the suspicion of salpingitis, with or without pyosalpinx, and can also identify appendicular or other abdominal involvement.
Keywords: Pyosalpinx; Streptococcus Pyogenes; Pharingytis; Virginity; Adnexitis.
Introduction
Acute salpingitis is a prevalent acute condition in women, often linked to sexually transmitted infections such as Chlamydia trachomatis and Neisseria gonorrhoeae but also intestinal bacteria. Additionally, it has been noted to have connections with bacteria commonly associated with bacterial vaginosis, including Mycoplasma, Urea plasma, Gardnerella vaginalis and anaerobes [1]. While Lancefield group A β-hemolytic Streptococcus, or Streptococcus pyogenes, typically causes mild and self-limiting epithelial infections like pharyngitis and impetigo, certain aggressive strains can lead to severe invasive diseases such as bacteremia, toxic shock syndrome or necrotizing fasciitis. This augmented virulence is attributed to the production of superantigens as streptococcal exotoxins [2,3]. Pyosalpinx in young and sexual inactive patients is rare and usually not the first differential diagnosis considered in acute abdomen. We report a case of 12-year-old, sexually inactive patient with unilateral pyosalpinx with appendicular involvement following an untreated pharyngitis caused by Streptococcus pyogenes.
Case
A 12-year-old virgin girl presented to emergency ward with ongoing menstruation for the past two weeks and history of sharp pain in the lower abdomen in the last 24 hours. Other symptoms like vaginal discomfort, urinary or digestive symptoms were denied. No history of prior surgeries or previous illnesses except for a febrile episode with sore throat and rhinitis three weeks ago. A pharyngitis caused by group A β-hemolytic Streptococcus was diagnosed approximately 3 days after the onset of symptoms but left antibiotically untreated because of spontaneous remission of symptoms. Menarche occurred five months prior. Irregular menstrual cycles with the last one beginning three weeks prior which continued for three weeks until the previous day. The patient never used tampons, no IUD. When presenting in the emergency ward the patient had a low-grade fever around 38°C but was otherwise in good general condition. Physical examination revealed a sharp pain in the right lower abdomen without abdominal guarding on palpation. The gynecologic examination of vulva and vagina was normal with an intact hymen. Neither a foreign body nor vaginal bleeding were detectable. An abdominal – pelvic ultrasound showed a cystic mass by the right ovary measuring 3.5cmx3cm with inconspicuous uterus a swell as left ovary. Vessels with venous fluid profile were not altered as in possible ovarian torsion. The appendix could not be visualized. While waiting for blood results the patient presented with rising fever up to 40°C and deterioration in general condition. The laboratory results revealed leucocytosis (18 G/l), a slightly elevated CRP (29 mg/l), normal haemoglobin and a negative urine pregnancy test.A diagnostic laparoscopy was performed. The patient was found to have a right pyosalpinx and a haemorrhagic ovarian cyst. For this reason, a salpingotomy with evacuation of pus and a cyst fenestration were performed (Figure 1.). Intraoperative no evidence of appendicitis acute although the appendix reached into the purulent fluid collection, for this reason an opportunistic appendectomy was also performed (Figure 2.). Postoperative intravenous antibiotic therapy with amoxicillin/clavulanic acid for 6 days followed by 4 days per os was initiated. The swab taken from the pyosalpinx and appendix grew Streptococcus pyogenes which was sensitive to amoxicillin/clavulanic acid. The histological examination of the appendix revealed an appendicitis acuta. The postoperative recovery was uneventful. The patient was discharged in a healthy condition on the fifth day after surgery. Regarding the hypermenorrhoea, a therapy with Estradiol valerate (2 mg) + Norgestrel (0.5 mg) was initiated.
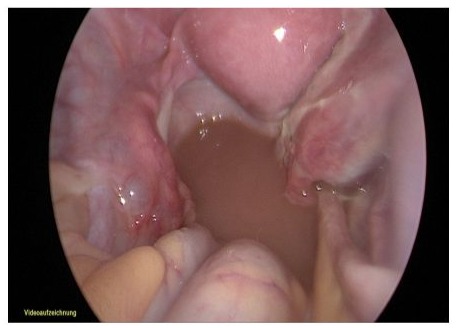
Figure 1: Right pyosalpinx with right haemorrhagic ovarian cyst and purulent fluid collection in rectouterine pouch.

Figure 2: Appendix vermiformis.
Discussion
Possible differential diagnoses for lower abdominal pain with elevated infection parameters encompass appendicitis, diverticulitis, peritonitis, urinary tract infection, adnexitis and other potential causes. Adnexitis primarily arises from Chlamydia trachomatis, Neisseria gonorrhoeae or intestinal bacterial infections, typically through ascending routes rather than hematogenous spread. Hematogenous spread seems to be the cause of salpingitis in our patient because of history of untreated streptococcal pharyngitis approximately a week prior to the operation. Very few cases of Pyosalpinx in sexually inactive patients caused by Streptcoccus pyonogenes have been described in literature, while is more common in older, sexually active patients or IUD-carriers [4,5]. The low occurrence of S. pyogenes salpingitis may be due to its infrequent presence in the typical vaginal flora of post-pubertal females [6,7]. Streptococcus pyogenes likely resides in the vagina briefly, potentially from self-contamination, close contact sources like the pharynx, or even gastrointestinal carriage in rare instances [8]. Direct transmission could be an alternate route of infection, particularly in acute appendicitis cases [9]. Serious complications such as peritonitis, fallopian tube torsion or subsequent fallopian tube sterility may arise after pyosalpinx development [10].
Conclusions
Physicians should note that PID with or without pyosalpinx can occasionally stem from untreated Streptococcal pharyngitis in young girls without traditional risk factors. Additionally, even if streptococcal pharyngitis appears to be in spontaneous remission, antibiotic treatment is still recommended to prevent potential complications. Laparoscopy is the gold standard for the diagnosis and treatment of salpingitis with or without pyosalpinx and can confirm appendicular or other abdominal involvement.
Consent for publication: Informed consent was obtained from the patient’s guardian for publication of this manuscript and any accompanying images in anonymized form.
Data Availability: The data supporting findings cannot be made available as containing proprietary information.
Disclosure statement: The authors declare that they have no competing interests.
Ethics Statement: Our institution does not require ethics approval for reporting individual cases if the given treatment follows the standard guidelines.
References
- Hebb JK, Cohen CR, Astete SG, Bukusi EA, Totten PA. (2004) Detection of novel organisms associated with salpingitis, by use of 16S rDNA polymerase chain reaction. J Infect Dis. 190:2109–20.
- Plainvert C, Doloy A, Loubinoux J, Lepoutre A, Collobert G, et al. (2012) Invasive group A streptococcal infections in adults, France (2006–2010). Clin Microbiol Infect.18:702–10.
- Nelson GE, Pondo T, Toews K-A, Farley MM, Lindegren ML, et al. (2016) Epidemiology of invasive Group A streptococcal infections in the United States, 2005–2012. Clin Infect Dis.63:478–86.
- Brown-Harrison M, Christenson J, Harrison A, Matlak M. (1995) Group A Streptococcal Salpingitis in a Prepubertal Girl. Clin Pediatr. 34:556–558.
- Blot M, de Curraize C, Salmon-Rousseau A, Gehin S, Bador J, et al (2017) Streptococcus pyogenes: an unusual cause of salpingitis. Case report and review of the literature. Infection. 45:697-702.
- Philip BM (2008) A streptococci in late pregnancy. Infect Dis Obstet Gynecol. 8:217–9.
- Beargie R, Lynd P, Tucker E, Duhring J. (1975) Perinatal infection and vaginal fora. Am J Obstet Gynecol. 122:31–3.
- Sobel JD, Funaro D, Kaplan EL. (2007) Recurrent group A streptococcal vulvovaginitis in adult women: family epidemiology. Clin Infect Dis.44: e43–5.
- Singh-Ranger D, Sanusi A, Hamo I. (2008) Coliform pyosalpinx as a rare complication of appendicectomy: a case report and review of the literature on best practice. J Med Case Rep. 2:97.
- Hillis SD, Joesoef R, Marchbanks PA, Wasserheit JN, Cates W Jr, et al (1993) Delayed care of pelvic inflammatory disease as a risk factor for impaired fertility. Am J Obstet Gynecol. 168:1503-1509.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.