Prosthetists' Perspective on Surgical Intervention, Postoperative Treatment, and Prosthetic Assessment Following Transtibial Amputation
by Anton G. Johannesson1*, David F. Rusaw2
1Ossur Clinics EMEA, Stockholm, Sweden
2School of Health and Welfare, Jönköping University, Jönköping, Sweden
*Corresponding author: Anton G. Johannesson, Ossur Clinics EMEA, Stockholm, Sweden
Received Date: 04 December 2024
Accepted Date: 09 December 2024
Published Date: 11 December 2024
Citation: Johannesson AG, Rusaw DF (2024) Prosthetists' Perspective on Surgical Intervention, Postoperative Treatment, and Prosthetic Assessment Following Transtibial Amputation. J Surg 9: 11202 https://doi.org/10.29011/2575-9760.11202
Abstract
Background: Many healthcare professionals collaborate in the clinical care of individuals who have undergone a Transtibial Amputation (TTA), and a good start to their rehabilitation is essential. The Prosthetist plays a long-term role in patient care, while surgeons often have limited follow-up, typically 1-2 weeks post-surgery.
Objective: This paper aims to present the perspective of two Prosthetists on the subject of TTA: why this perspective is needed, the effect of the limb length, the incision techniques used, new alternatives in postoperative treatment, and its impact on early prosthetic fitting, within a Swedish context.
Methodology: To address this aim, each section was discussed individually, summarizing relevant evidence from a professional perspective, using various evidence sources (e.g., peer-reviewed literature, and national patient registries).
Findings: From the authors' view, when using modern postoperative treatment and prosthetic technology, the Sagittal Incision (SF) incision may be beneficial to Posterior Flap (PF) incision in TTA, if the aim is to reduce the time to prosthetic fitting. New postoperative treatment methods are being made more accessible and recognized. This might not be a valid solution in all places, but they contribute to the evidence base used for decision-making following TTAs.
Conclusion: From a Prosthetist perspective, more could be done to improve the pathway from amputation to prosthetic fitting and ensure the best functional outcome for the patient. Traditional methods from the 1950s have been discussed, and other alternatives have been contrasted.
Keywords: Amputation; Postoperative; Treatment; Transtibial; Outcome
Introduction
Many healthcare professionals will be required to interact and collaborate with all the relevant team members involved in the clinical care of individuals who have undergone a Lower Limb Amputation (LLA). These will include all those appropriate to the rehabilitation team [8 professions according to the World Health Organisation (WHO)] and the patient, family members, and others [1]. Communication and understanding within this team build upon a standard set of values and models for communication. The International Classification of Functioning, disability, and health (ICF) can facilitate this communication by allowing all involved to use a shared language and framework. Professional culture and norms can often dictate how and why we communicate in healthcare teams. Still, the ICF is an accepted and valuable tool that allows communication that considers the complex perspective of an individual's health concerns [2]. There are many historical connections between orthopedic surgery and prosthetics. Long before the formation of the rehabilitation field and subsequent professionalization of rehabilitation, prosthetists (or their historical predecessors) were working to ensure that individuals who had amputations were able to be as active and participate in their lives as much as possible [3]. For this reason, we have a very long professional relationship. As such, we have much to discuss.
Since rehabilitation consultants and prosthetists are involved in long-term patient care, often at different stages, it is essential to adopt a patient-centered perspective. Surgeons, in contrast, typically engage with the patient for a short period, primarily focused on achieving successful surgical outcomes before considering their role complete. Rehabilitation professionals, such as consultants, physical therapists, and occupational therapists, continue care afterward. This linear treatment approach often limits interdisciplinary collaboration discussions from an International Classification of Functioning (ICF) perspective. Within orthopedics, outcomes focus on the ICF's body function and structural impairment domain, with a minimal proportion (16%) of studies measuring activity or participation [4]. This focus may contribute to a bias among surgeons, who often prioritize surgical outcomes over a more holistic view that includes activity and participation domains. Prosthetists' primary goal is to enhance a patient's activity and participation through appropriate assistive technology. As such, surgical outcomes related to body function and structure directly influence prosthetic outcomes, making them critically important. Interdisciplinary dialogue on how these domains interact would greatly benefit patients, as understanding how a surgeon's decisions affect body structure and function has lasting, irreversible impacts on a person's ability to remain active and participate in life. With their specialized training, prosthetists are responsible for the patient's prosthetic care and often maintain lifelong relationships with the user. A solid start to rehabilitation is crucial for achieving functional, long-term outcomes.
The standards of orthotic and prosthetic (O&P) care, developed by WHO and ISPO, begin at the "Assessment" stage and typically exclude earlier surgical considerations. However, decisions made during the amputation process can affect the user for years, both positively and negatively, and should be part of ongoing discussions to refine care and prevent future mistakes [5]. In contrast, surgeons (unless subspecialists) typically follow patients for only 1-2 weeks post-surgery and rarely perform Lower Limb Amputations (LLA) [6]. This paper is written from the perspective of two prosthetists in Sweden, and some aspects of postoperative care leading to prosthetic fitting may differ from those in other settings.
In the Prosthetist's first contact with the amputee, the most common surgical method they face at this level is the Long Posterior Flap technique [7] and, in certain regions, the Sagittal incision technique [8]. This immediate contact after the LLA is hopefully with the Prosthetist as part of the multidisciplinary team (including doctors, physiotherapists, nurses, and occupational therapists). This has been seen optimal treatment for patients who have had a LLA [9]. An alternative scenario occurs when patients arrive at clinic with a referral for prosthetic provision several months post-amputation or at any subsequent point in between. In extreme cases, this delay may result in complications such as ineffective compression therapy and contractures in both the knee and hip, significantly hindering the patient's possibilities for mobility and motivation. These issues can also negatively impact long-term rehabilitation outcomes [10]. Irrespective of location or resource setting, this is concerning. Many healthcare systems do not follow international standards for prosthetic service. The concern here is that standards ensure the quality of care is consistent and high for individual patients. If not followed, patients are at risk of receiving low-quality, inconsistent care and delayed rehabilitation [11]. The prosthetist's role varies between countries, and even within a country, and is often dependent on their level of education relative to other healthcare providers, or whether they operate as private or state providers. Irrespective, when examining the contributions of prosthetists to the pre-amputation and postoperative processes, their input is often limited. This is likely due to other allied healthcare professionals predominantly produce much of the literature and knowledge in these areas [3].
This paper aims to present a Prosthetist perspective related to transtibial amputation: why this perspective is needed, the effect of the limb length, incision techniques used, new alternatives in postoperative treatment, and its impact on early prosthetic fitting.
Materials and Methods
To address this aim, we will discuss each section individually, summarizing relevant evidence and perspectives, from a professional perspective.
Results and Discussion
I. The length and condition of the residual limb as a facilitator of active and participatory lives. Following World War II, basic research demonstrated that an amputee's gait benefited from retaining as much healthy bone and soft tissue as possible [3]. However, a literature review regarding the length of the residuum from the 1970s and forward has found inconsistent results. In 1977, Marsden recommended limiting the length of the residual limb to 15 cm, reasoning that this would make prosthetic fitting easier for prosthetists [12]. This assumption likely stemmed from the fact that older prosthetic technology, such as wooden ankles, required more space between the distal end of the limb and the floor. However, by that time, prosthetists in developed countries were already utilizing modular socket systems, which offered greater flexibility and improved fitting options, making the need for such a limitation less relevant. Today, many prosthetic foot models are designed to accommodate reduced build height while offering various functional benefits to users. As a result, the historical argument for shorter residual limbs to facilitate prosthetic fitting no longer holds, given the advancements in prosthetic technology. These developments provide significantly more options for users with residual limb characteristics that were once considered disadvantageous. Recent evidence, even from studies on other lower limb amputation levels, suggests that the overall condition of the residual limb, not just its length, is the key factor influencing a person's functional outcome post-amputation [13]. If there is doubt, a surgeon should ask a prosthetist for advice regarding the optimal length and proposed foot and components for the patient preoperatively.
In 1992, Tooms RE recommended, “Ideally, the tibia length for TTA is 12.5 to 17.5 cm depending on the body height”, as we assume that the individual height impacts the selected residual limb length [14]. This marked an improvement over prescribing a fixed length, offering a more tailored approach. Persson and Liedberg suggested a different and more straightforward measure of the residual limb length by using the width of the knee. Their method proposes defining a limb as "Ordinary" when the length is between 1 and 2 times the width of the knee, "Short" if the length is the same or less than the width, and "Long" if the length is more than twice the width of the knee [15]. Although simplified, it uses patient characteristics other than width alone, fixed measurements (e.g., centimeters), or the surgeon's handbreadth [7]. In 2002, in the second Edition of Atlas of Amputation and Limb Deficiencies, the late Professor John H Bowker summarized: “There is no longer an ideal length or site of amputation. In vascular absent popliteal pulse, amputation in the proximal half of the leg would seem reasonable, with a bony level as distal as the junction of the proximal and middle thirds. In cases with good blood flow to the ankle, bone length at the junction of the middle and distal thirds will provide a very functional residual limb. Modern prosthetic components can be easily matched to these more distal levels” [16]. In the latest, 5th edition of the Atlas, published in 2024, J.R. Ficke states: "The ideal residual limb length is at least 12 cm distal to the knee joint line and at least 25 cm above the plantar heel pad, where sufficient gastrocnemius muscle can serve as padding via myodesis." While this recommendation offers a theoretical range, it still prescribes two fixed points, overlooking important factors like tissue condition, patient height, and residual limb width. As such, it represents both progress and a limitation in defining optimal residual limb length post-amputation. The problem is the fixed measurement without reference, e.g., to the "optimal components”, the person's length, or both. The benefit of a longer residual limb could be related to a longer lever arm, less energy to ambulate, and more area to distribute the load [17]. The negative effect of long TTAs can be due to the nerve impingement risk related to conical pressure between the distal Tibia and Fibula. Using a bone bridge, e.g., Ertl's procedure, has been proposed as an alternative in these cases [18]. Skin complications can arise from a combination of poor vascularity, insufficient soft tissue, and inadequate prosthetic suspension (e.g., pistoning effects). Pistoning within the prosthetic interface negatively impacts the soft tissue [19], leading to friction-related issues like redness, blisters, and eventually wounds, which can hinder long-term prosthetic use. These challenges, especially in cases of longer residual limbs, raise important questions about the functional limitations of shorter residual limbs.
In Wheeless' Textbook of Orthopaedics: Below Knee Amputation, they also added that in residual limbs less than 9 cm, the surgeon could consider removing the entire Fibula along with the Soleus muscle (e.g., Brückner technique). According to this textbook, if the residuum measures less than 5 cm, the surgeons should consider amputation at the next higher level [20]. The current shortest length of the tibia to be fitted with a prosthesis is, in general, at the level of the distal end of the tibial tuberosities (preferably using the Brückner technique) [21]. The availability and option of using a gel liner with vacuum sleeve suspension extended over the knee (or hinges) to support the thigh and lightweight prosthetic components can give the user an excellent function (Figure 1). If the focus is on mobilizing patients with prostheses, these options should be carefully considered and validated before selecting a higher amputation level.

Figure 1: Transtibial prosthesis with pin lock and thigh support for a short limb.
To summarize these recommendations on residual limb length from a prosthetist's perspective, Bowker's view remains the most favored for its guidance on length and consideration of the prosthetic foot's build height. This aligns with Ficke's emphasis on ensuring sufficient gastrocnemius muscle for effective padding at the distal end. Conversely, the minimum residual limb length is determined by the rehabilitation goal, specifically prosthetic fitting, and depends on the knee joint's condition and the availability of rehabilitation resources and lightweight prosthetic components.
II. The Potential Effect of the Incision Technique on Prosthetic Fitting
i. Long Posterior Flap (PF): The most widely used incision technique in transtibial amputation is the PF technique, often referred to as the Burgess technique, developed in the 1950s [22]. More recent attempts have been made to develop a more standardized approach to the original proposal [7]. Some aspects of this approach can be questioned today, including recommendations regarding the limb length, the bulbous shape of the limb, and the position of the scar; applying the incision scar directly over a distal bone area can present risks of creating adherences between the skin and the bone [23]. Burgess's evolution of the PF surgical technique coincided with changes in prosthetic technology in the 1950s and his close cooperation with prosthetists [22]. At that time, standard care was transitioning from the "conventional" prosthesis with a thigh corset and hinges to a Patellar Tendon Bearing (PTB) socket [24]. It also included a more holistic approach to postoperative treatment following amputation utilizing rigid dressing, compression therapy, early mobilization, and long-term care of the amputee, which is still considered state-of-the-art [25]. PTB fitting required a well-padded distal end to facilitate early rehabilitation (Figure 2). This need could be demonstrated in later studies where the distal end of the tibia was, on average, shifting 7.5 cm (2.8 inches) during one gait cycle. In a full day, the tibial end could be expected to move approximately 232.5 cm (92 inches) within the PTB socket [26]. Additional issues with this technique are often related to the bulbous form and the placement of the scar transversally over the distal tibia, where one of the highest peak pressure points occurs during the gait cycle [17]. An incision scar that has become adherent is a constant concern during prosthetic use, as shear forces, often related to adherence, can affect the skin condition and user comfort [27]. The benefit of this technique can be related to the proximal muscle bulk (the proximal part of the gastrocnemius and the soleus muscles) that can stabilize the socket in swing phase.
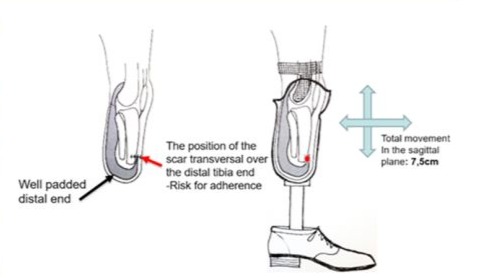
Figure 2: Burgess-technique and the PTB socket.
ii. Skew Flaps (SkF): Robinson's SkF technique was developed to address the bulbous shape of the residual limb, which can delay initial prosthetic fitting, and to minimize the risk of skin breakdown caused by placing the scar over the tibia [28]. The incision line was therefore rotated by 15⁰, resulting in skewed flaps and the scar shifted from the point of high pressure. However, forming the gastrocnemius-soleus muscle into a long posterior myoplastic flap and covering the distal end of the bone, similarly to the traditional posterior flap technique, is still utilized. The downside of this method is that it requires separation of the skin from the muscle flap, which can be challenging to perform in individuals with vascular disease [28]. In a recently published study, long PF and SkF were found to have similar outcomes regarding surgical failures [29].
iii. Sagittal Flaps (SF): The sagittal incision technique has increased in popularity among surgeons who perform TTAs in Sweden. With a similar holistic approach to Burgess's recommendation, changes in procedures in most hospitals performing amputations in Sweden have occurred during recent decades, including the use of sagittal incisions [30]. The sagittal incision technique was popularized as the primary TTA technique in southern Sweden by Persson in the late 1960s. In his publication [31], he names two specific reasons related to the lower risk of necrosis in dysvascular individuals: firstly, the placement of flaps medially and laterally reduces the amount of poorly vascularized anterior skin that remains, and secondly, the resultant flaps are wide and short, thus enhancing their viability. Persson also stated that a side-to-side myoplasty ensures better coverage and good spontaneous drainage [31]. Additional benefits of this incision technique became evident later due to the position of the scar, especially when modern liner and suspension technology became more widely used [32].
iv. Myoplasty/Myodesis: Myoplasty, a procedure where agonistic and antagonistic muscles are sutured together over the distal end of a bone, can aid in early rehabilitation by providing greater stabilization of the incised muscle tissue. For transtibial prosthesis users, it is recommended that the deepest muscle layers be anchored directly to the bone, while the more superficial layers are joined using myoplasty techniques [33]. This alters the function of the gastrocnemius from a two-joint muscle to a single-joint muscle. Following amputation, the soleus and anterior tibial muscles lose their function, which affects the degree and rate of atrophy in the residual limb due to the changed role of the remaining muscles.
Bowker stated, "Myodesis provides firm fixation of the posterior muscle padding to the tibia, thus preventing later retraction. It is contraindicated, however, in cases of severe dysvascularity in which the blood supply to the muscle appears compromised. In these cases, myoplasty will be sufficient" [16]. The scar will diminish over time (Figure 3), and the non-active muscle fibers will not only atrophy but also change to fat cells and, finally, be absorbed by the body [34]. Lilja et al. found that muscle morphological changes begin immediately postoperatively and continue simultaneously with reduced edema. The amount of this atrophy can be correlated to physical activity, postoperative bandaging, and prosthetic fit [34]. In summary, preserving the knee joint is critical for optimal mobility following a high-level limb amputation. Equally important is a well-planned postoperative treatment and an undisturbed healing process, especially when the functional goal is to fit the patient with a prosthesis. A 2014 Cochrane Review [35] found no significant differences in primary stump healing rates, revision rates, or reamputation rates, regardless of the incision method used. However, the review did not consider factors such as postoperative treatment, dressing types, or compression therapy. Interestingly, one of the studies highlighted in the review found that amputations with sagittal incisions had shorter prosthetic fitting times than those with long posterior flaps [36].
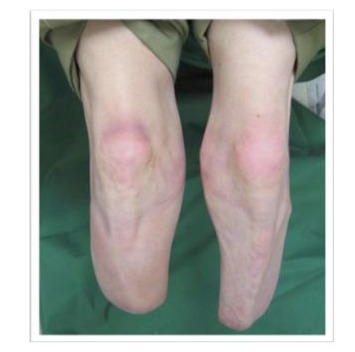
Figure 3: Bilateral amputation: left side from 1996, and the right side 2006. Observe the rate of atrophy and that the incision scar is barely noticeable.
However, one must consider that the included studies were published between 1968 and 1999 [35]. Since the late 1990s, options for prosthetic service providers have dramatically evolved, especially related to interface options [37]. This includes the prosthetist's decisions regarding early prosthetic fitting, fabrication methods, liner selection, and suspension techniques. These choices are influenced by the shape of the limb, whether it is bulbous or cylindrical. Achieving a cylindrical shape sooner makes donning the prosthetic socket easier, facilitating earlier prosthetic fitting. A cylindrical shape can be attained more quickly with a sagittal flap compared to a posterior flap, as the upward folding of the posterior flap can compromise circulation and create 'dog ears' at the scar site, leading to a bulky distal end [38]. Therefore, depending on the viability of the tissue or previous surgery, a reasonable recommendation would be to use an SF-incision, if the aim is to expedite early prosthetic fitting.
III. Postoperative Phase and the Effect on Early Prosthetic Fitting
As previously mentioned, the shape of the residual limb is crucial for early prosthetic fitting and restoring the patient's mobility. Traditionally, using a PF technique, combined with soft dressings and bandaging, often results in a bulbous limb shape and challenges in achieving consistent compression, which can delay early prosthetic fitting (11,38). However, new alternatives in postoperative treatment, such as using postoperative liners instead of bandaging, are gaining popularity [30,32]. Effective control of post-surgical edema is essential for shaping the residuum and facilitating the first prosthetic fitting [11].
i. Rigid dressing: Plaster-of-Paris rigid dressings have never been widely adopted due to personnel difficulties for vascular surgeons, as competent professionals who apply the dressing may not be available in all regions or facilities. On the contrary, where orthopedic surgeons conduct amputation, rigid dressings are much more common [39]. Rigid dressing usage after lower limb amputation has been evaluated in more than 350 articles, including three systematic reviews [23,40,41], reporting that rigid and semi-rigid dressings have advantages associated with reduced pain and the usage of pain medication, better wound healing and volume control, protection against injury during falls, lower risk of knee contracture, reduced time in hospital, and reduced time to prosthetic fitting. Despite the reported benefits of rigid dressings, soft dressings remain the most used option following Transtibial Amputation (TTA). The primary goal of a soft dressing is to absorb wound fluid and prevent edema using a compressive elastic bandage, which is cost-effective but comes with potential risks. For instance, pressure levels under soft dressings can vary significantly, and improper application may result in complications such as pressure sores and persistent edema. To date, no studies have demonstrated that soft dressings provide superior outcomes compared to rigid or semi-rigid dressings [40]. Factors that limit the use of rigid dressings are believed to be related to application difficulties (surgeons may need assistance during application), time taken (time for application, prolonged anesthesia, and cleaning), difficulty in wound inspection (surgeons may prefer to have easy access to the wound, especially if complications occur) and risk of pressure ulcers or pressure on the patella [42-45]. An alternative to Plaster-of-Paris is a Removable Rigid Dressing (RRD) or a vacuum-formed Removable Rigid Dressing (ORD), which, in a randomized trial, has been compared with a conventional Plaster-of-Paris rigid dressing, with similar outcomes [42]. This dressing has been shown to solve some of the problems mentioned above while retaining the advantages of the Plaster-of-Paris dressing.
Limb volume postoperatively, before applying the rigid dressing in the operation theater, already includes, in theory, edema, which is necessary to promote healing. Correctly applied rigid dressings do not apply additional pressure. However, excessive edema, leading to internal pressure, could indicate uncontrolled infection, creating problems with non-removable rigid dressing. With a removable rigid dressing, this can be observed and controlled more easily [42]. ORD should, however, be distinguished from other RRDs. Although it has many of the same features as traditional RRD: to be removable and act as a protective shell for the reimaging limb in case of falling, it additionally conforms to the surface of the remaining limb, adapting to the early volume changes, when compared with the fixed shape of the traditional RRDs [42].
ii. The use of silicone postoperative liner for compression therapy: The use of a special silicone postoperative liner [32] is now a standard treatment in most clinics in Sweden (30). Compression therapy can begin 5-7 days after amputation, once the rigid dressing is removed. The liner size is determined by taking a circumferential measurement 4 cm from the distal end of the residual limb. Initially, compression is applied twice daily (morning and afternoon), with the duration gradually increasing from 1 to 4 hours, adding an hour each day, until the patient can apply it independently and regulate its use. A soft stockinette is worn day and night when the liner is not used to maintain compression. If the patient needs to stand or mobilize, applying the liner beforehand is recommended to prevent excessive edema. The liner size is adjusted as needed to ensure consistent compression, and both the duration of use and circumferential measurements should be recorded [32]. The use of Surgical clamps instead of sutures is not recommended in this protocol, nor is the use of drains, as many of elderly patients have vulnerable skin tissue and a higher risk of infection after surgery [43]. In the PF incision, with the suture line transversally placed over the distal tibia, there is a risk that the compression creates pain during the compression therapy with a liner due to the risk of the clamps hitting the distal tibia.
iii. The postoperative compression liner and the differences in effects when using either the SF or the long PL flap incision techniques: The silicone postoperative liner is an easy alternative to traditional residual limb management. The same compression level is achieved regardless of who applies the liner. In conventional care, the compression and the quality of the soft bandage application can vary depending on the individual who performs the treatment [32,42]. The main benefit of the SF incision compared with the PF technique is the placement of the incision scar (optimal is to have it between the Tibia and Fibula) and the minimal risk of ending up with the traditional bulbous form [44]. An additional benefit of the scar position with a silicone postoperative liner is that when the liner is inverted, it stretches the innermost material. The tension created by contact between the silicone and skin helps to pull the soft tissues of the residual limb into the liner (Figure 4 A).
Three objectives are achieved in this phase (Figure 4):
- Stretching of the soft tissue in a forward direction (Figure 4A). This helps to keep the wound closed.
- The compression of the wound surfaces along the suture lines (Figure 4B). To minimized excessive edema.
- An even compression that decreases proximally because of the decreasing thickness of the liner walls (Figure 4C). The geometry of the liner automatically generates this.
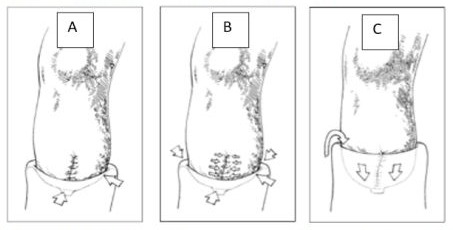
Figure 4: Function of the postoperative liner on the sagittal incision.
Compared with traditional treatment, the improved effects of using a silicone compression liner on scar tissue can be visualized (see Figure 5), and a similar effect is observed as with general scar tissue treatment using silicone gel. This treatment period allows the skin to adapt to the new environment. This includes the adaptation regarding perspiration and how to don and take off a liner correctly, hence taking care of the affected skin. It is later included as a part of modern prosthetic technology (e.g., liner and vacuum suspension).

Figure 5: Heald scar after a typical Sagittal incision, the use of rigid dressing followed by compression therapy with postop liner.
In summary, soft dressings combined with compression bandaging remain the most used postoperative method, with little change since the 1950s. Using a removable rigid dressing (ORD) provides similar results to Plaster of Paris rigid dressings and offers added protection in case of falls. After 5-7 days, once the situation has stabilized, silicone postoperative liners can be a preferred option for compression therapy. Early liner treatment offers additional benefits by keeping the suture line intact and allowing the skin 3 to 6 weeks to acclimate to the new environment before the loading and unloading process associated with prosthetic use, while also gradually increasing compression on the soft tissue.
IV. Prosthetic fitting
All main components in the process can be updated compared with the traditional methods, aiming at early prosthetic fitting on a well-prepared limb. These changes allow the use of a direct manufacturing prosthetic technique early in the process if suitable [32].
i. Direct Socket manufacturing procedure: Since 1997, the introduction of direct lamination techniques using carbon fiber and polyurethane resin, combined with pressure casting, has provided new alternatives for manufacturing prosthetic sockets. These advancements have significantly reduced rehabilitation time compared to traditional methods. The new postoperative techniques align well with the CE-marked Direct Sockets concept [45], reducing the need for temporary socket solutions and minimizing time-consuming volume adjustments [6]. Direct Socket technology is produced and fitted on-site to optimize patient outcomes, significantly improving the results of the first prosthetic fitting, as reported by the SwedeAmp register [30].
Summary of the process
Despite efforts to incorporate innovative technologies in certain areas of prosthetic production, transtibial amputation techniques and postoperative care have seen little significant innovation since the 1950s, especially when compared to other advancements in healthcare. This stagnation may be attributed to the complexity of the process, the involvement of multiple professions, challenges with reimbursement systems, limited access to the latest developments and technologies, and a lack of consensus on treatment protocols. Additional difficulties could include inherent hierarchies in the system and the lack of an intradisciplinary approach when working with this patient group. The process that we suggest was made to improve the whole process, with elements connected to each other, using new products that were unavailable in the past, recording the outcome, and reporting it back to those who performed the amputation.
V. The outcome of the Swedish process
In 2010, Johannesson et al. presented the outcomes of a standardized treatment and rehabilitation strategy for managing patients undergoing initial unilateral transtibial amputation (TTA) due to peripheral vascular disease (PVD) (Figure 6) [32]. Between January 1, 1997, and December 31, 2006, a total of 217 consecutive patients from a well-defined population were enrolled. Prosthetic fitting was achieved in 119 patients (55%), with a mean age of 77 years, within a median time of 41 days (range: 12-147). Of those, 76 patients (64%) achieved good functional outcomes. The reamputation rate during the first year was 8.2%. Since the publication of this study, the standardized approach has seen increased adoption in most hospitals across Sweden [30].

Figure 6: The standardized process, from the left: Sagittal incision, Removable rigid dressing, Postop compression liner, and Direct socket.
The outcomes can be compared with data from the SwedeAmp register, which provides an annual report on lower limb amputations (LLA) in Sweden, including amputation levels, surgical techniques, time to prosthetic fitting, and other relevant metrics [30]. Currently, the register includes approximately 12,000 patients and 17,500 surgeries. The latest report highlights how surgical techniques in transtibial amputation can influence the time to prosthetic fitting. When the Sagittal/Skewed technique was used, the median time to prosthetic fitting was 54 days (range: 11-492), compared to 66 days (range: 16-376) with the Long Posterior Flap technique (p = 0.0011). This also impacts prosthetic fabrication methods. Direct socket fitting has become the dominant approach, significantly reducing the time to prosthetic fitting, with a median of 55 days (range: 14-418), compared to 199 days (range: 22-451) using traditional hand-casting methods, or 87 days (range: 19-355) with scanning methods.
To summarize, the SwedeAmp database register gives unique opportunities to analyze outcomes from a large population of those who have undergone LLA and are provided prostheses. The SwedeAmp registry offers an opportunity to review the longitudinal development of these procedures over time.
Discussion
In this paper, we have described the process of transtibial amputation from the Prosthetist perspective, commenting on the Surgeons' traditional performance and views on the postoperative treatment. These comments are based on Swedish sources (e.g., literature and SwedeAmp registry). The results and proposals may not be valid for all regions and settings, but they contribute to the evidence base used for decision-making following transtibial amputation.
The functional outcome of TTAs is superior compared with higher amputation levels and similar to partial foot amputations [13]. Rehabilitation has been considered successful in studies in the past if the patient had obtained regular daily use of their prosthesis for at least 6 months after prosthetic fitting and completing gait training. With an effective rehabilitation program, the likelihood of those who received transtibial prostheses being independent is high [10]. However, the presence of frailty in patients undergoing surgical intervention is associated with poorer outcomes concerning mortality and return to independence [46]. Mobility and prosthetic prescription are not only significant considerations for the younger population. For older adults with LLA, increased mobility is also highly associated with greater independence and a higher QOL, and age alone should not disqualify individuals from assessment or participation in an amputee rehabilitation program [46].
It is not realistic and may not always be beneficial for elderly patients who are at risk of amputation to be amputated at the transtibial level [47]. If these individuals with vascular disease had been considered "not walking" 3 months prior to the TTA, they are unlikely to be candidates for prosthetic fitting [32]. Although this level could be a potential healing level, the surgeons in these cases may want to consider performing a knee disarticulation instead, as the benefit of this surgical procedure is that it leaves remaining proximal skeletal and muscular structures largely intact [41]. This level provides a good opportunity for postural balance in seating with all the major thigh muscles intact. TTA level in these cases will include a higher risk of developing contractions in the knee joint and distal wound. The disadvantage of the KD, in this vulnerable population, is related to a higher risk for reamputation. If a TTA requires a reamputation, the KD level should not be selected due to higher risk of additional reamputation [47].
It could be questioned if we should discharge elderly patients with vascular disease who have undergone amputation from specialist care. The multidisciplinary or interdisciplinary management of the amputee is a forum that prosthetic users need to easily access to solve a minor problem related to the function of their remaining leg before it becomes a significant problem [9]. The Prosthetist should actively participate in the team collaboration to ensure proper fit and the greatest level of adherence [48]. Optimal outcomes need also be considered in light of the requirement to reducing costs of LLA. For this reason, one must consider that the total cost of TF, KD, and TT amputations in Sweden is estimated to currently be approximately $95,000 USD, and this statistic only covers acute care (not including prosthetic fitting and rehabilitation) [49]. When considering total surgical cost, prosthetic fitting and service for the following eight years represent 6% of this total [50]. If one wishes to lower the total cost, it seems reasonable that sufficient focus be placed on improving the acute care of those undergoing LLA, including standardizing the surgical method and the postoperative process, using the new technology available, and, most importantly, documenting the outcomes.
From the authors' view, when considering the Swedish context of modern postoperative treatment and prosthetic technology, registry data sems to suggest that SF incision may offer benefits over PF in TTA in the area of time to prosthetic fitting. New postoperative treatment methods are being made more accessible and recognized. However, further funding is required for the execution of well-designed studies related to amputation, including individuals over 65 years old, who, unfortunately, are often excluded from studies.
Conclusions
From a Prosthetist perspective, more could be done to improve the pathway from amputation to prosthetic fitting and ensure the best functional outcome for the patient. Traditional methods from the 1950s have been discussed, and alternatives have been presented.
References
- WHO standards for prosthetics and orthotics 2024.
- Allan CM, Campbell WN, Guptill CA, Stephenson FF, Campbell KE (2006) A conceptual model for interprofessional education: the international classification of functioning, disability and health (ICF). J Interprof Care 20: 235-245.
- Atlas of Amputations and Limb Deficiencies: Surgical, Prosthetic, and Rehabilitation Principles 2024.
- Almoajil H, Wilson N, Theologis T, Hopewell S, Toye F, et al. (2020) Outcome domains and measures after lower limb orthopaedic surgery for ambulant children with cerebral palsy: an updated scoping review. Dev Med Child Neurol 62: 1138-1146.
- Sabolich J (1996) You’re Not Alone: With the Stories of 38 Remarkable Amputees Who Conquered the Challenges of a Lifetime. Revised edition. Hanger Prosthetics & Orthotics 358.
- Johannesson A, Larsson GU, Oberg T (2004) From major amputation to prosthetic outcome: a prospective study of 190 patients in a defined population. Prosthet Orthot Int 28: 9-21.
- Fluss G, Greenspan J, Szczerepa D, Finlay DJ (2021) The optimal below knee amputation flap. Ann Vasc Surg - Brief Rep Innov 1: 100003.
- Larsson GU, Johannesson AG (2024) The Sagittal Incision in Transtibial Amputation-Including the Postoperative Treatment 8.
- Cater C (2026) Physiopedia. 2026 [cited 2024 Feb 16]. Multidisciplinary and Interdisciplinary Management of the Amputee 2026.
- Stineman MG, Kwong PL, Xie D, Kurichi JE, Ripley DC, et al. (2010) Prognostic differences for functional recovery after major lower limb amputation: effects of the timing and type of inpatient rehabilitation services in the Veterans Health Administration. PMR 2: 232-243.
- Miller TA, Paul R, Forthofer M, Wurdeman SR (2023) Factors that influence time to prosthesis receipt after lower limb amputation: A Cox proportional hazard model regression. PM&R 15: 474-481.
- Marsden FW (1977) Amputation: surgical technique and postoperative management. Aust N Z J Surg. 1977 Jun 1977: 384-392.
- Quigley M, Dillon MP (2016) Quality of life in persons with partial foot or transtibial amputation: A systematic review. Prosthet Orthot Int 40: 18-30.
- Crenshaw A, Tooms RE (1992) Campbell’s operative orthopaedics. Vol. 2. Mosby-Year Book 1992: 689-702.
- Persson BM, Liedberg E (1983) A clinical standard of stump measurement and classification in lower limb amputees. Prosthet Orthot Int 7: 17-24.
- Bowker JH, Michael JW (1992) American Academy of Orthopaedic Surgeons, editors. Atlas of limb prosthetics: surgical, prosthetic, and rehabilitation principles. 2nd ed. St. Louis: Mosby Year Book 1992: 930.
- Ibarra Aguila S, Sánchez GJ, Sauvain EE, Alemon B, Fuentes-Aguilar RQ, et al. (2020) Interface Pressure System to Compare the Functional Performance of Prosthetic Sockets during the Gait in People with Trans-Tibial Amputation. Sensors 20: 7043.
- Firth GB, Masquijo JJ, Kontio K (2011) Transtibial Ertl amputation for children and adolescents: A case series and literature review. J Child Orthop 5: 357-362.
- Eshraghi A, Osman NAA, Gholizadeh H, Karimi M, Ali S (2012) Pistoning assessment in lower limb prosthetic sockets. Prosthet Orthot Int 36: 15.
- Editor DT (2020) Below Knee Amputation. Wheeless’ Textbook of Orthopaedics 2020.
- Brückner L (1992) A standardised trans-tibial amputation method following chronic occlusive arterial disease. Prosthet Orthot Int 16: 157-162.
- Burgess EM, Zettl JH (1969) Amputations below the knee. Artif Limbs 13: 1-12.
- Nawijn SE, van der Linde H, Emmelot CH, Hofstad CJ (2005) Stump management after trans-tibial amputation: a systematic review. Prosthet Orthot Int 29: 13-26.
- Sewell P, Noroozi S, Vinney J, Andrews S (2000) Developments in the trans-tibial prosthetic socket fitting process: a review of past and present research. Prosthet Orthot Int 24: 97-107.
- Burgess EM, Romano RL, Zettl JH, Schrock RD (1971) Amputations of the leg for peripheral vascular insufficiency. J Bone Joint Surg Am 53: 874-890.
- Lilja M, Johansson T, Oberg T (1993) Movement of the tibial end in a PTB prosthesis socket: a sagittal X-ray study of the PTB prosthesis. Prosthet Orthot Int 17: 21-26.
- Levy SW (1995) Amputees: skin problems and prostheses. Cutis 55: 297-301.
- Robinson KP (1991) Skew-flap below-knee amputation. Ann R Coll Surg Engl 73: 155-157.
- Jesani L, Gwilym B, Germain S, Jesani H, Stimpson A, et al. (2020) Early and Long Term Outcomes Following Long Posterior Flap vs. Skew Flap for Below Knee Amputations. Eur J Vasc Endovasc Surg 60: 301-308.
- SwedeAmp registery. Årsrapport 2022.
- Persson BM (1974) Sagittal incision for below-knee amputation in ischaemic gangrene. J Bone Joint Surg Br 56: 110-114.
- Johannesson A, Larsson GU, Ramstrand N, Lauge-Pedersen H, Wagner P, et al. (2010) Outcomes of a Standardized Surgical and Rehabilitation Program in Transtibial Amputation for Peripheral Vascular Disease: A Prospective Cohort Study. Am J Phys Med Rehabil 89: 293-303.
- General Principles of Amputation Surgery 2024.
- Lilja M, Hoffmann P, Oberg T (1998) Morphological changes during early trans-tibial prosthetic fitting. Prosthet Orthot Int 22: 115-122.
- Tisi PV, Than MM (2014) Type of incision for below knee amputation. Cochrane Database Syst Rev 2014: CD003749.
- Termansen NB (1977) Below-knee amputation for ischaemic gangrene. Prospective, randomized comparison of a transverse and a sagittal operative technique. Acta Orthop Scand 48: 311-316.
- Paterno L, Ibrahimi M, Gruppioni E, Menciassi A, Ricotti L (2018) Sockets for Limb Prostheses: A Review of Existing Technologies and Open Challenges. IEEE Trans Biomed Eng 65: 1996-2010.
- Jain SK (2005) Skew flap technique in trans-tibial amputation. Prosthet Orthot Int 29: 283.
- Kamrad I, Söderberg B, Örneholm H, Hagberg K (2020) SwedeAmp-the Swedish Amputation and Prosthetics Registry: 8-year data on 5762 patients with lower limb amputation show sex differences in amputation level and in patient-reported outcome. Acta Orthop 91: 464-470.
- Churilov I, Churilov L, Murphy D (2014) Do rigid dressings reduce the time from amputation to prosthetic fitting? A systematic review and meta-analysis. Ann Vasc Surg 28: 1801-1808.
- Fard B, Persoon S, Jutte PC, Daemen JWHC, Lamprou DA, et al. (2023) Amputation and prosthetics of the lower extremity: The 2020 Dutch evidence-based multidisciplinary guideline. Prosthet Orthot Int 47: 69-80.
- Johannesson A, Larsson GU, Oberg T, Atroshi I (2008) Comparison of vacuum-formed removable rigid dressing with conventional rigid dressing after transtibial amputation: similar outcome in a randomized controlled trial involving 27 patients. Acta Orthop 79: 361-369.
- Coulston JE, Tuff V, Twine CP, Chester JF, Eyers PS, et al. (2012) Surgical factors in the prevention of infection following major lower limb amputation. Eur J Vasc Endovasc Surg Off J Eur Soc Vasc Surg 43: 556-560.
- Gholizadeh H, Abu Osman NA, Eshraghi A, Arifin N, Chung TY (2016) A comparison of pressure distributions between two types of sockets in a bulbous stump. Prosthet Orthot Int 40: 509-516.
- Socket Fabrication Directly on Residual Limb. Ossur.com 2024.
- Oakland K, Nadler R, Cresswell L, Jackson D, Coughlin PA (2016) Systematic review and meta-analysis of the association between frailty and outcome in surgical patients. Ann R Coll Surg Engl 98: 80-85.
- Sjödin LS, Ottosson CC, Lapidus LJ (2024) Knee disarticulation vs. transfemoral amputation after failed transtibial amputation: Surgical outcome and prosthetic fitting in patients with peripheral vascular disease. Prosthet Orthot Int 48: 25-29.
- Salawu A, Middleton C, Gilbertson A, Kodavali K, Neumann V (2006) Stump Ulcers and Continued Prosthetic Limb Use. Prosthet Orthot Int 30: 279-285.
- Eneroth M, Apelqvist J, Troëng T, Persson BM (1996) Operations, total hospital stay and costs of critical leg ischemia. A population-based longitudinal outcome study of 321 patients. Acta Orthop Scand 67: 459-465.
- Hermodsson Y, Persson BM (1998) Cost of prostheses in patients with unilateral transtibial amputation for vascular disease. A population-based follow-up during 8 years of 112 patients. Acta Orthop Scand 69: 603-607.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.