Progressive Pseudorheumatoid Dysplasia, A close mimicker of Juvenile Idiopathic Arthritis
by Saad Mohammad1, Duaa Mohamed1, Maryam AlShehhi2, Shyam Mohan3, Ayesha AlMheiri4*
1Department of Pediatrics, Education institute Pediatric Residency Program, Sheikh Khalifa Medical City, Al Karama Street, Abu Dhabi, UAE
2Department of Pediatrics, Division of Genetics, Sheikh Khalifa Medical City, Al Karama Street, Abu Dhabi, UAE
3Department of Pediatrics, Division of Radiology, Sheikh Khalifa Medical City, Al Karama Street, Abu Dhabi, UAE
4Department of Pediatrics, Division of Rheumatology, Sheikh Khalifa Medical City, Al Karama Street, Abu Dhabi, UAE
*Corresponding author: Ayesha AlMheiri, Consultant Pediatric Rheumatologist, Sheikh Khalifa Medical City, Al Karama Street, Abu Dhabi, UAE
Received Date: 19 July 2024
Accepted Date: 23 July 2024
Published Date: 25 July 2024
Citation: Mohammad S, Mohamed D, Alshehhi M, Mohan S, AlMheiri A (2024) Progressive Pseudorheumatoid Dysplasia, A close mimicker of Juvenile Idiopathic Arthritis. Ann Case Report. 9: 1903. https://doi.org/10.29011/2574-7754.101903
Abstract
Progressive pseudorheumatoid dysplasia is a rare, autosomal recessively inherited, noninflammatory musculoskeletal disorder. Joint cartilage is the primary site of involvement the incidence of PPRD is one per million in the United Kingdom. The clinical manifestations of juvenile idiopathic arthritis are similar to those of progressive pseudorheumatoid dysplasia. Most often, patients with progressing pseudorheumatoid dysplasia are misdiagnosed as having juvenile idiopathic arthritis.
A 15-year-old Egyptian male presented to the rheumatology clinic with a history of stiffness, pain and swelling in multiple joints, limitation of daily activity of 7 years. Was diagnosed with JIA that was treated with Cortisol and Rituximab but with poor response. The patient was having abnormal gait, there was none tender swelling of knee joints, metacarpophalangeal and interphalangeal joints.
Labs including inflammatory markers, Rheumatological workup, were inconclusive. Whole exome sequencing result showed: A homozygous likely pathogenic variant was identified in the CCN6 gene. This result is consistent with the genetic diagnosis of autosomal recessive Progressive pseudorheumatoid dysplasia.
The similar presentation between this entity and JIA makes the diagnosis of Progressive pseudo rheumatoid dysplasia challenging. When 1st line treatment doesn’t cause improvement in patient clinical situation, always think about alternative diagnosis.
Although the differentiation between JIA and Progressive pseudo rheumatoid dysplasia is challenging based on clinical presentation and physical Examination, Radiological finding can help. The absence of inflammatory joint disease and platyspondyly and generalized epiphyseal dysplasia in Radiological findings with a normal inflammatory marker makes the diagnosis of Progressive pseudo rheumatoid dysplasia superior to JIA.
Keywords: Progressive Pseudorheumatoid Dysplasia; Juvenile Idiopathic Arthritis; Inflammatory Arthritis; Pediatrics Rheumatology.
Abbreviations: PPRD: progressive pseudorheumatoid dysplasia; JIA: Juvenile Idiopathic Arthritis; MRI : Magnetic resonance imaging; CRP: C reactive protein; ESR: Erythrocyte sedimentation Rate; RF: Rheumatoid factor; Anti-CCP: anti-citrullinated peptides antibodies; anti-dsDNA: anti-double stranded DNA; ANA: antinuclear antibody; NSAIDS: Non-Steroidal anti-inflammatory drugs; CCN6: cellular communication network factor 6; WNT1: Wingless-related integration site; AP: Anteroposterior; STIR: Short tau inversion recovery.
Introduction
Progressive Pseudorheumatoid dysplasia (PPRD) is a rare skeletal dysplasia characterized by predominant involvement of articular cartilage with progressive joint stiffness and enlargement in the absence of inflammation [1]. It is inherited in an autosomal recessive pattern and caused by mutations occurring in the WNT1-inducible signalling pathway protein 3 gene. Even though this illness has a significant arthropathy, pain is not one of its main presenting characteristics. The diagnosis of PPRD is established in a proband with characteristic radiographic features and/or identification of biallelic pathogenic variants in CCN6 on molecular genetic testing [1]. WISP3 is essential in maintaining cartilage integrity by regulating the expression of type II collagen and aggrecan in chondrocytes [2]. It is believed that PPRD is more prevalent in Turkey and Middle East population although the incidence is unknown. In UK, the prevalence is estimated to be 1 per million [3]. The clinical manifestations of juvenile idiopathic arthritis are similar to those of progressive pseudorheumatoid dysplasia. Most often, patients with progressing pseudorheumatoid dysplasia are misdiagnosed as having juvenile idiopathic arthritis.Herein, we present a case of a 15-year-old boy who was earlier diagnosed with poly-articular Juvenile Idiopathic arthritis and subsequently diagnosed with PPRD with characteristic signs and symptoms development.
Case Presentation
A 15-year-old Egyptian boy who was referred for admission from the rheumatology clinic with a previously diagnosis of JIA. His development and growth were normal during his first few years of life. However, at the age of four he was noticed to have an abnormal gait, he was evaluated in his home country and given vitamin D and calcium supplements in addition to occasional ibuprofen for pain relief. The assessment revealed no cause for concern. Then he started developing swelling in his fingers, elbows, and knees, he was assessed by a pediatric rheumatologist who diagnosed the child with JIA and prescribed steroids and methotrexate, but with no significant improvement.
Over time, his condition worsened, resulting in increased joint restrictions, discomfort, and stiffness in the morning. He began to have deteriorated lower back, hip, and knee pain a few months ago. This pain was accompanied by morning stiffness lasting more than thirty minutes. He eventually lost the ability to move, including the ability to stand or walk, and he developed hip flexion, which prevented him from extending his hip because of pain and limitation. Due to the advancement of his condition, he has not attended school for the past two years. He is now confined to his chair all the time and needs assistance with everyday tasks. He is underweight. He has no fever, rash, headaches, eye symptoms, mouth ulcer, chest pain, breathing issues, gastrointestinal symptoms, hair loss, or fatigue.
He was born to first-degree healthy cousins, and has 4 healthy older siblings. He has two maternal cousins with similar complaints who have been diagnosed with Rheumatoid Arthritis but are not receiving any medication other than calcium and vitamin D. No history of any other autoimmune diseases.
Physical Examination
He looked generally well with normal vitals. Growth chart showed he is underweight with a weight of 35kg and has short stature with his height being 115cm, both below the third centile. His musculoskeletal assessment revealed marked swelling of proximal and distal interphalangeal joints bilaterally (Figure 1) with mild tenderness, he has significant restrictions in both wrists, both elbows, and in both shoulders. Lower limb examination showed restriction of movement and stiffness of the hips and knees, there was no signs of inflammation in both joints (Figure 2). Upon assessing the gait of the patient, he had significant kyphoscoliosis (Figure 3). His rest of other systems examination were unremarkable.
Investigations
Erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), Rheumatoid factor (RF), anti-citrullinated peptides antibodies (Anti-CCP), anti-double stranded DNA (anti-dsDNA), antinuclear antibody (ANA) and HLA-B27 typing all negative and are not suggestive of inflammatory arthritis. Workup up for extra-articular involvement done including ophthalmic exams and ECHO were all unremarkable. Radiological findings showed significant changes. There was marked loss of joint space affecting multiple joints in the body with variable degree of involvement. There was involvement of both small and large joints. There was no signs of active arthritis is these joints, and most of the changes was representing chronic changes, and complications of chronic inflammation (Figures 4-7). Other imaging modality was done to assess the degree of joints involvement. The significant finding was the spine involvement. MRI of the spine showed changes that is unusual to be seen in common causes of arthritis in pediatrics such as JIA, there was spine deformity and changes involving the vertebra (Figures 8,9). Based on history, clinical and imaging findings, laboratory results, the diagnosis Progressive pseudorheumatoid dysplasia (PPRD) was suspected and Whole exome sequencing sent that revealed: A homozygous likely pathogenic variant was identified in the CCN6 gene, which confirmed the diagnosis. During his stay he started on Zoledronic acid for osteopenia, he was undergoing daily physiotherapy and occupational therapy.The patient’s joint pain was alleviated and joint motion improvement was obvious after treatment and he discharged home on a walking frame which have improved his range of motion and his pain.

Figure 1: Swelling of the proximal and Distal interphalangeal Joints with restriction of movement.

Figure 2: Legs remained flexed, with significant restriction on the hips and knees.

Figure 3: Spine has kyphoscoliosis.

Figure 4: AP radiograph of the left hand shows marked loss of joint space affecting the radiocarpal, inter-carpal and inter-phalangeal joints.

Figure 5: AP radiograph of both elbows showing loss of joint space, osteophyte formation.
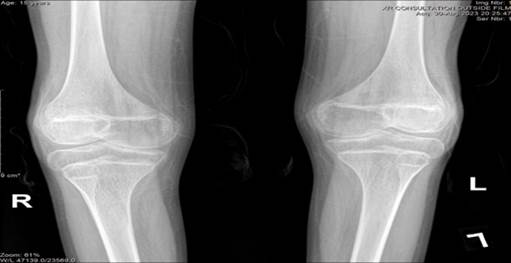
Figure 6: AP radiograph of both knees showing joint space loss that is more marked in the medial compartment. Medial condylar enlargement is also seen, possibly from long standing hyperemia.

Figure 7: AP radiograph of the pelvis showing marked joint space loss in the hip joints bilaterally with features of secondary osteoarthritis including osteophytosis and subchondral cyst formation.

Figure 8: Axial STIR image showing complete loss of cartilage signal in the hip joints, with bone abutting bone and subchondral edema.
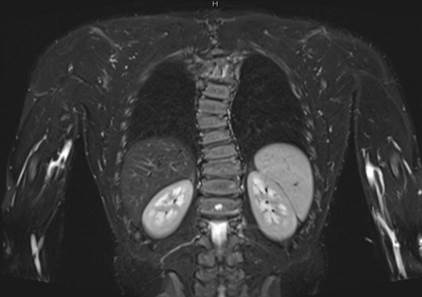
Figure 9: Coronal STIR image of spine MRI showing vertebral body flattening (arrows) and focal scoliosis. These are features that are not usually seen with JIA.
Discussion
PPRD is a rare autosomal recessive dysplasia. With an incidence of one per million in the United Kingdom (prevalence category of <1-9:1,000,000) [1]. The main feature of PPRD is the gradual stiffness and expansion of the joints, primarily affecting the articular cartilage, without any associated inflammation. It first manifests clinically in children between the ages of three and six, affecting the interphalangeal joints. Over time, it affects the large joints and the spine, resulting in significant joint contractures, abnormal gait, scoliosis, or kyphosis, which leads to abnormal posture and significant morbidity [2]. Although this condition is often misdiagnosed as juvenile idiopathic arthritis, it can be identified by radiographic examination, which highlights the absence of inflammatory joint disease and platyspondyly and generalized epiphyseal dysplasia with a normal inflammatory marker unlike what is seen in JIA in which there is an elevated CRP and ESR. Other differential feature between PPRD and JIA is that in JIA, joint destruction is seen on radiographs. While in PPRD, radiographs show dysplasia along with epiphyseal enlargement and platyspondyly [1]. Investigations for PPRD include normal erythrocyte sedimentation rate and C-reactive protein levels with radiologic featuresinclude spondyloepiphyseal dysplasia, generalized arthropathy, distinctive joint deformity of the hands (superficially resembling that of juvenileidiopathicarthritis), and diffuse osteoporosis at the late stage [1,4]. Diagnosis is confirmed genetically via identifying pathogenic variant in CCN6 gene. Management of PPRD is supportive. Analgesics mainly NSAIDS can help with pain. In some cases orthopedics procedure including joint arthroplasty can be done. Physiotherapy and occupational therapy are a cornerstone in supporting the patients and reducing the joints stiffness and improve the overall daily living for the patients. Orthopedic procedures for spine abnormalities like scoliosis and kyphosis can also be done if indicated. Life span for these patients is not affected however due to the progressive nature of the disease and lack of cure, patients eventually develop major limitations in their daily living and physical and psychosocial morbidity.
Conclusion
PPRD is a rare progressive skeletal condition that is usually misdiagnosed as JIA. Our patient continued to experience progressive joint stiffness, discomfort, edema, and limited mobility even after starting JIA medications. Genetic testing revealed his homozygous pathogenic mutation in the CCN6 gene, which led to the diagnosis of PPRD. PPRD needs to be considered as one of the differentials in JIA patients who are not responding to usual treatments.
Acknowledgements: I extend my deepest thanks to Dr. Ayesha Al Muhairi for her supervision and unstopped support. Further appreciation to Dr. Maryam AlShehhi, Dr. Shyam Mohan, and Dr. Duaa Mohamed for their collaborative efforts. I would also like to thank Pediatrics Department at Sheikh Khalifa medical City for their support and constructive feedback.
Conflict of Interest Disclosures: The authors have no conflicts of interest relevant to this article to disclose.
References
- Bhavani GS, Shah H, Shukla A, Dalal A, Girisha KM (2020) Progressive Pseudorheumatoid Dysplasia. GeneReviews® - NCBI Bookshelf.
- Omar A, Ahmed S, Rodrigues J, Kayiza A, Owino L. (2021) Progressive pseudorheumatoid dysplasia misdiagnosed as juvenile idiopathic arthritis: a case report. Journal of Medical Case Reports; BioMed Central, 15: 551.
- Giray E, Yağcı İ, Elçioğlu HN (2019) Progressive pseudorheumotoid dysplasia: A presentation of four cases with slow and rapid progression and effects of early rehabilitation program. Turk J Phys Med Rehabil. 65: 290-297.
- Alexander (2022) GARD Rare Disease Information - Progressive pseudorheumatoid dysplasia - National Organization for Rare. National Organization for Rare Disorders.
© by the Authors & Gavin Publishers. This is an Open Access Journal Article Published Under Attribution-Share Alike CC BY-SA: Creative Commons Attribution-Share Alike 4.0 International License. Read More About Open Access Policy.